DKA - British Society for Paediatric Endocrinology and Diabetes
advertisement

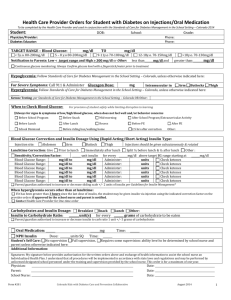
Insert Trust Logo Integrated Care Pathway for Children and Young People with Diabetic Ketoacidosis (DKA) This Integrated Care Pathway was developed by the Southwest Paediatric Diabetes Regional Network as a bedside tool to aid care and documentation. It forms the official care record, so file in patient notes. It is based on Guidelines of NICE 2004, British Society of Paediatric Endocrinology and Diabetes 2009. Young Adults are also at risk of Cerebral Oedema - we recommend this guideline up to age 25 years. All interventions must be documented and signed. Write your name clearly next to your signature. Any deviation from the care plan must be documented. If you are not experienced in managing children in DKA, ask for senior help now. PATIENT DETAILS: Patient identification sticker: ADMISSION DATE: NAME: ADMISSION TIME: ADMISSION SOURCE: HOSPITAL NUMBER: ABBREVIATIONS USED BP Blood Pressure ENT Ear, Nose and Throat K Potassium CNS Central Nervous System FBC Full blood count KCl Potassium Chloride CRP C-reactive protein HbA1c Glycosylated Hb MSU Mid-stream urine CRT Capillary Refill Time HCO3 Bicarbonate Na Sodium CSF Cerebrospinal fluid HDU High Dependency Unit NG tube Nasogastric Tube CXR Chest X-ray ITU Intensive Therapy Unit PICU Paediatric Intensive Care Unit ECG Electrocardiogram IV Intravenous U+Es Urea and Electrolytes GLASGOW COMA SCALE (GCS) Maximum score 15, minimum score 3 Best Best 1 = none 1 = none Modification (2-5yrs) Motor 2 = extensor response to pain Verbal 2 = incomprehensible sounds 1 = none Response 3 = abnormal flexion to pain Response 3 = inappropriate words 2 = grunts 4 = withdraws from pain 4 = appropriate words but confused 3 = cries or screams 5 = localises pain 5 = fully orientated 4 = monosyllables 6 = responds to commands Modification (<2yrs) 5 = words of any sort 1 = none Eye 1 = none 2 = grunts Opening 2 = to pain 3 = inappropriate crying/unstimulated screaming 3 = to speech 4 = cries only 4 = spontaneous 5 = appropriate non-verbal responses (coos, smiles, cries) R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 1 Insert Trust Logo Algorithm for DKA History Signs - polyuria - polydipsia - weight loss - abdominal pain - lethargy - vomiting - confusion - assess % dehydration - deep sighing respiration (Kussmaul) - smell of ketones - lethargy, drowsiness Biochemistry - elevated blood glucose >11mmol/l - acidaemia: pH<7.3, Bicarbonate <15 - ketones in blood or urine - check U + Es, Creatinine - other tests as indicated Confirm Diagnosis Diabetic Ketoacidosis Call Senior Staff Shock Reduced conscious level Dehydration > 3% Clinically acidotic Vomiting Dehydration < 3% Clinically well Tolerating fluid orally Intravenous therapy Resuscitation - calculate fluid requirements - correct over 48 hours - 0.9% saline for at least first 12 hours - add KCl 20mmol per 500ml bag - 1 hour after IV fluids commenced, start Insulin infusion 0.1U/kg/hour - Airway + NG tube - Breathing (100% 02) - Circulation (slow bolus 10ml/kg IV 0.9% saline, repeated until circulation restored - further doses rarely needed, maximum 3 doses) Subcutaneous Therapy - start with subcut insulin - give oral fluids No improvement Ketones rising Looks unwell Starts vomiting Observations - hourly blood glucose - neurological status at least hourly - hourly fluid input:output chart - U+Es & blood gas 2 hours after start of IV therapy, then 4-hourly - 2-4 hourly blood ketone levels if available, or dip test every urine for ketones No improvement Re-evaluate: - fluid balance & IV therapy - if continued acidosis, may require further resuscitation fluid - check insulin dose correct - consider sepsis, on-going fluid losses Subcutaneous Insulin Start s/c Insulin then stop IV Insulin infusion 1 hour later (or after 10 minutes if starting rapid acting analogs – see p 8) Neurological deterioration Warning signs: Headache, irritability, slowing heart rate, reduced conscious level, specific signs raised intra-cranial pressure Blood glucose falls <14 mmol/L ? Exclude hypoglycaemia Is it cerebral oedema? Intravenous therapy - During initial 12 hours: use 0.9% saline 5% glucose - After 12 hours: change to 0.45% saline/ 5% glucose - ensure KCl 20mmol/500ml bag - continue monitoring as above - consider reducing Insulin 0.05U/kg/hour, only when pH>7.30 and/or Bicarbonate >15 Resolution of DKA - Clinically well, drinking well, tolerating food - Blood ketones < 1.0 mmol/L or pH or bicarb normal - Urine ketones falling (but may still be positive) R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Management - secure airway, 100% 02 - head-up tilt to bed - 2.7% Saline 3 ml/kg IV or Mannitol 0.5 -1.0 g/kg IV - call senior staff - restrict IV fluids by 50% - move to ITU / PICU - CT scan when stabilised Page 2 Patient details or hospital sticker: Insert Trust Logo RAPID ASSESSMENT (fill all boxes) Airway Patent? Breathing Resp rate / min O2 Saturation % Circulation Pulse /min Central CRT seconds Shock? Y/N GCS % 3% 5% 8% / 15 (see front sheet) AVPU Urinalysis BP / Just clinically detectable Dry mucous membranes, reduced skin turgor As above + sunken eyes + prolonged CRT or (Alert, Responds to Voice, or Pain, or Unresponsive) Signs of cerebral oedema? Y / N Initial bloods Acidotic pattern? Y / N Y/N Dehydration Disability (neuro) (if drowsy/coma: NG tube) (headache, irritable, drowsy, focal neurology, low pulse, high BP, papilloedema) see p5 Arterial / Venous / Capillary (circle) pH Bicarbonate Bedside glucose Blood ketones Ketones Glycosuria if available (superior to urine ketones) MANAGE USING THIS DKA PATHWAY IF: Blood glucose > 11mmol/l, and pH <7.30/HCO3 <15, particularly if vomiting and/or drowsy HYPERGLYCAEMIA WITHOUT THESE FEATURES: Usually managed with subcutaneous insulin - do not use this pathway, see your local protocol. If unsure, discuss with consultant. If any of the following present, consider local ITU/Bristol PICU: ▪ pH<7.1 with marked hyperventilation ▪ severe dehydration with shock ▪ depressed conscious level ▪ age <2years If very high glucose (eg >50mmol/l) think of Hyperglycaemic Hyperosmolar State (HHS) Calculate osmolality by: 2(Na + K) + Gluc + Urea. Normal 280-295mOsm/l; If > 340mOsm/l, seek expert advice. RECORD MANAGEMENT DECISION (circle): Clinical plan: Admit to: For DKA: Consultant informed? If 'No' record why: DKA pathway or subcut insulin Ward or HDU/ITU or PICU Y/N Signed: ___________________ R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 3 Insert Trust Logo HISTORY & EXAMINATION (if ill, resuscitate first - page 5) HISTORY (use extra sheets as needed) Polyuria? Polydipsia? Weight loss? Vomiting/Abdominal pain? Headache? Infection? Other symptoms: Drug history Usual insulin regime: Adherence? Other medications: Allergies: Family & Social history Past medical history EXAMINATION (additional to RAPID ASSESSMENT above) General status: Cardiovascular: Respiratory/ENT: Abdomen: CNS: Signed: ____________ MANDATORY INVESTIGATIONS For newly diagnosed patient, add: BLOOD KETONES (if available) Thyroid function URINE KETONES (if not) Thyroid antibodies BLOOD GAS Coeliac screen VENOUS LAB GLUCOSE HbA1c U&Es, CREATININE If clinical suspicion of infection, consider: FBC, CRP, urine culture, blood culture, CXR, Throat swab, Lumbar puncture Signed: ____________ R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 4 Patient details or hospital sticker: Insert Trust Logo DKA MANAGEMENT 1. RESUSCITATION If patient very ill (drowsy, shocked, marked hyperventilation), call for senior help immediately A Establish airway B Give O2 100% via face mask with reservoir bag C Establish IV access, take initial bloods (consider 2nd cannula for later samples) Cardiac monitoring (peaked T waves may indicate hyperkalaemia) If coma, insert NG tube, free drainage ► If prolonged CRT plus other signs of shock, give 10ml/kg IV 0.9% Saline. Assess effect. More than one fluid bolus rarely needed. ► If circulation not improved, can give 2nd and (rarely) 3rd bolus (each over 30 mins) ie maximum total 30ml/kg - if shock persists, consult senior paediatrician & inform ITU/PICU WEIGHT: Actual kg Estimated kg or Recent clinic weight kg (date: ______ ) or If too ill to weigh, estimate: 1 - 10 years: Weight (kg) = 2 (Age + 4) >10 years: Use 50th centile weight on growth chart [If recent clinic weight and weight at presentation known, use these to estimate % dehydration] Record Resuscitation Fluid Volume Given: D ml Consider CEREBRAL OEDEMA (at presentation, or may develop in first 12 hours) If drowsy/coma, nurse in HDU/ITU/PICU Headaches? Irritability/drowsiness? Convulsions? Focal neurological signs? Abnormal posturing? Falling GCS? Rising BP, falling pulse? Papilloedema? Poor respiratory effort? Falling O2 saturations? Signed: ____________ CEREBRAL OEDEMA: This is the major cause of severe morbidity/mortality in childhood DKA. Often develops within 12 hours of starting treatment, may already be present before treatment. Risk factors: raised urea, raised PaCO2, >40ml/kg resus fluids within first 4 hours. Management: Inform senior staff immediately Check blood glucose (exclude hypoglycaemia as cause of neurological signs/symptoms) Secure airway, give 100% O2 Hypertonic 2.7% Saline (3ml/kg IV over 30 mins), or Mannitol 0.5-1g/kg (2.5-5ml/kg 20% solution IV over 20 mins). Give as soon as possible if warning signs occur. Transfer to PICU Recalculate IV fluid: Use 50% of usual maintenance requirement; replace deficit over 72 not 48 hours When stable, arrange CT scan to exclude other causes of deterioration (not to confirm oedema) Document all events with dates and times R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 5 Insert Trust Logo 2. INITIAL TREATMENT WEIGHT CAUTION! ▪ Overrapid or excessive fluids may increase risk of cerebral oedema ▪ Don't overestimate degree of dehydration (never use >8% for calculations) ▪ Aim to rehydrate slowly over 48 hours, not 24 hours FLUID VOLUME 1. Maintenance fluids in DKA 0 – 12.9 kg 13 – 19.9 kg 20 – 34.9 kg 35 – 59.9 kg >60 kg (or adult) 80 ml/kg/24hrs 65 ml/kg/24hrs 55 ml/kg/24hrs 45 ml/kg/24hrs 35 ml/kg/24hrs Note 1: APLS maintenance fluid rates over-estimate requirement. Don't use them in DKA. Note 2: Neonatal DKA requires special consideration and larger volumes of fluid may be needed, usually 100-150 ml/kg/24 hours. 2. Dehydration deficit (i.e. 3, 5 or 8%) % dehydration x weight (kg) x 10 = fluid deficit (ml) (e.g. 10 kg child who is 5% dehydrated : 5 x 10 x 10 = 500 mls deficit) 3. Fluid requirement for 48hrs = Maintenance for 48hrs + Deficit - Resus Fluids Add maintenance for 48 hours (2 x daily maintenance) to calculated deficit; subtract volume of resuscitation fluid already given; then infuse over 48 hours. i.e. Hourly rate (ml/hour) = 48 hour maintenance (ml) + deficit (ml) - resuscitation fluid already given (ml) 48 Do not include continuing urinary losses in calculations at this stage RECORD FLUID CALCULATION HERE: 1. Maintenance for 48 hours (2 x daily maintenance, above) PLUS 2. Deficit (% dehydration x weight (kg) x 10) ml + ml = ml - ml 3. Fluid to be given in next 48 hours = ml ...divided by 48 to give hourly rate = ml/hour MINUS Volume of resuscitation fluids already given Or for calculating fluid rates, can use this link Fluid Calculator and print out for child’s medical records Signed _______________ INITIAL FLUID TYPE Start with 0.9% Saline + 20mmol KCl/500ml. Only omit KCl if anuric at presentation, or peaked T waves - await urgent U+E result. There is always massive total body potassium depletion, although initial plasma levels may be low, normal or even high. Potassium moves rapidly into cells with rehydration and insulin, so levels will fall. Therefore KCl must be added from the start and continued. More than 20mmol KCl /500ml is sometimes needed. Continue 0.9% Saline + 20mmol KCl/500ml (with extra glucose if required) for at least 12 hours. (i.e. do not switch to 0.45% Saline/5% glucose within first 12 hours). See p8 for Ongoing fluid management, including action required when glucose falls <14mmol/l R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 6 Patient details or hospital sticker: Insert Trust Logo INSULIN Do not give insulin bolus. Insulin can be run via same cannula as fluids, using Y-connector. Allow 1 hour of IV fluids before starting insulin (may reduce cerebral oedema risk) Insulin infusion: 50 units Actrapid (or other rapid-acting insulin) in 50ml 0.9% Saline Infusion rate: 0.1 ml/kg/hour ( = 0.1 units/kg/hour) This rate is required to switch off ketone production and improve pH. Aim to maintain this rate (may need to add dextrose to IV fluids, p8), until pH>7.3, HCO3 >15 mmol/L (Some clinicians prefer 0.05 units/kg/hour in very young patients, although no firm evidence to support this) Patients with pre-existing diabetes: If on long-acting insulin (especially Glargine (Lantus)) - local consultant may want this to continue at usual dose and time during DKA treatment, in addition to IV insulin infusion, to shorten length of stay. If on insulin pump therapy, stop the pump when starting DKA treatment. 3. ONGOING MANAGEMENT PRINCIPLES Aim to rehydrate, correct pH & electrolyte disturbances and blood glucose slowly Reassess patient frequently, specifically watching for signs of CEREBRAL OEDEMA Pay strict attention to fluid balance and electrolyte management NURSING Consider PICU/HDU if: pH<7.1 with marked hyperventilation, severe dehydration with shock, depressed consciousness, age <2years, or if staffing levels insufficient to allow adequate monitoring. If no PICU/HDU within admitting hospital, transfer to another hospital for such care may not be appropriate (unless ventilatory support necessary). However, all children with DKA are high-dependency patients and need high level of nursing care, usually 1:1, even if on general wards. Ongoing: Hourly fluid balance sheet Hourly vital signs AND neuro obs Cardiac monitor (observe for T wave changes) Hourly capillary blood glucose 2-4 hourly capillary blood ketone levels* Test every urine for ketones Twice daily weight (if available) (if blood ketones not available) Consider urinary catheter (in young/very sick) If consciousness reduced - NG tube, free drainage until child conscious * Use near-patient ketone testing to confirm that levels are falling. If ketones not falling, check infusion lines, insulin dose and calculation - consider giving more insulin. Consider sepsis, inadequate fluid input and other causes if sufficient insulin is being given. INFORM MEDICAL STAFF IMMEDIATELY IF: Any change in consciousness (GCS)/behaviour, or headache/slowing heart rate/rising BP Any ECG changes (watch for peaked T waves) Urine output poor (<1.5ml/kg/hour) or excessive (>2.5ml/kg/hour) If marked rise in blood glucose e.g. >5 mmols/L in 1 hr, check calculations, insulin infusion; possibly remake infusion, re-evaluate for sepsis. REPEAT BLOOD TESTS & GASES Repeat 2 hours after starting resuscitation, and 4 hourly thereafter until acidosis resolved and electrolytes normal. Record all results on flow sheet, p9. R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 7 Insert Trust Logo ONGOING INSULIN & IV FLUID AND ELECTROLYTE MANAGEMENT Ensure each 500ml fluid bag contains 20mmol KCl (40mmol/litre) unless anuric or peaked T waves. Alter potassium replacement according to U&Es. More potassium than 40 mmol/L occasionally required. Falling Glucose level Addition of glucose to IV fluids is required when glucose falls <14mmol/L. (Some suggest adding glucose even before this if the initial rate of fall of blood glucose is greater than 5-8 mmol/l per hour, but there is no good evidence for this, and blood glucose levels will often fall quickly purely because of rehydration.) When glucose falls <14mmols/L, add glucose to IV fluids as follows (don't reduce insulin infusion): If within first 12 hours Continue 0.9% Saline/KCl as patient still sodium-depleted, but add glucose. Bags of 500ml 0.9% Saline / 5% glucose + 20 mmol KCl should be available from Pharmacy (it can be obtained as an unlicensed bag from Baxter- Order Code FKB2486). If not, make-up: withdraw 50ml from 500ml bag 0.9% Saline + 20mmolKCl, replace with 50ml 50% glucose. If after 12 hours, with plasma Sodium stable or increasing Can change to 0.45% Saline / 5% Dextrose + KCl 20mmol / 500ml. If after 12 hours, but plasma Sodium is low or falling Corrected sodium level should be rising as blood glucose falls during treatment. Do not change to 0.45% Saline/5% Dextrose + KCl 20mmol / 500ml. Instead, continue 0.9% Saline/5%glucose + 20mmol KCl / 500ml (see above) Corrected Na = Na + 0.4 ([Glucose] - 5.5) On-line sodium calculator http://www.strs.nhs.uk/resources/pdf/guidelines/correctedNA.pdf Some workers believe low Corrected Na relates to risk of cerebral oedema. If blood glucose <4mmol/l, give bolus 2 ml/kg 10% glucose and increase glucose in IV fluids: Do not stop insulin, although may temporarily be reduced for 1 hour. 0.45% Saline/10% glucose + 20mmolKCl / 500ml can be made as follows: withdraw 50ml from 500ml bag 0.45% Saline / 5% glucose + 20mmol KCl, replace with 50ml 50% glucose. Once pH >7.3 HCO3 >15, consider reducing insulin infusion rate rather than adding glucose to IV fluids if glucose <14mmol/L. If a massive diuresis continues, fluid input may need to be increased. Changing from IV to Subcutaneous Insulin Once glucose <14mmols/L, pH>7.30/HCO3 >15, blood ketones<1.0mmol/L and patient well, not vomiting and able to tolerate food, consider switching to subcutaneous insulin (urinary ketones may not have cleared completely). For insulin type, timing and dose, see your local protocol. Continue IV insulin until 60 minutes (if using soluble or long-acting insulin) or 10 minutes (if using Novorapid or Humalog) after first subcutaneous insulin to avoid rebound hyperglycaemia. Additional Notes Bicarbonate: Stop! Rarely, if ever, necessary. Continuing acidosis means insufficient resuscitation, or insulin infusion problems. Bicarbonate should only be considered if profoundly acidotic (pH < 6.9) and shocked, with circulatory failure. Its only purpose is to improve cardiac contractility. ALWAYS DISCUSS WITH THE CONSULTANT IN CHARGE, PREFERABLY ALSO WITH BRISTOL PICU. Phosphate: There is always depletion of phosphate, another predominantly intracellular ion. No evidence in adults or children that replacement has any clinical benefit and it may lead to hypocalcaemia. Anticoagulant prophylaxis: There is significant risk of femoral vein thrombosis in young and very sick children with DKA who have femoral lines inserted. Consider anticoagulation with Fragmin 100units/kg once daily. Children who are significantly hyperosmolar might also need anticoagulant prophylaxis (discuss with local consultant). R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 8 Patient details or hospital sticker: Insert Trust Logo Lab (L) or Gas (G) or Ward meter (W) Venous(V) or Cap (C) or Arterial(A) Gluc pH HCO3 Na K Urea Ketones (blood) Actual date & time Creatinine Time from start Aim to check bloods at the time intervals shown Base Excess Results Flow Sheet: 0 (baseline) 2 hours 6 hours 10 hours 14 hours 18 hours 22 hours 26 hours 30 hours 34 hours 38 hours 42 hours Other results FBC: CRP: OTHER: R Bragonier, CP Burren for South West Regional Paediatric Diabetes Network January 2010 Page 9