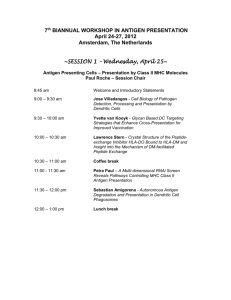
Immunology 3: Innate Immunity
Immunology 1: Introduction to Immunology
Explain the importance of immunology for human health
Function of the immune system: to identify and eliminate harmful microorganisms and substances
Mechanisms of action:
1.
Distinguishing ‘self’ from ‘non-self’ proteins
2.
Identifying ‘danger’ signals (e.g. from inflammation)
The immune system must make a compromise between removing the pathogen and causing accidental damage to the host (immunopathology)
Failure of proper function of the immune system function may lead to:
Persistent/fatal infections
Allergy
Autoimmune disease
Transplant rejection
The advent of vaccines resulted in a significant increase in human health (e.g. vaccines for diphtheria, polio and measles)
Generation times: time taken for reproduction
Pathogens have much shorter generation times than hosts (i.e. humans)
The host exerts selection on the pathogen and the pathogen exerts selection on the host
The pathogen replicates and can evolve much faster than the host
The host relies on a flexible and rapid immune response with a degree of non-specificity
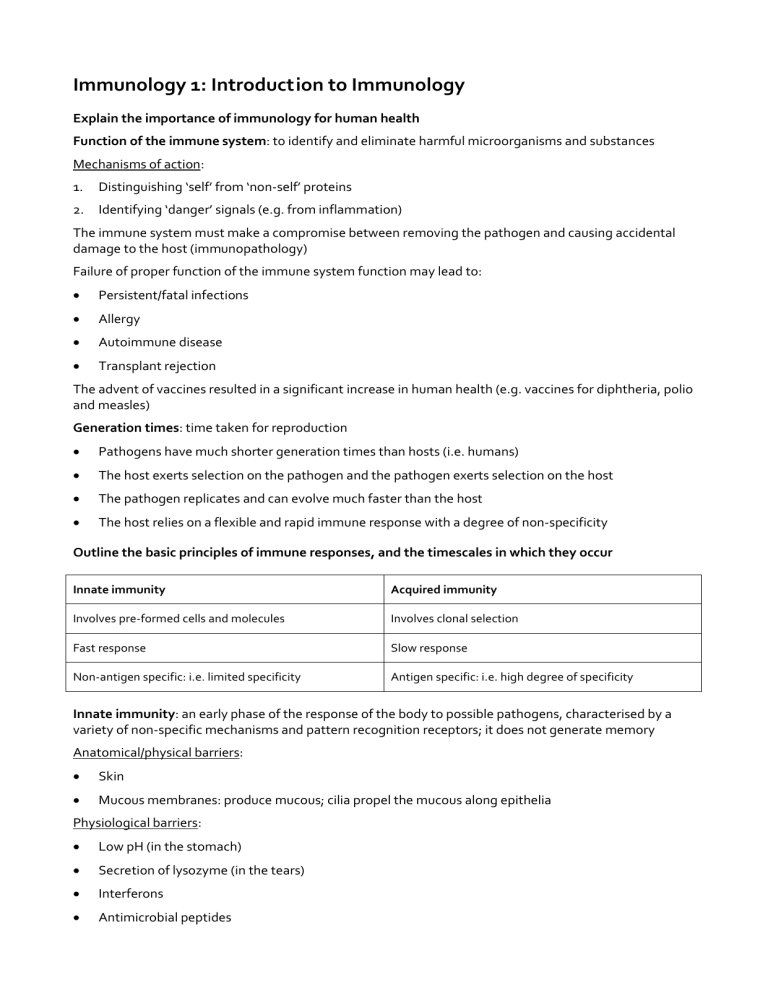
Outline the basic principles of immune responses, and the timescales in which they occur
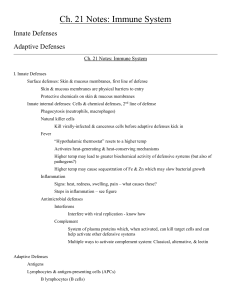
Innate immunity
Involves pre-formed cells and molecules
Fast response
Non-antigen specific: i.e. limited specificity
Acquired immunity
Involves clonal selection
Slow response
Antigen specific: i.e. high degree of specificity
Innate immunity: an early phase of the response of the body to possible pathogens, characterised by a variety of non-specific mechanisms and pattern recognition receptors; it does not generate memory
Anatomical/physical barriers:
Skin
Mucous membranes: produce mucous; cilia propel the mucous along epithelia
Physiological barriers:
Low pH (in the stomach)
Secretion of lysozyme (in the tears)
Interferons
Antimicrobial peptides
Complement
Components of the innate immune system
Cellular components: granular leukocytes
Natural killer cells (NK)
Macrophages (mononuclear phagocytes)
Neutrophils (polymorphonuclear leukocytes or PMN)
Basophils/mast cells
Eosinophils
Humoral components
Acute-phase proteins
Cytokines
Complement
Granulocytes:
Neutrophils (PMN): multi-lobed nucleus; phagocytic; 50-70% of circulating leukocytes
Eosinophils: bi-lobed nucleus; act against parasites; 1-3% of circulating leukocytes
Basophils: release granules containing histamines, serotonin or prostaglandins; not phagocytic; less than 1% of circulating leukocytes
Cytokines: small proteins which carry messages between cells
Mechanism of cytokine action:
1.
A stimulus induces cytokine-producing cells to secrete cytokines
2.
Cytokines bind to a receptor on the surface of a target cell
3.
This stimulates gene activation which has biological effects: cytokines stimulate proliferation of lymphocytes
Functions of the innate immune system:
Buys time while the acquired immune system is mobilised
Stimulates the acquired immune response (e.g. via cytokines and complement)
Acute phase inflammatory response: occurs in response to tissue damage (e.g. due to infection or trauma)
Effects:
Fever (rise in body temperature)
Increased production of acute phase proteins, mainly by the liver: o C-reactive protein and serum amyloid protein: bind to molecules found on the cell wall of some bacteria and fungi o Mannan-binding lectin: binds to mannose residues- these are not found on mammalian cells o These acute phase proteins direct phagocytes and complement to combat the infectious agent as part of the innate immune response
Acquired/adaptive immunity: the response of antigen-specific lymphocytes to antigen; it involves the development of immunological memory; adaptive responses can increase upon repeated exposure to the potential pathogen
Antigen specific
Can form memory
Requires priming
Effector arms: include B lymphocytes, T lymphocytes and antibodies
Components of the acquired immune system
Cellular components
T lymphocytes
B lymphocytes
Dendritic cells
(Basophils/mast cells)
(Eosinophils)
Humoral component
Antibodies
Define the terms antigen, antibody, B lymphocyte, T lymphocyte, active and passive immunity, primary and secondary immune responses
Antigen: a molecule which reacts with antibodies or T cells
Antibodies bind to the epitope region of the antigen
T cell receptors bind to peptide fragments of the antigen
Immunogen: an antigen which is sufficient to induce an immune response by itself
Antibody: an immunoglobulin molecule which binds specifically to the immunogen that induced its synthesis
Antibodies are produced by B lymphocytes and found in the bloodstream and body fluids
Antibodies are the humoral component of the acquired immune response
Types of immunoglobulin (Ig): IgG, IgA, IgM, IgE, IgD
IgG: monomer
75% of serum Ig
Bivalent
Can be transferred across the placenta
Longest serum half-life
Contributes to the secondary immune response
IgA: dimer
Tetravalent: 2 molecules are held together by a J chain
Found in body secretions
Contains a secretory piece to protect it from the action of hydrolytic enzymes in secretions
IgM: pentamer (star-shaped)
10% of serum Ig
Multivalent (decovalent): 5 molecules are held together by a J chain
IgE: monomer
Bivalent
Involved in allergic response and defence against parasites
Bound to basophils/mast cells: it triggers the release of histamines
IgD: monomer
Antibodies are specific to a particular antigen since the antigen-binding region (Fab region) on the antibody is complementary to the epitope (antibody-binding region) on the antigen
Mechanisms of antibody action against viruses:
1.
Neutralisation: the antibody binds to a virus and prevents its attachment to the host cell
2.
Opsonisation: the virus-antibody complex is phagocytosed by macrophages
3.
Complement-mediated lysis of enveloped viruses
4.
Antibody-dependent cell-mediated cytotoxicity (ADCC): this is mediated by NK cells
Lymphocytes: mononuclear agranular leukocytes
Antigen-specific: lymphocytes express antigen receptors on their surface which are specific to a particular antigen
Form 20-40% of circulating leukocytes and 99% of cells in lymph fluid
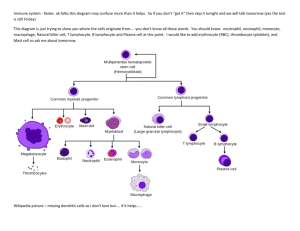
Lymphocyte precursors are produced in the bone marrow by self-renewing haematopoietic stem cells
Lymphocytes consist of bone marrow-derived and thymus-derived cells
Subsets of lymphocytes are distinguished by unique cell-surface markers
B lymphocytes: bone marrow-derived lymphocytes
Mature in the bone marrow
Recognise free antigen in the body fluids
Surface markers include: CD19 and class II MHC molecules
B cells produce 1 clone of antibody
The antibody may be bound to the surface of the B cells or it may be secreted by the B cells
The Fab (antigen-binding) region of an antibody is unique to a particular antigen
When an antigen binds to a surface antibody, this promotes the B cell to secrete antibodies
T lymphocytes: thymus-derived lymphocytes
Mature in the thymus
Recognise antigen presented at the cell surface by MHC molecules
Surface markers include: CD3, CD4 and CD8
T
H
cells (helper T cells): express the CD4 co-receptor on their surface
T
C
cells (cytotoxic T cells or CTLs): express the CD8 co-receptor on their surface
Regulatory T cells: a subset of T
H
cells which suppress the immune response
Naïve lymphocytes: have never encountered their cognate antigen and hence have never responded to it
Memory lymphocytes: the product of an immune response; they allow their specific receptor to remain in the pool of lymphocytes in the body
Active immunity: the induction of an immune response by the introduction of antigen
Passive immunity: immunity gained without antigen introduction (i.e. by transfer of antibody or immune serum into a naïve recipient)
Primary response: the response made by naïve lymphocytes when they first encounter their cognate antigen
Naïve lymphocytes are activated by antigen to ensure proliferation of a lymphocyte with the appropriate receptor for the antigen
After the antigen has been removed, a few lymphocytes with the cognate antigen remain as memory cells; the remaining lymphocytes die
Secondary response: the response made by memory lymphocytes when the reencounter their cognate antigen
The secondary response is more effective than the primary immune response: it is quicker, greater in magnitude and lasts longer than the primary response
Outline the concept of clonal selection, and its role in immune responses
Immune memory (secondary response): a response which occurs upon the 2 nd or subsequent exposure to a particular antigen
Lymphocyte antigen receptors:
T and B lymphocytes express unique surface antigen receptors which bind to proteins
Each cell has a particular antigen receptor which recognises and binds to the epitope of its cognate
(associated) antigen
There are many copies of the antigen receptor on the cell surface
Lymphocytes circulate constantly between the blood and tissues via the lymph
The thoracic duct is the final lymphatic vessel which reintroduces lymph into the subclavian vein
B cell antigen receptor (BCR): a surface immunoglobulin (i.e. a membrane-bound antibody)
T cell antigen receptor: the T cell receptor (TCR) consists of 2 protein chains
Generation of clonal diversity in lymphocytes:
During development of T and B lymphocyte precursors in the bone marrow: random genetic recombinations occur within each cell among multiple copies of immunoglobulin genes or TCR genes
This generates diversity of clones of lymphocytes
Each clone of lymphocytes has a different antigenic specificity (i.e. it is unique to a particular antigen)
Each naïve lymphocyte is the precursor of a genetically identical clone of daughter lymphocytes
Principle of clonal selection: when the surface antigen receptor of a T or B lymphocyte recognises and binds to its cognate antigen, it stimulates that particular clone of cells to proliferate
The surface antigen receptor of a T or B lymphocyte recognises and binds to its cognate antigen
This leads to selection and activation of a lymphocyte clone
Clonal expansion occurs: a clone of lymphocytes with identical antigenic specificities is produced
Most of the recently proliferated lymphocytes die at the end of the primary immune response due to lack of antigen, lack of cytokines or activation-induced cell death
Some proliferated lymphocytes survive as memory cells
In other words:
T and B cells produced in the primary lymphoid organs are released into the peripheral lymphoid pool
Those that meet their cognate antigen proliferate and produce effector and memory cells; those that do not meet their cognate antigen die
The size of the peripheral lymphoid pool is regulated by homeostatic mechanisms
Antigen presentation:
Antibodies and BCRs bind directly to the antigen
TCRs can only recognise processed antigen (peptide) which is bound to major histocompatibility complex (MHC) proteins on the cell surface
Human leukocyte antigens (HLA): the MHC molecules which occur in human cells
2 types of MHC molecules: class I MHC and class II MHC
Class I MHC molecules: occur on the surface of all cells
Class II MHC molecules: only occur on the surface of antigen presenting cells (APCs)
APCs include: dendritic cells, macrophages and B lymphocytes
Immune response:
T cell activation: occurs in the secondary lymphoid organs (e.g. lymph nodes)
Antigens are taken up by APCs and transported from tissues into secondary lymphoid organs where they meet T cells
T
C
cells (CTLs): kill infected cells
T
C
cells recognise virally infected cells via the peptides presented by class I MHC molecules
They kill infected cells by injecting granules containing lethal enzymes into the cells
Antibodies: recognise and label infected cells for destruction
Understand the roles of natural selection and the physical organization of the immune system in its function
Organisation of the lymphatic system:
Lymphatic vessels: venules, veins and ducts
Lymphatic tissues: nodules, nodes, tonsils and Peyer’s patches
Lymphatic organs: spleen and thymus
Lymphoid organs: organised tissue where lymphocytes interact with non-lymphoid cells; site of initiation and maturation of the adaptive immune response
Primary lymphoid organs: site of maturation of lymphocytes
Bone marrow: site of B cell maturation
Thymus: site of T cell maturation
Secondary lymphoid organs: lymph nodes, spleen (white pulp) and mucosa-associated lymphoid tissue
(MALT)
Lymphocytes and APCs recirculate through lymphatic vessels from tissues via lymph nodes or the spleen into the blood
Immunology 2: Immune Cells and Organs
Name the primary and secondary lymphoid organs and briefly differentiate between their functions
Primary lymphoid organs: the site of lymphopoiesis (production of lymphocytes)
Bone marrow: the site of haematopoiesis and B cell maturation
Thymus: the site of T cell maturation
Secondary lymphoid organs: the site where antigen, antigen presenting cells and mature lymphocytes come together to initiate an immune response
Spleen
Lymph nodes
MALT (mucosal-associated lymphoid tissue)
Secondary lymphoid organs have special vascular adaptations to recruit lymphocytes from the blood
Draw simple diagrams to illustrate the structure of the thymus, lymph node, spleen, Peyer’s patch, and indicate the changes that occur after stimulation by antigen
Thymus:
A bi-lobed structure which is located in the thorax
Each lobe is organised into lobules
Each lobule contains histologically defined regions of cortex and medulla
Cortex: contains immature thymocytes, some of which undergo selection to become mature thymocytes in the medulla
Medulla: contains mature thymocytes
Only ~5% of cells exit the thymus and enter the peripheral T cell pool
Atrophies with age: areas of active T cell maturation are replaced by adipose tissue
Simple diagram of a human thymic lobe:
Bone marrow:
Produces haematopoietic stem cells and B cells
Haematopoietic stem cells destined to become T cells migrate to the thymus
Differentiation of B cells is centripetal with stem cells under the bone; the most mature B cells are found towards the centre of the bone marrow
In the foetus: the liver and spleen are the first active sites of haematopoiesis; bones become active subsequently to the liver and spleen
In adults: active sites of haematopoiesis include spongy regions at the end of long bones, vertebral bones, the sternum, ribs and flat bones of the cranium and pelvis
Lymph nodes:
Diameter: 1-15 mm
Round or kidney-shaped
Have an indentation at the hilus where blood vessels (BV) enter and leave the lymph node
Lymph enters the lymph node through several afferent vessels (A)
Lymph leaves the lymph node through one efferent vessel (E) at the hilus
As lymph passes through a lymph node, phagocytes remove free antigens
Cortex: rich in B cells
Paracortex: rich in T cells
Simple diagram of a lymph node:
A: afferent
E: efferent
BV: blood vessel
Spleen:
Contains 2 main types of tissue:
Red pulp: acts as a general filter for antigens in the blood
White pulp: the lymphoid tissue; it initiates the major responses to blood-borne antigens
Periarterial lymphatic sheath (PALS): concentric areas of lymphoid tissue which surround the central arteriole
The PALS region nearest the central arteriole is rich in T cells
Lymphoid follicles: rich in B cells; occur periodically along the PALS
Marginal zone: the primary entry site of B and T cells into the white pulp; surrounds the PALS
Simple diagram of a part of the spleen:
Diagram of a part of the spleen:
Individuals who do not have a spleen are highly susceptible to infections with encapsulated bacteria
Epithelium: the first line of defence against infection
The skin and mucosal layers form a physical barrier with a very large surface area
Epithelia are heavily defended by MALT and the cutaneous immune system
MALT: an aggregate of lymphoid tissue which does not have a tough outer capsule
Occur predominantly in the lamina propria and submucosal areas of the GI, respiratory and genitourinary tracts
Examples of MALT: tonsils; appendix; Peyer’s patches
Peyer’s patches: organised regions of lymphoid tissue found in the wall of the gut
Predominantly contain B cells
Contain germinal centres during immune responses
Simple diagram of a Peyer’s patch:
Cutaneous immune system:
Consists of 2 parts: the epidermis and the dermis
Epidermis: contains Langerhans cells (epidermal dendritic cells) and intraepidermal lymphocytes
Dermis: contains T lymphocytes, macrophages and dermal dendritic cells
Outline the re-circulation of lymphocytes
Naïve lymphocytes: lymphocytes which have matured and have not yet encountered antigen
There are many naïve T and B lymphocytes with different specificities (i.e. they recognise different antigens); however there may only be a limited amount of antigen
Lymphocyte recirculation increases the likelihood that naïve lymphocytes will encounter their cognate antigen
Recirculation of naïve lymphocytes:
Naïve lymphocytes constantly circulate from the blood into secondary lymphoid organs: they leave blood vessels through high endothelial venules (HEVs)
HEVs: specialised sections of post-capillary venules
Naïve lymphocytes migrate from lymph nodes into efferent lymphatic vessels
They eventually return to the blood via the thoracic duct
In case of an infection: lymphocytes which recognise the infectious agent remain in the lymphoid tissue in lymph nodes, where they proliferate and differentiate
Explain the use of CD (cluster of differentiation) markers for discrimination between lymphocytes
Lymphocytes: small cells with agranular cytoplasm and a large nucleus
Subdivided into 2 groups:
1.
B lymphocytes: mature in the bone marrow
2.
T lymphocytes: mature in the thymus
B cells and T cells cannot be differentiated under a microscope using conventional stains
CD markers: an internationally recognised systematic nomenclature for cell surface molecules which is used to discriminate between haematopoietic cells; more than 300 CD markers exist
Compare and contrast phenotypic characteristics of B and T cells
T cells:
Produced by the bone marrow; mature in the thymus
All T cells express CD3
90% express α ß TCRs o 2/3 of these express CD4 o 1/3 of these express CD8
10% express γδ TCRs
2 subsets of T cells:
1.
CD4 + : T helper cells and regulatory T cells
Effector function: secrete cytokines
2.
CD8 + : CTLs
Effector functions: lyse infected cells; secrete cytokines
Thymic output (production of mature T cells by the thymus) decreases with age since the activity of the thymus steadily decreases after puberty
TCRs recognise processed antigen presented by MHC molecules at the surface of a cell
B cells:
Produced by and mature in the bone marrow
Express CD19 and CD20
Express MHC class II molecules which present antigen to T helper cells
Effector function: produce and secrete antibodies
BCRs (surface immunoglobulins) recognise intact, free antigen present in blood and body fluids
Recognise…
Antigen receptor
Express…
Site of maturation
T cells
Processed antigen presented at the cell surface by MHC molecules
TCR: either α ß or γδ
All T cells express CD3
α ß T cells express CD4 or CD8
Thymus
B cells
Intact, free antigen
BCR (surface immunoglobulin/antibody)
CD19 and CD20
Bone marrow
Give examples of antigen presenting cells and their locations
Antigen presenting cells (APCs): cells which present processed antigen (peptide fragments derived from proteins) to effector T cells to initiate the acquired immune response
Present antigen to APC
Activated dendritic cells
Activated B cells
Activated macrophages
Follicular dendritic cells
Location
Widely spread (e.g. in the skin and mucosal tissue)
Include Langerhans cells which are present below the skin
Lymphoid tissue
Lymphoid tissue
Lymph node follicles
T cells
T cells
T cells
B cells
Immunology 3: Innate Immunity
Characteristics of innate immunity:
Present from birth
Broad specificity: uses pattern recognition receptors to recognise pathogen associated molecular patterns (PAMP); does not use antigen-specific receptors
No immunological memory: i.e. it is not enhanced upon second exposure to a particular pathogen
Includes both cellular and humoral components
Provides a rapid response
Cooperates with and directs (subsequent) adaptive immunity
Innate immunity
Neutrophils
Cellular components
NK cells
Humoral components
Anti-microbial peptides
Innate & adaptive immunity
Monocytes/macrophages
Dendritic cells
Mast cells/basophils
Complement
Cytokines
Adaptive immunity
B lymphocytes
T lymphocytes
Antibodies
Briefly describe the functions of the important phagocytic cells: neutrophils, monocytes/macrophages
Phagocytes: engulf invading organisms, try to kill them and release signals to alert other cells
General mode of action of phagocytes:
1.
The pathogen is engulfed by the phagocyte via formation of pseudopodia around the pathogen
2.
The pseudopodia fuse to form a phagosome around the pathogen
3.
A lysosome fuses with the phagosome to form a phagolysosome
4.
The pathogen is killed by the action of hydrolytic enzymes contained within the lysosome
5.
Certain peptides from the degraded pathogen are released from the phagocyte
Neutrophils (PMN leukocytes): granular leukocytes (granulocytes)
Multi-lobed nucleus
Present abundantly in the circulation; make up 50-70% of circulating leukocytes
Short life-span: to limit damage to normal tissues
Die by apoptosis (programmed cell-death)
Circulate in the blood and migrate out into tissues to the site of damage/infection when required
They are the first cells to be recruited to the site of tissue infection
Mode of action of neutrophils:
1.
Migrate from circulation to the site of tissue infection
2.
Bind to the pathogen at the site of infection
3.
Phagocytose the pathogen
4.
Kill the pathogen
Migration of neutrophils from circulation into tissues: diapedesis and chemotaxis
Diapedesis: passage of cells through adjacent endothelial cells into tissues
Chemotaxis: directed movement of cells along a chemokine gradient to the site of infection
Chemokines: chemotactic cytokines which attract and direct cells to the site of infection
1.
Endothelial cells which line the blood vessels express integrin ligands on their surface
2.
Neutrophils express selectin ligands on their surface
3.
Activated macrophages at the site of tissue infection secrete alarm cytokines which signal infection
4.
Cytokines stimulate endothelial cells which line local blood vessels to express selectins on their surface
5.
Selectins bind to selectin ligands on the surface of neutrophils: this is a weak interaction and causes neutrophils to slow down and roll along the blood vessel
6.
Inflammatory signals stimulate neutrophils to express integrins on their surface
7.
Integrins bind to integrin ligands on the surface of endothelial cells: this is a strong interaction and causes neutrophils to stop rolling
8.
Chemokines stimulate neutrophils to migrate through the endothelial cell layer to the site of inflammation
Phagocytosis of pathogens by neutrophils:
Neutrophils are highly phagocytic cells: this is a key component of host defence
When many neutrophils are involved in phagocytosis an abscess filled with pus is formed
Phagocytosis is much more effective following opsonisation
Opsonisation: the process by which pathogens are coated with opsonins to facilitate phagocytosis
Opsonins: molecules which can bind to antigens and be bound by phagocytes
Opsonins include antibodies and complement
Mechanism of neutrophils binding opsonins:
1.
IgG opsonises the pathogen by binding to cognate antigens on the surface of a pathogen
2.
This activates the complement system
3.
C3b opsonises the pathogen by binding to the surface of the pathogen
4.
IgG binds to the Fc receptor and C3b binds to the CR1 receptor on the surface of a neutrophil
5.
This activates the neutrophil and the pathogen is phagocytosed
Killing of pathogens by neutrophils: (following phagocytosis)
Neutrophils have multiple killing mechanisms; the respiratory burst is the most important of these
Oxygen-independent mechanisms:
Granules, containing hydrolytic enzymes, fuse with phagolysosomes and kill phagocytosed pathogens
Antimicrobial peptides (e.g. defensins)
Oxygen-dependent mechanisms:
Respiratory burst: activated neutrophils produce toxic metabolites which damage pathogens o Hydrogen peroxide, superoxide anions, singlet oxygen and hydroxyl radicals o Reactive nitrogen intermediates (nitric oxide)
Neutrophil deficiency is associated with infections caused by extracellular bacteria and fungi
Monocytes:
Leukocytes which enter the bloodstream from the bone marrow
Precursors to macrophages and dendritic cells
Leave the circulation through pores between adjacent endothelial cells lining the blood vessels, enter tissues and mature into macrophages
Secrete alarm cytokines, particularly: IL-1, IL-6, IL-8 and TNFα
Macrophages:
Less abundant than neutrophils
Long life-span relative to neutrophils
Dispersed throughout peripheral tissues and beneath all exposed tissues
Produce cytokines to signal infection to recruit other immune system cells to the site of infection
Function as APCs: macrophages present processed antigen to helper T cells
Mode of action of macrophages:
Express pattern recognition receptors which recognise PAMP
Become activated when PAMP bind to macrophage receptors
Activated macrophages secrete cytokines to recruit other cells to the site of infection
Phagocytose and kill pathogens to which they bind
Define cytokines and describe their general properties
Cytokines: small soluble molecules which facilitate communication between cells of the immune system
Small secreted proteins which are involved in cell-cell communication
Generally act locally
Powerful biological effects, even at low concentrations
Short-lived
When a cytokine binds to its receptor: a change in gene expression occurs (e.g. cytokines stimulate proliferation of lymphocytes)
IL-1
TNFα
IL-6
IL-8
IL-12
Type of cytokine
Interleukins (IL)
Interferons (IFN)
Chemokines
Growth factors
Function
Facilitate communication between leukocytes (IL is a generic name for a cytokine)
Have anti-viral effects
Required for chemotaxis (i.e. to recruit cells to the site of infection)
Required for the development of cells of the immune system
Can induce cell death; e.g. tumour necrosis factor (TNF) Cytotoxic cytokines
Cytokines secreted by activated macrophages
Function
Alarm cytokine which induces the fever response
Alarm cytokine
Stimulates production of acute phase proteins in the liver
Chemokine: stimulates chemotaxis of neutrophils to the site of tissue infection
Directs adaptive immunity; activates NK cells
Bacterial septic shock: a systemic infection caused by bacterial endotoxins
Effects:
Secretion of alarm cytokines (TNFα and IL-1) by activated macrophages
Increased vascular permeability due to cytokines
This leads to hypotension severe drop in blood pressure
Death occurs in 10% of cases
Dendritic cells: recognise pathogens and secrete cytokines
Found in the skin and near mucosal epithelia
Express pattern recognition receptors which recognise PAMP
Become activated when PAMP bind to dendritic cell receptors
Activated dendritic cells secrete cytokines which stimulate chemotaxis of monocytes to enter tissues and mature into dendritic cells
Activated dendritic cells capture pathogens and migrate to local lymph nodes to present antigens to the adaptive immune system
Define complement, list its major functions, and draw a simple diagram of the complement pathways
Complement system: a cascade of serum enzymes activated by the presence of a pathogen
Plays a major role in innate and antibody-mediated immunity
Consists of a series of ~30 proteins and glycoproteins with a relatively high serum concentration (3-4 mg/ml)
Enzyme cascade system which produces a rapid, highly amplified response
Components of the complement system are mainly produced in the liver and also by monocytes and macrophages
Must be activated before it can function: there are 3 mechanisms for activation
3 mechanisms for activation of the complement system:
1.
Classical pathway: antibody-dependent activation; activated by antibody-antigen complexes
2.
Alternative pathway: antibody-independent activation; direct activation by the pathogen surface
3.
Lectin pathway: antibody-independent activation by lectins which bind to carbohydrates only found on pathogens
All of the pathways converge at the activation of C3: C3 C3a + C3b
C3 leads to the final Common Pathway
The Common Pathway ends with the formation of the membrane attack complex (MAC)
Functions of the complement system:
Lytic pathway: complement causes cell lysis by formation of the MAC
Opsonisation: C3b opsonises the surface of pathogens which facilitates phagocytosis
Anaphylatoxins: complement fragments which as chemokines (these include C3a and C5a)
Control of the complement system:
Components of the complement system are labile (i.e. they have a short half-life)
Components of the complement system are diluted in biological fluids
Specific regulatory proteins help inhibit complement activation: these include circulating and membrane-bound proteins
Describe a typical inflammatory response to a localised infection involving recruitment of neutrophils, and phagocytosis and killing of bacteria
Briefly outline the events involved in a systemic acute phase response
Mast cells:
Located beneath all exposed surfaces (like macrophages) o Mucosal mast cells: present in the lungs o Connective tissue mast cells: present in the skin, peritoneal cavity and near blood vessels
Protect against parasitic infection by degranulation: o Mast cells have granules which contain active chemicals, such as histamine o The mast cell releases the contents of its granules onto the parasite to kill it
Recognise, phagocytose and kill opsonised bacteria
Secrete inflammatory mediators, including histamine and cytokines
Anaphylatoxins activate mast cells and trigger mast cell degranulation
Activated mast cells lead to vasodilation and increased vascular permeability
Local acute inflammatory response:
1.
Macrophage activation
2.
Cytokine secretion
3.
Endothelium activation
4.
Leukocyte extravasation and chemotaxis
5.
Phagocytosis and killing by neutrophils
6.
Complement activation
7.
Opsonisation
8.
Mast cell degranulation
9.
Increase in vascular permeability
Systemic acute phase response:
Often accompanies a local inflammatory response, 1-2 days later
Alarm cytokines (IL-1, IL-6 and TNFα ) induce the acute phase response
Alarm cytokines affect the hypothalamus, adrenal cortex, liver and bone marrow
Effects of the acute phase response:
Fever
Increased leukocyte production (leukocytosis)
Production of acute-phase proteins by the liver
Acute-phase proteins:
C-reactive protein (CRP): o Binds to the C polysaccharide of pneumococcus
o Activates complement o The CRP level may increase up to 1000 fold
Mannan-binding lectin (MBL): binds to mannose residues o Opsonises pathogens for phagocytosis by monocytes o Activates complement via the lectin pathway
Serum amyloid A: similar to CRP
Complement components
Fibrinogen: involved in clotting
Outline the phenotype and functions of natural killer (NK) cells
Natural killer cells:
Large granular lymphocytes
Cytotoxic
Circulate in the blood, spleen and liver; make up 5-10% of peripheral circulating lymphocytes
Activated NK cells secrete cytokines (interferonγ )
Lyse target cells
Antibody dependent cell cytotoxicity (ADCC): when Fc receptors on NK cells bind to antibodies, the cytotoxic ability of NK cells is stimulated
Important in defence against tumour cells and viral infections (especially Herpes): NK cells induce apoptosis in these cells
Do not have antigen-specific receptors (unlike T and B lymphocytes)
Express both activating and inhibitory receptors
Killing depends on a balance of different signals: o Ligation of inhibitory NK receptors inhibition of target cell killing o Ligation of activating NK receptors target cell killing
Immunology 4: Antibodies
Describe with the aid of a simple diagram the immunoglobulin molecule, identifying the antigenbinding site (Fab) and Fc portions of the molecule
Antibody: a protein that is produced in response to an antigen and has the property of binding specifically to the antigen that induced its formation
Antibodies constitute the immunoglobulin class of proteins
Antibodies are a large family of soluble glycoproteins
B lymphocytes produce antibodies
Individuals have many different antibodies (>10 7 ); antibody-deficiency is life-threatening
Secondary effector functions of the antibody-antigen complex: o Complement activation (via the classical pathway) o Opsonisation: this facilitates phagocytosis of the pathogen o Cell activation via binding of the Fc region of the antibody to Fc receptors on the surface of certain cells (e.g. macrophages)
IgG structure:
Symmetrical structure: composed of 2 light chains (Lc) and 2 heavy chains (Hc) held together by disulphide bonds
Each IgG molecule has 2 identical Fab regions which can bind to antigens
The Fab regions of a particular antibody can bind to a specific antigen
Each IgG molecule has an Fc region which can bind to Fc receptors on the surface of certain cells
The IgG molecule is flexible due to the presence of a hinge region
The hinge region allows the each of the 2 Fab arms to bind to an antigen
Ig treated with
Papain
Pepsin
Mercaptoethanol
No. of fragments produced Ratios of each type of fragment
3 2 Fab fragments : 1 Fc fragment
2
2
1 F(ab)
2
fragment : many small fragments derived from Fc
1 Hc : 1 Lc
Heavy and light chains:
Consist of constant domains (C
H
or C
L
) and variable domains (V
H
or V
L
)
Heavy chain structure: 1 variable domain (V
H
) + 3 or more homologous constant domains (C
H
)
Light chain structure: 1 variable domain (V
L
) + 1 constant domain (C
L
)
Briefly describe the properties of the antigen-binding site
Properties of the antigen-binding site (Fab region):
A relatively large, flat surface with undulations
Composed of the variable domains of heavy and light chains (i.e. the V
H
and V
L
domains)
Each variable domain has 3 hypervariable regions
The 3 hypervariable regions form the complementarity determining regions
Epitope: the site on an antigen which is bound by the Fab region of an antibody
There is a high degree of complementarity between an Fab region and an epitope
Distinguish between antibody affinity and avidity
Antibody affinity: the strength of the total non-covalent interactions between a single antigen-binding site of an antibody and a single epitope on its cognate antigen
Antibody + antigen antibody-antigen complex
Each individual antibody-antigen interaction is relatively weak and has a low affinity since the interactions are non-covalent
Forces involved in antibody-antigen binding include: hydrogen bonds; ionic bonds; hydrophobic interactions; van der Waals interactions
Antibody avidity: the overall strength of multiple interactions between an antibody with multiple antigenbinding sites and a complex antigen with multiple epitopes
Avidity is a better measure of binding capacity in biological systems
Polyvalent antibodies have a higher avidity than monovalent/bivalent antibodies
Cross-reactivity: an antibody elicited in response to one antigen can also recognise a different antigen
Examples of cross-reactivity:
1.
Vaccination with cowpox induces antibodies which are able to recognise smallpox
2.
ABO blood group antigens (glycoproteins on red blood cells): antibodies made against microbial antigens on normal gut flora may cross-react with ABO blood group antigens
List the immunoglobulin classes and sub-classes in man. Describe their functions and relate these to
their individual structure
Isotypes: immunoglobulin structures which are present in all members of a species
E.g. kappa and lambda light chains; the different heavy chains; Ig classes and subclasses
Allotypes: allelic polymorphisms of an Ig molecule which vary in the population; allotypes are not present in all members of a species; allotypes are usually detected by antibodies
E.g. gamma chain; kappa chain
Immunoglobulin classes:
The constant region of the heavy chain of an antibody determines its class and function
Immunoglobulins may have either a κ or a λ light chain; a given Ig has the same type of light chain since the Ig molecule must be symmetrical
Different classes of antibodies differ in the constant regions of their heavy chains:
Ig class
Heavy chain
Light chain
Ig class
Ig subclass
Heavy chain
IgG
γ
IgA
α
IgG
IgM
μ
κ or λ
IgE
ε
IgA
IgD
δ
IgG1
γ 1
IgG2
γ 2
IgG3
γ 3
IgG4
γ 4
IgA1
α 1
IgA2
α 2
IgG:
Present in the blood and extracellular fluids
The most abundant immunoglobulin
The most important immunoglobulin in defence generally: IgG neutralises toxins and viruses
Exists as a monomer (which has 2 Fab regions)
Actively transported across the placenta: this provides passive immunity to the foetus
Activates complement via the classical pathway (mainly IgG1 and IgG3)
Opsonises pathogens for phagocytosis: phagocytes have Fc receptors that recognise the Fc chain
4 subclasses of IgG: variability of the subclasses is mainly located in the hinge region and effector function domains (i.e. the Fc region)
(Stimulates ADCC in NK cells)
IgA:
Major secretory immunoglobulin: IgA has an important role in seromucous secretions
The 2 nd most abundant immunoglobulin
In the blood: exists as a monomer (which has 2 Fab regions)
In secretions: exists as a dimer (which has 4 Fab regions) o Dimer structure: 2 IgA monomers are held together by a J chain and a secretory component o The secretory component is added to the molecule during its passage through epithelial cells out into the secretions o It protects IgA from acids and enzymes found in secretions (e.g. the GI tract)
Secretory IgA neutralises toxins and blocks the infectivity of infectious agents
Protects mucosal surfaces from bacteria, viruses and protozoa
2 subclasses of IgA: IgA1 predominates in the blood; IgA2 predominates in secretions
(Secreted in the milk: IgA coats the baby’s intestinal mucosa and protects against ingested pathogens)
(Does not activate complement)
IgM:
Mainly present in the blood (80%)
Exists as a pentamer (which has 10 Fab regions) o Pentamer structure: 5 monomers are held together by a J chain o The 5 Fab pairs allow it to bind strongly to the surface of bacteria: this causes agglutination
The 1 st antibody to be produced after exposure to an antigen; it is involved in the primary antibody response
Active in the blood
Multiple Fab sites compensate for its low affinity; therefore it has a relatively high avidity
Efficient at agglutination (clumping together of antigens)
Activates complement (via the classical pathway)
IgE:
Present in extremely low concentrations
Produced in response to parasitic infections and in allergic diseases o Defends against parasites o Causes allergies and anaphylactic shock
Fc receptors on mast cells and basophils have a high affinity for the Fc region of IgE
Cross-linking by antigen triggers mast cell activation and histamine release: this is important in protection against certain parasitic infections
(Allergic response):
On 1 st exposure to an allergen:
o Many IgE antibodies are produced o Fc receptors on the surface of mast cells bind to the Fc region of the IgE antibodies
On 2 nd exposure to the allergen: o IgE antibodies which are bound to the surface of mast cells bind to the allergen o This causes cross-linking (clustering) of many IgE antibodies which brings many Fc receptors close to each other o Degranulation occurs: the mast cell releases granules containing histamine into tissues
IgD:
The least well characterised immunoglobulin
Extremely low serum concentrations (it is not really found as a free antibody)
Surface IgD is expressed early in B cell development
Involved in signalling during development and activation of B cells
Selective distribution of immunoglobulins:
Blood: IgG and IgM
ECF: IgG
Secretions: IgA (dimer)
Foetus (via placental transfer): IgG (maternal)
Below the epithelium: IgE (associated with mast cells)
Brain: lacks immunoglobulins
Functions of antibodies:
In defence:
Targeting and recognising infectious organisms
Recruitment of secondary effector mechanisms
Neutralisation of toxins
Removal of antigens
Inducing passive immunity in newborns (IgG)
In medicine:
Ig levels are used in diagnosis and monitoring (e.g. a viral infection leads to synthesis of specific antibodies)
Pooled antibodies are used for passive therapy and protection (i.e. prophylaxis)
In laboratory science:
Many diagnostic and research applications
Immunology 5: B lymphocytes
Adaptive immune response:
Develops after exposure to antigen
Requires time to develop
2 arms: humoral and cell-mediated
B lymphocytes:
Derived from haematopoietic stem cells in the bone marrow
Main effector cells of humoral immunity: activated B lymphocytes secrete antibodies
Mature in the bone marrow in the absence of antigen
Migrate into circulation (blood and lymph) and into lymphoid tissues
Activation and differentiation occur in peripheral lymphoid tissues in the presence of antigen
B cell maturation: antibody-independent phase
1.
Stem cell pro-B cell
2.
Pro-B cell pre-B cell
3.
Pre-B cell immature B cell
4.
Immature B cell mature B cell: self-reactive immature B cells are destroyed
B cell antigen receptors (BCRs): confer specificity to a particular antigen
Many identical BCRs are present on the surface of a mature B cell
Therefore each B cell is specific to a particular antigen since all the BCRs on a given B cell recognise the same antigen
BCRs have a unique antigen-binding site (Fab region) which binds to the epitope of an antigen
BCRs are made before the B cell encounters antigen
BCR structure: transmembrane protein complex
BCRs consist of a membrane-bound immunoglobulin and 2 associated heterodimers
Each heterodimer is composed of Ig α and Igß, linked by a disulphide bond
Heterodimers contain an immunoglobulin-fold structure
N.B. in contrast to BCRs, antibodies are free immunoglobulins which are not bound to the membrane of a
B lymphocyte since they lack the protein sequence which anchors BCRs to the surface of a B cell
BCR signalling:
The membrane-bound Ig of a BCR recognises the epitope of its cognate antigen: it must communicate this to the nucleus of the B cell
The cytoplasmic tail extending from the heavy chain of the membrane-bound Ig into the interior of the B cell is too short to signal
The cytoplasmic tails of Ig α and Igß are long enough to interact with intracellular signalling molecules
Briefly outline the principles of immunoglobulin (Ig) gene rearrangement in the generation of diversity
There is an almost infinite number of potential antigens
The immune system must be able to respond to all these potential antigens; therefore it requires a large repertoire of cells which have specific receptors that can recognise all potential antigens
Immunoglobulin gene rearrangement: exclusive to B and T lymphocytes
Each Ig of a BCR is composed of heavy chains and κ and λ light chains
Each chain is encoded by a gene which is assembled from gene segments
Genes encoding each type of chain are present on different chromosomes
During B cell maturation the gene segments are rearranged and combined
This generates the diversity of the lymphocyte repertoire
Only B cells which successfully rearrange their genes will mature and enter circulation
Heavy chain synthesis: chromosomes which encode the heavy chain have multiple copies of V, D, J and C gene segments
Light chain synthesis: chromosomes which encode the heavy chain have multiple copies of V, J and C gene segments
Process of gene rearrangement:
1.
Rearrangement of germline DNA B cell DNA
Each B cell chooses one of each kind of segment at random and joins them together by deleting the
DNA sequences in between them to form B cell DNA
The unused DNA sequences are deleted by being looped out and removed
2.
Transcription of B cell DNA primary RNA transcript
Transcription only occurs if there is a productive rearrangement of gene segments (i.e. the B cell DNA encodes a functional chain)
3.
Splicing of primary RNA transcript mature mRNA
4.
Translation of mature mRNA functional chain polypeptide
5.
The functional chain is transported to the cell surface
6.
BCRs are made at the cell surface by assembly of heavy and light chains
Describe the process of stimulation of individual B cells to divide and secrete antibody such as to generate immunity to a particular antigen (clonal selection)
Clonal selection of B cells: antigen-dependent phase
A naïve B cell is activated when its BCRs bind to their cognate antigen and when it receives costimulation (see below)
Naïve B cell: a B cell which has not yet encountered antigen
The activated B cell proliferates to produce a clone of cells with identical BCRs
All of the clonally expanded B cells have the same specificity (i.e. they express BCRs which recognise the same antigen)
The clonally expanded B cells secrete antibodies into the bloodstream
Finally when the pathogen has been eliminated most of the B cells die
Outline the differences in antibody production during primary and secondary immune responses
A naïve B cell cannot be activated by encountering antigen alone; it requires a co-stimulatory signal in addition to encountering antigen
2 pathways of B cell activation:
1.
Thymus-independent activation: microbial constituents directly supply the co-stimulatory signal
2.
Thymus-dependent activation: T helper cells supply the co-stimulatory signal
Thymus-independent activation:
Thymus-independent antigens directly activate B cells without the help of T cells
Therefore antibody formation can be induced in people with no thymus and no T cells
The co-stimulatory signal is supplied by the microbial constituent or by an accessory cell
Thymus-dependent activation:
Thymus-dependent antigens require T helper cells to activate B cells
Antigen recognition and presentation by B cells:
1.
A BCR recognises and binds to its cognate antigen
2.
The BCR-antigen complex is internalised by the B cell
3.
The internalised antigen is degraded into peptides by hydrolytic enzymes
4.
The peptides associate with class II MHC molecules to form a class II MHC-peptide complex
5.
The class II MHC-peptide complex is transported to the surface of the B cell for expression
6.
T helper cells with complementary TCRs recognise the complex and secrete cytokines which bind to the B cell and activate it
T helper cell dependent activation:
1.
When BCRs bind to antigens they cross-link (cluster) on the surface of the B cell: this co-stimulates B cells to up-regulate expression of class II MHC molecules and B7 proteins
2.
Antigens are internalised, processed and presented by B cells as above
3.
T helper cells recognise their cognate antigen: this co-stimulates and activates T helper cells
4.
Activated T helper cells express CD40L
5.
CD40L interacts with CD40 on the surface of B cells: this co-stimulates B cells to express cytokine receptors on their surface
6.
B7 interacts with CD28 on the surface of T helper cells: this co-stimulates T helper cells to secrete cytokines which bind to cytokine receptors on the surface of B cells
7.
This stimulates B cells to proliferate and differentiate to form plasma B cells which secrete antibodies into the bloodstream
Class switching: only occurs in mature B cells which have encountered antigen
When naïve B cells are activated they mainly produce IgM antibodies
As B cells mature they can change the class of antibody which they make
The class of an antibody is determined by the constant region of its heavy chain
The gene segments which encode the constant regions of the heavy chain are located adjacent to each other on the same chromosome
Special switching signals are located between constant region gene segments: they allow class switching to occur
Cytokines made by T helper cells influence class switching:
Proliferation cytokines stimulate activated B cells to proliferate
E.g. IL-2, IL-4, IL-5
Differentiation cytokines stimulate proliferating B cells to differentiate into different classes
E.g. IL-2, IL-4, IL-5, IFNγ , TGF-ß
Immunological memory: once the immune system has recognised and responded to a particular antigen it exhibits memory for that antigen
Immunological memory is a consequence of clonal selection
Primary immune response: induced by initial exposure to antigen
Involves naïve B cells which mainly produce IgM
Secondary immune response: induced by subsequent exposure to the same antigen
Involves the clonally expanded population of memory B cells which mainly produce IgG
Memory B cells only produce antibodies when they are activated by T helper cells
The secondary immune response is more faster and greater than the primary immune response
Antibodies produced by the secondary immune response have a higher affinity for antigen
Differentiate between monoclonal and polyclonal antibodies
An antigen has multiple epitopes; therefore a mixture of antibodies is produced in response to a single antigen (polyclonal response)
Monoclonal antibodies: derived from a single clone of B cells
Polyclonal antibodies: derived from many different clones of B cells
Immunology 6: T-Lymphocytes and Antigen Recognition
Outline the origins and functions of T lymphocyte subsets
T lymphocytes:
Destroy intracellular pathogens
Recognise foreign antigen via a specific T cell receptor (TCR) on their surface
TCRs recognise processed antigen (i.e. small peptide fragments derived from larger proteins of a pathogen) presented by an MHC molecule on the surface of the infected host cell
T cell receptors (TCRs):
TCRs consist of 2 polypeptide chains: they are either α ß or γδ
α ß TCRs: composed of an α chain and a ß chain; present on the surface of the majority of T cells
γδ TCRs: composed of a γ chain and a δ chain; present on the surface of a small subset of T cells
α ß TCRs:
Recognise an MHC-peptide complex on the surface of a cell
TCRs on a given T cell recognise peptides associated either with MHC class I molecules or with MHC class II molecules
Structure of each chain: variable region, constant region, hinge, transmembrane region and cytoplasmic tail
The α chain and ß chain are held together by a disulphide bond at the hinge
Signalling:
The cytoplasmic tails of the α and ß chains are too short to signal
T cells express the CD3 signalling complex
The CD3 complex is composed of 4 proteins: γ , δ , ε and ζ
CD3 proteins are anchored in the cell membrane; they have cytoplasmic tails which are long enough to signal
Antigen recognition: there are 2 major populations of T cells which express either CD4 or CD8 coreceptors on their surface
Class I restricted: express CD8 co-receptors; recognise peptide presented by MHC class I
Class II restricted: express CD4 co-receptors; recognise peptide presented by MHC class II
Functions of co-receptors:
Recognise antigen and bind to the appropriate MHC molecule
Increase the avidity of the interaction between a T cell and its target cell
Important in signalling
Interaction with target cells:
CD8 + cells (CTLs): cytotoxic (kill target cells); secrete cytokines
Induce apoptosis in the target cell
CD4 + cells (T-helper cells): secrete cytokines
Recruit the effector cells of innate immunity
Help activate macrophages
Amplify the CTL and B cell responses
T lymphocytes only recognise processed antigen presented by MHC molecules at the cell surface:
1.
CD8 + CTLs: recognise and kill virus-infected cells
2.
CD4 + Th1 cells: recognise and activate macrophages which have phagocytosed bacteria
3.
CD4 + Th2 cells: recognise and activate antigen-specific B cells
Thymus:
Movement of T cells:
1.
Progenitor T cells produced by the bone marrow enter the thymus from the blood
2.
T cells migrate to the cortex of the thymus, where they are known as immature thymocytes
3.
T cells migrate from the cortex to the medulla, where they are known as mature thymocytes
4.
Mature thymocytes leave the thymus and enter the circulation
Development of T cells:
1.
Progenitor T cells which enter the thymus don’t express CD4, CD8 or a TCR (i.e. CD4 CD8 TCR )
2.
T cells undergo gene rearrangement and express low levels of pre TCR: this consists of a ß chain and a surrogate α TCR (i.e. CD4 CD8 pre TCR + )
3.
T cells become double positive as they migrate through the cortex: they express both CD4 and CD8 coreceptors in addition to TCRs (i.e. CD4 + CD8 + TCR + )
4.
T cells become single positive as they move from the cortex into the medulla: they express either CD4
or CD8 in addition to TCRs (i.e. CD4 + TCR + or CD8 + TCR + )
Gene rearrangement: the gene encoding each chain ( α and ß) is formed by recombination of germline
DNA to produce rearranged DNA
ß chain: rearranged DNA is formed by recombination of V, D, J and C fragments of germline DNA
α chain: rearranged DNA is formed by recombination of V, J and C fragments of germline DNA
Selection: only 5% of thymocytes survive selection
1) Following gene rearrangement, T cells which express pre TCR undergo selection:
If the ß chain is functional: T cells survive selection and develop to form double positive T cells
If the ß chain is not functional: T cells die by apoptosis
2) Double positive T cells undergo positive selection in the cortex:
Useless T cells whose TCRs cannot recognise self MHC-peptide complexes die by apoptosis
Useful T cells whose TCRs recognise self MHC-peptide complexes weakly survive selection
3) T cells whose TCRs which survive positive selection undergo negative selection in the medulla:
Dangerous T cells whose TCRs recognise self MHC-peptide complexes strongly die by apoptosis
Selection results in mature T cells which recognise self MHC-peptide complexes but not self antigens
Briefly describe the structure and distribution of major histocompatibility complex (MHC) class I and class II molecules
MHC: the major histocompatibility complex
A group of tightly linked genes which are important in specific immune responses
Discovered by experiments looking at the genetic basis of transplant rejection in mice
Found in all vertebrates
MHC molecules are highly polymorphic glycoproteins which present processed antigen to T lymphocytes
2 types of MHC molecules: class I and class II
HLA (human leukocyte antigens): encoded by the human MHC
Human MHC genes have various functions, including immune-related functions
The human MHC is polygenic: i.e. it consists of several genes for both class I and class II MHC proteins
Each individual inherits 2 MHC alleles at a single locus, 1 from each parent
Expression of genes is co-dominant: i.e. both maternal and paternal genes are expressed
Human MHC genes are highly polymorphic: i.e. there are many alleles of the genes which encode
MHC proteins
MHC haplotype: a group of MHC alleles which are linked on one chromosome
Different people have different immune responses due to polymorphism of MHC genes
MHC alleles are not randomly distributed; they segregate with race due to exposure to different infections in different regions
MHC class I molecules:
Transplantation antigens: control transplant acceptance/rejection
Expressed on the surface of most nucleated cells in the body at varying levels
Expression levels may be altered by cytokines or during infection
Gene expression:
Each MHC class I molecule is composed of 1 heavy chain and 1 light chain
The heavy chain is an α chain which has 3 regions: α 1, α 2 and α 3
The light chain is ß2-microglobulin
There are 3 MHC class I genes on each chromosome: HLA-A, HLA-B and HLA-C
Therefore each individual has 6 MHC class I genes
Each MHC class I gene encodes a heavy chain which pairs with the light chain
Peptide binding:
MHC class I molecules accommodate peptides 8-10 amino acids in length
The binding groove of the MHC molecule is closed at both ends
The anchor amino acids which bind to the peptide are clustered at the ends of the binding groove
MHC class II molecules:
Regulatory: control the ability of T cells to mount an immune response
Usually expressed only on the surface of antigen presenting cells (dendritic cells, B lymphocytes and macrophages)
Expression levels may be regulated by cytokines
Gene expression:
Each MHC class II molecule is composed of 2 heavy chains which are of a similar length
Heavy chain 1 is an α chain which has 2 regions: α 1 and α 2
Heavy chain 2 is a ß chain which has 2 regions: ß1 and ß2
MHC class II proteins are encoded by genes in the HLA-D region
Peptide binding:
MHC class II molecules accommodate peptides which are 13 amino acids in length or greater
The binding groove of the MHC molecule is open at both ends
The anchor amino acids which bind to the peptide are spaced along the binding groove
MHC structure:
Peptide-binding region
Ig-like region
CD binding site
Transmembrane region
Cytoplasmic region
MHC class I
α 1 and α 2
α 3 and ß2-microglobulin
α 3: binds to CD8
MHC class II
α 1 and ß1
α 2 and ß2
ß2: binds to CD4
Outline the mechanisms by which antigen presenting cells (APCs) process and present antigens
2 mechanisms of antigen presentation:
1.
Endogenous antigens: presented to MHC class-I restricted CD8 + T cells by MHC class I molecules
Virus-infected cells present to CTLs (T-killer cells) via MHC class I molecules
2.
Exogenous antigens: presented to MHC class-II restricted CD4 + T cells by MHC class II molecules
Macrophages which have ingested bacteria present to Th1 cells via MHC class II molecules
B cells which have bound to their cognate antigen present to Th2 cells via MHC class II molecules
Two pathways of antigen presentation are required because:
Antigens in different locations require different responses
Each pathway presents antigen from different locations to different T cell subsets
Endogenous antigen presentation by MHC class I molecules:
1.
Endogenous antigens are cut up into peptides by proteasomes
2.
Peptides are transported into the rER by TAP transporters for processing
TAP: transporter associated with antigen processing
3.
Peptides bind to the grooves of MHC class I molecules
4.
MHC I-peptide complexes move from the rER to the Golgi complex within vesicles
5.
MHC I-peptide complexes are transported from the Golgi complex to the cell surface for display
Exogenous antigen presentation by MHC class II molecules:
1.
An MHC class II molecule is formed by association of α and ß chains in the cytoplasm
2.
The class II MHC molecule is injected into the rER; an invariant chain occupies its binding groove
3.
The MHC-invariant chain complex is transported from the rER to an endosome in the cytoplasm
4.
Exogenous antigens are phagocytosed into the cell and enclosed within a phagosome
5.
The phagosome fuses with the endosome
6.
Enzymes within the endosome cut up exogenous antigens into peptides
7.
A peptide replaces the CLIP at the groove of the MHC class II molecule
CLIP: class II associated invariant chain peptide (the piece of the invariant chain which is associated with the MHC binding groove)
8.
The MHC II-peptide complex is transported from the Golgi complex to the cell surface for display
Compare and contrast antigen recognition by B and T lymphocytes and by CD4+ and CD8+ T lymphocytes
B lymphocytes
Have surface BCRs (surface Ig receptors)
Recognise intact extracellular antigen directly
T lymphocytes
Have surface TCRs
Recognise processed antigen presented at the cell surface by MHC molecules
Immunology 7: Effector T-lymphocytes
Functions of T cell mediated immunity:
Detection and elimination of intracellular pathogens (i.e. viruses, bacteria, intracellular parasites)
Elimination of altered cells (i.e. tumour cells)
Lymphocyte recirculation:
Lymphocytes recirculate from the blood and lymph to lymphoid organs
They enter lymph nodes across high endothelial venules (HEVs) in the cortex
HEVs: specialised areas in post-capillary venules where there are high endothelial cells which allow lymphocytes to exit the blood
This increases the likelihood that naïve lymphocytes will encounter antigen and become activated
Naïve T cells: mature recirculating T cells which have not yet encountered their cognate antigen
Only recirculate in secondary lymphoid organs; must be activated to enter non-lymphoid tissue
Migration of T cells into secondary lymphoid organs is mediated by receptors presented on the surface of the T cells (e.g. L-selectin)
Activated in secondary lymphoid organs (i.e. lymph nodes)
Effector T cells: mature T cells which have encountered their cognate antigen and proliferated and differentiated into cells which exert immune effector functions
CD8 + CTLs: class I restricted; target virus-infected cells
Recognise peptides of intracellular pathogens presented by MHC class I molecules on the surface of target cells
Cytotoxic: secrete granules which kill target cells
CD4 + Th1 cells: class II restricted; target macrophages
Recognise peptides presented by MHC class II molecules on the surface of target cells
Activate macrophages and cause inflammation
Secrete cytokines: IL-2, IFNγ and TNF-ß
CD4 + Th2 cells: class II restricted; target B cells
Recognise peptides presented by MHC class II molecules on the surface of target cells
Stimulate B cells to differentiate into plasma B cells which secrete antibodies
Secrete cytokines: IL-4, IL-5, IL-6, IL-10 and IL-13
Target cells: cells which are acted on by T cells
Activation of naïve T cells:
Naïve T cells are activated by cross-linking of TCRs by MHC-peptide complexes on the T cell surface
Activation of naïve T cells requires 2 signals:
1.
Antigen recognition: TCRs must recognise their cognate antigen presented by the appropriate MHC molecules
2.
Co-stimulation: co-stimulatory molecules on the surface of an APC (e.g. B7 proteins) must ligate CD28 receptors on the surface of the T cell
Co-stimulation of naïve T cells amplifies the signal sent to the nucleus by engaged TCRs; therefore fewer
TCRs need to be cross-linked to activate the T cell in the presence of co-stimulation
Effector T cells are less dependent on co-stimulation than naïve T cells
T cell activation:
1.
Naïve T cells enter lymph nodes across HEVs
2.
Naïve T cells monitor antigen presented by APCs (activated dendritic cells and macrophages) in lymph nodes
3.
Naïve T cells are activated when they encounter their cognate antigen and receive co-stimulation
(Naïve T cells which do not encounter their cognate antigen leave the lymph node through lymphatic vessels and continue recirculation)
4.
Activated naïve T cells proliferate and differentiate into a clone of effector T cells with the same specificity (i.e. they express the same TCR on their surface and are specific to the same antigen)
5.
Effector T cells enter the circulation and migrate to the site of antigen in peripheral tissues
6.
Effector T cells are activated when they encounter their cognate antigen
7.
Activated effector T cells exert effector immune functions
Resting T cells: express a moderate-affinity IL-2 receptor consisting of ß and γ chains
Activated T cells: express a high-affinity IL-2 receptor consisting of α , ß and γ chains; secrete IL-2
IL-2 secreted by activated T cells binds to the IL-2 receptor and stimulates T cell proliferation
Outline the importance of antigen presenting cells in the induction of T lymphocyte responses
Antigen presenting cells (APCs): express high levels of MHC molecules and co-stimulatory molecules which are required for T cell activation
Co-stimulation: usually involves B7 proteins on the surface of APCs which ligate CD28 receptors on the surface of T cells
APCs include:
Activated dendritic cells (DCs)
Activated macrophages
Activated B cells
Activated dendritic cells:
DCs are distributed below exposed surfaces
Langerhans cells: a subset of dendritic cells which are found below the epidermis
Immature DCs in uninfected peripheral tissues: express low levels of MHC molecules and B7 proteins; therefore they cannot function effectively as APCs
When there is a microbial invasion of peripheral tissues immature DCs are activated by: o Cytokines released by other immune system cells (e.g. TNF) and/or chemicals released by dying cells o Ligation of their pattern-recognition receptors (e.g. Toll-like receptors) by PAMP
Activated DCs travel to lymph nodes, mature and activate naïve T cells
Activation of DCs:
1.
Immature DCs become activated when they phagocytose foreign antigen in peripheral tissues
2.
Activated DCs leave the peripheral tissue and migrate to secondary lymphoid tissues (the nearest lymph node)
3.
Activated DCs mature as they travel to lymph nodes
4.
Activated DCs become mature DCs in the lymph nodes: they express high levels of both MHC-peptide complexes and co-stimulatory molecules
Activated macrophages:
Dispersed throughout exposed surfaces
Inactivated macrophages: express low levels of MHC and co-stimulatory molecules; therefore they cannot function effectively as APCs
Activated macrophages: express sufficient levels of MHC and co-stimulatory molecules to function effectively as APCs
Macrophages are activated by: o Cytokines (e.g. IFNγ ) o Ligation of their pattern-recognition receptors (e.g. Toll-like receptors) by PAMP
Activated macrophages do not migrate; they re-stimulate activated T cells at the site of infection in peripheral tissues
Activated B cells:
Naïve B cells: express low levels of class II MHC molecules and B7 proteins; therefore they cannot function effectively as APCs
Naïve B cells are activated by activated T helper cells???
Activated B cells: express high levels of class II MHC molecules and B7 proteins; therefore they can function effectively as APCs for T helper cells
Activated B cells concentrate MHC II-peptide complexes on their cell surface for presentation to T helper cells
Memory B cells play a major role as APCs either late in the initial infection or early in subsequent infections by the same pathogen
Explain the different requirements for the activation of naïve and memory T lymphocytes
Immunological memory:
The immune system recognises and responds to antigen; it can also remember the same antigen upon subsequent encounters
Memory may confer life-long immunity to many infections
It is the basis for successful vaccination
It is the most important consequence of adaptive immune responses
Memory responses are characterised by a faster and stronger immune response which eliminates the pathogen and prevents infection
T cell memory:
In contrast to B cells, T cells do not undergo class switching (i.e. the TCR remains the same) or affinity maturation (the process whereby BCRs increase their affinity for antigen)
Memory T cells are different from naïve T cells
Generation of memory T cells:
Activated naïve T cells proliferate and differentiate into either effector T cells or central memory T cells:
Effector T cells travel to the site of infection in peripheral tissues
After the infection most effector T cells die by apoptosis
Effector memory T cells: some effector T cells remain in the tissues
Central memory T cells remain in the secondary lymphoid organs and the bone marrow
Central memory T cells activate quickly during subsequent attack and mature into effector T cells
2 subsets of memory T cells:
Expression of CD45RA allows differentiation between naïve T cells and memory T cells
Naïve T cells express CD45RA; whereas memory T cells do not express CD45A
Expression of CCR7 (a chemokine receptor) allows differentiation between memory T cells
Expression of CCR7 instructs memory T cells to remain in secondary lymphoid organs
Effector memory T cells (T
EM
) are CCR7 CD45RA -
They display immediate effector function
Central memory T cells (T
CM
) are CCR7 + CD45RA -
They lack immediate effector function; they differentiate into CCR7 stimulation
effector cells after secondary
Briefly outline the function of T helper cells in relation to the cytokines they produce
Th1 and Th2 cells differentiate from a common precursor: naïve CD4 + T cells
Activation of T helper cells:
Requirements for activation of T helper cells:
Recognition of the cognate antigen presented by MHC class II molecules on the surface of an APC
Ligation of CD28 receptors on the surface of the T helper cell by B7 proteins on the surface of an APC
T helper cell activation:
Naïve CD4 + T cells are activated when they encounter their cognate antigen presented by MHC class II molecules on the surface of an APC and receive co-stimulation from the same APC
Activated T cells proliferate to form a clone of cells which have the same specificity
Proliferated T helper cells differentiate and mature into effector T helper cells (either Th1 or Th2 cells) which have a particular cytokine profile
Cytokine secretion by effector T cells:
Effector T helper cells direct a local immune response against a particular pathogen by secreting the appropriate profile of cytokines:
Th1 cytokines: direct production of cells and antibodies which are effective against viral and bacterial infections
Th2 cytokines: direct production of cells and antibodies which are effective against parasitic and mucosal infections
Effector T cell Cytokine Effector function
Th1 cells
IFNγ
TNF
IL-2
Activates macrophages
Stimulates B cells to secrete IgG which is good at opsonisation and at fixing complement
Activates macrophages and NK cells
Stimulates proliferation of CTLs and NK cells
Th2 cells
IL-4
IL-5
Stimulates growth of B cells
Stimulates B cells to secrete IgE which causes degranulation of mast cells
Stimulates growth and differentiation of eosinophils
Stimulates B cells to secrete IgA
Cytokine profiles of activated T helper cells can be reinforced or changed by cytokines at the site of infection:
At the site of a bacterial or viral infection activated macrophages secrete IL-12: this influences T helper cells to secrete Th1 cytokines
At the site of a parasitic infection there is a high concentration of IL-4: this influences T helper cells to secrete Th2 cytokines
Cytokines secreted by committed T helper cells (i.e. effector T helper cells) influence uncommitted Th0 cells (i.e. newly activated T helper cells) to secrete the same profile of cytokines:
Th1 cells secrete IFNγ : this activates macrophages; activated macrophages secrete IL-12 which influences Th0 cells to secrete Th1 cytokines
Th2 cells secrete IL-4: this influences Th0 cells to secrete Th2 cytokines
Committed T helper cells secrete cytokines which result in positive and negative feedback
Positive feedback:
Th1 cells secrete IL-2: this stimulates proliferation of Th1 cells
Th2 cells secrete IL-4: this stimulates proliferation of Th2 cells
Negative feedback:
Th1 cells secrete IFNγ : this inhibits proliferation of Th2 cells
Th2 cells secrete IL-10: this inhibits proliferation of Th1 cells
Describe the effector functions of T lymphocytes including cell-mediated cytotoxicity, macrophage activation, delayed type hypersensitivity and T/B lymphocyte cooperation
Effector functions of T helper cells:
Effector T helper cells coordinate the immune response against infections caused by intracellular pathogens
Effector T helper cells have 2 main functions:
1.
To direct the local immune response (i.e. at the site of infection) by cytokine secretion
2.
To help B cells and CTLs
Cell-mediated cytotoxicity:
CTL precursors (CTL-Ps): naïve CTLs which exert no cytotoxic effector function (i.e. they cannot kill)
CTL-Ps must be activated to differentiate into effector CTLs which are functional
Initial activation requires an interaction between a CTLp and an APC; it is T helper cell-independent
Generation of CTLs:
1.
A CTLp is activated when it encounters its cognate antigen presented by MHC class I molecules on the surface of an APC and receives co-stimulation from the same APC
2.
Activated CTL-Ps migrate to the site of infection in peripheral tissues
CTL-Ps require an external supply of IL-2 to proliferate in peripheral tissues
3.
Th1 cells secrete IL-2 at the site of infection: this stimulates activated CTL-Ps to proliferate
4.
Proliferated CTL-Ps differentiate into effector CTLs which exert effector cytotoxic function
Effector cytotoxic function of CTLs:
Effector CTLs become polarised when they encounter their cognate antigen presented by MHC class I molecules on the surface of a target cell (e.g. virus-infected cells)
Polarisation results in redistribution of the cytoskeleton and cytoplasmic components within CTLs: granules migrate to the site of TCR-MHC I-peptide interaction at the plasma membrane
CTLs release their granules at the site of cell-cell contact after recognition of the target cell
CTLs kill a target cell by inducing apoptosis:
1.
The CTL recognises and binds to its cognate antigen presented by MHC class I molecules on the surface of a virus-infected cell
2.
The CTL programs the target cell for death by inducing DNA fragmentation
3.
The CTL migrates to a new target cell
4.
The original target cell dies by apoptosis
2 pathways of cell-mediated cytotoxicity:
1.
Granules
2.
Fas-FasL interactions
Granules: contain cytotoxic effector molecules which trigger apoptosis
Perforin: perforin molecules polymerise to form a pore in the plasma membrane of the target cell
Perforin helps a CTL to deliver granzymes into the cytoplasm of the target cell
Granzymes: serine proteases which induce apoptosis once they are in the cytoplasm of the target cell
Granulysin: induces apoptosis in the target cell
Fas-FasL interactions:
CTLs have Fas ligands (FasL) on their surface which can bind to Fas proteins on the surface of a target cell
Fas-FasL interactions induce apoptosis in the target cell
CTLs also release cytokines which contribute to host defence by amplifying the immune response:
IFNγ : inhibits viral replication; activates macrophages
TNFα and TNF-ß: synergise with IFNγ receptors
N.B. CTLs are recycled
Macrophage activation:
Macrophages must interact with Th1 cells in order to be activated
Requirements for macrophage activation:
TCR-MHC II-peptide interaction: a TCR on the surface of a Th1 cell recognises and binds to its cognate antigen presented by MHC class II molecules on the surface of a macrophage
CD40-CD40L interaction: CD40L on the surface of a Th1 cell ligates CD40 on the surface of a macrophage
Cytokine interaction: Th1 cells secrete cytokines (IFNγ ) which bind to IFNγ receptors on the surface of a macrophage
Cytokine mediated interactions between naïve CD4 + T cells and macrophages:
APCs secrete IL-12: this activates naïve CD4 differentiate into a clone of Th1 cells
+ T cells and stimulates them to proliferate and
Th1 cells secrete IFNγ : this activates macrophages
Delayed type hypersensitivity (DTH): an inflammatory reaction in which T helper cells recognise a specific pathogen and secrete cytokines that activate and recruit cells of innate immunity to kill the pathogen
Functions:
Primary role in defence against intracellular pathogens by eradication of the pathogen
If the pathogen is not eradicated, it is contained by chronic stimulation and granuloma formation
Hypersensitivity: if the antigen is not a microbe, DTH produces tissue injury without protection as in contact hypersensitivity (CHS)
DTH may be protective as well as pathological
2 phases of DTH:
1.
Sensitisation phase
2.
Effector phase
Tuberculin hypersensitivity:
Clinical appearance: firm red swelling of the skin which is maximal 48-72 hours after injection
Histological appearance: there is a dense dermal infiltrate of leukocytes and macrophages
T/B lymphocyte cooperation:
T helper cell dependent activation of B cells requires cell-cell contact and cytokines
See “Immunology 5”
Beneficial and deleterious actions of effector T cells:
Clearance of the pathogen: effector T cells recognise antigenic peptide derived from foreign pathogens
Effector T cells may cause pathological reactions:
Autoimmunity: effector T cells recognise antigenic peptide derived from self proteins
Rejection (of transplants): effector T cells recognise antigenic peptide derived from proteins of the transplant donor
Regulatory T cells: T cells which regulate the activation or effector functions of other T cells
A subset of CD4 + T cells
Have a relatively high affinity for MHC II-self peptide complexes: it may be necessary to maintain tolerance to self antigens
Control immune responses: suppress the immune response to self antigens o Secrete cytokines (IL-10 and TGF-ß) which inhibit T cell responses o Cell-cell contact inhibits T cell responses
Immunology 8: Host Defence Overview
Name the important components of the immune system
Summarise and give examples of the roles taken by: physical or chemical boundaries; mechanical removal; innate immune responses
Define and contrast: innate and adaptive/acquired immunity; humoral and cellular immunity; attributes of specific immunological memory
Appreciate special features of immune reactions at mucosal sites
Understand the sequence and timing of events during acute infection
List defence mechanisms operative against viruses and bacteria