Immune cells in the lung - Lungeninformationsdienst
advertisement
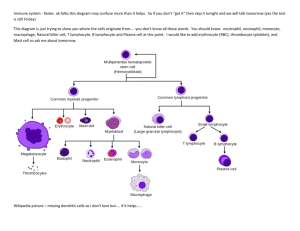
Immune cells in the lung Nunja C. Habel-Ungewitter & Sabine Bartel 12.11.14 immunity • from immunis, Latin for "exempt“ • capability of the body to resist harmful microbes from entering it • Immunity involves both specific and nonspecific components immunity Innate vs. adaptive immunity Innate immune system Adaptive immune system non-specific response pathogen and antigen specific response highly conserved pattern recognition receptors (PRRs) immediate maximal response (hours) highly specialized, variable receptors lag time between exposure and maximal response (days) cell-mediated and humoral components no immunological memory cell-mediated and humoral components found in nearly all forms of life found only in jawed vertebrates immunological memory Adaptive immune response Innate and adaptive immunity Innate • skin/mucosal tissues • Complement System • Antimicrobial Peptides • Phagocytes (Macrophages, PMNs, Monocytes, DCs) • Adaptive Immune System Activation Acquired (Adaptive) • B Lymphocytes -Antibodies • T Lymphocytes -Cytotoxicity -Cytokine Secretion -B cell Activation The immune system: overview Antigen presentation Complement system Complement system "Janeway's Immunobiology" Lymphatic organs Tonsils and adenoids Lymph nodes Lymphatic vessels Thymus Lymph nodes Spleen Peyer’s patches Appendix Lymph nodes Bone marrow Primary lymphatic organs: Lymphatic vessels generation of lymphocytes bone marrow, thymus Secondary lymphatic organs: initiation of adaptive immune responses lymphnodes, spleen;MALT Haematopoetic system Macrophages – frontline of innate immune defense J Clin Invest. 2002;110(11):1603-1605. doi:10.1172/JCI17302 Macrophages • Named by Elie Metchnikoff : „microorganims can be engulfed and digested by phagocytic cells“ • Progenitor in the blood: monocytes – Different in the lung: self renewal, proliferation • Resident in tissue – Alveoli alveolar macrophages – interstitium • Relatively long-lived (ca. 40% in 1 year) • Frontline/first line of antigen recognition and defense ! Macrophages - scavengers © Dr Dennis Kunkel • Professional phagocytes: engulf and kill invading pathogens (microorganism, particles) cell debris and infected cells distinguish between „dangerous“ and „harmless“ antigens • Equipped with pattern recognition receptors and can rapidly produce proinflammatory cytokines and chemokines Bliska&Casadevall Nat. Reviews Microbiology2009 Depletion of alveolar macrophages impairs neutrophil emigration after LPS impaired neutrophil evasion after alveolar macrophage depletion (open bars) in response to intratracheal LPS stimulation Maus et al., AJP Lung 2002 Recruitment of immune cells by macrophages Monocytes • 5-8 % • many lysosomes • Differentiate into lung DC and Macrophages lung M PBMo lung DC Recruitment of monocytes Granulocytes/polymorphonuclear leukocytes • Cytoplasmic granules • Irregularly shaped nuclei • Short lived Neutrophils (PMN) • The main effector of innate immunity (55-70%) • Phagocytes • Kills the pathogens mainly by ROS and enzymes (e.g., neutrophil elastase) • 2 types of vesicles: 1) lysosomal enzymes 2) collagenase and lactoferrin (toxic) • Become apoptotic after some hours to days or after phagocytosis of pathogen Leukocyte emigration to the lung: Adhesion molecules Neutrophils-NETosis • Release of granule proteins and chromatin extracellular fibers bind gram-pos. and –neg. bacteria • NETs: neutrophil extracellular traps degradation of virulence factors, kill bacteria Neutrophil Extracellular Traps Kill Bacteria ; Brinkmann et al. Science 2004 immunopaedia.org Neutrophils-NETosis A) Inactive neutrophils B) active neutrophils E) extracellular NETs Bacteria trapped in NETs A) Staphylococcus aureus B) Salmonella typhimurium Young et al. PlosONE 2011 • 2-5% of leukocytes • Granules: enzymes & toxic proteins • Important for defense against parasites • MBP: major basic protein • Attack surfaces that are marked with IgE (cells or parasites) • Involved in allergic inflammatory reactions • Also important role in attacking the mucosa and the airway epithelium in asthma www.laborlexikon.de Eosinophils Eosinophils – Asthma bronchiale Bronchus Knochenmark Antigen Mastzelle Eosinophiler Granulozyt TH 2-Zelle BronchialSchaden Interleukin-4 GM-CSF Interleukin-5 Histamin Leukotriene IL-4, IL-13 Granula-Proteine Leukotriene Verlängertes Überleben IL-13 Chemokine (RANTES, Eotaxin, MCP-1, MIP-1α ) Selektin VCAM-1 ICAM-1 Diapedese Adhäsion Endothelium Blut NEJM 344, 350-362, 2001 Basophils • Less than 1% of Leukocytes • Contain histamine and heparin • Proteolytic enzymes • Fast immune reaction; external antigens (asthma, hay fever) Mast cells • only in tissue and mucosa • bind IgE on their surface • degranulate among antigen contact and release histamin, leukotrienes etc. from their granulas • main cells which confer acute allergic symptoms (swelling, bronchial obstruction) in acute asthma etc. Mast cells - activation Bischoff 2007 Asthma bronchiale cross-linking of membrane-bound IgE by allergenes Activation Release of: histamine, leukotrienes, proteoglycans cytokines (IL-1,2,3,4,5, TNF-α, GMCSF) early response bronchial spasm oedema bronchial obstruction late response mucosal inflammation bronchial obstruction bronchial hyperreactivity development of matrix Dendritic cells (DC) • Myeloid and lymphoid progenitors (small subpopulation); lat. dendriticus = branched (verzweigt) • Key cells: link innate with adaptive immunity • Immature DCs: phagocytic - enter tissue & mature after pathogen encountering Lambrecht & Hammad, 2003 Dendritic cells Main function: Antigen presenting cell (APC) Lambrecht & Hammad, 2003 Dendritic cells • Secondary immune response: Lambrecht & Hammad, 2003 Dendritic cells • Mature DCs shape t-cell response (Hammad & Lambrecht, J Allergy Clin Immunol 2006) : • Which type of t-cells is activated? • Different Ils or different concentrations • Defines tolerance vs. Immunity • Immature DCs cannot activate naive T cells. Dendritic Cells (DC) pattern recognition receptors (TLR 2,4,7,9...) integrins (CD11b, CD11c) MHC class II maturation antigen presentation MHC class II co-stimulatory CD80/CD86 phagocytosis capacity T cell stimulation antigen uptake immature DC mature DC Antigen presentation via MHC-molecules MHC= major histocompatibility complex; repertoire differs between individuals MHC Class II MHC Class I CD8+ CD4+ Killing Activation Endogenous Antigens MHC I: ubiquitous expr. Exogenous Antigens MHC II: professional APC Antigen presenting cells MHCII expression : Constitutive on all professional APCs costimulatory molecules – present to CD4+ helper T-cells – HLA-DR, DP, DQ MHC I expresion: Constitutive on all nucleated cells – present to CD8+ cytotoxic T-cells – HLA (Human Leukocyte Antigen)A, B, C Peptide loading of MHC molecules Phagocytosis Endocytic pathway Postranslational modifications Secretory pathway Cross presentation of soluble antigen on MHC class I Mainly in dendritic cells => activation and recruitment of CD8+ T cells Interaction of MHC- molecules with T-cell receptors Small T-cell subpopulation: γδ-TCR => much less variable repertoire: 103 vs. 1015 (αβ) Interaction of MHC- molecules with T-cell receptors Signals required for activation: 1. Antigen-specific binding TCR-MHC 2. Co-stimulatory molecules (e.g. CD28 interaction with CD80/CD86 (B7) or ICOS with ICOS-L) 3. Cytokines (IL-4, -15, -12 or TGF-ß) Gutcher et al., JCI, 2007 Haematopoetic system T lymphocytes T lymphocytes Helper T cell (Th-CD4+) Activated helper T cell – “The Bureaucrat” – Directs other cells – Uses cytokines as its “memos” Cytotoxic T cell (Tc-CD8+) Activated killer cell – “The Hitman” – Kills on contact – Also produces cytokines (IFN-, TNF-a) T helper cells T helper cells T helper cell subtypes Dysbalance between the subtypes => (chronic) imflammatory diseases Février et al., Viruses, 2011 Cytotoxic T cells Regulatory T cells Regulatory T cells Effector T cells homeostasis inflammation inflammation Image derived from Bouma & Strober et al., Nature Reviews Immunology, Regulatory T cells Mode of action Valadi et al., Nature Reviews Immunology, 2008 B lymphocytes Establishment of a first, antibody-mediated immune response: ~ 7days Secondary immune response: ~3 days en.wikipedia.org Antibodies Antibody functions austincc.edu Antibody classes Thank you for your attention! „Es war einmal das Leben“, Albert Barillé, 1978-1995