ch21_notes
Ch. 21 Notes: Immune System
Innate Defenses
Adaptive Defenses
Ch. 21 Notes: Immune System
I. Innate Defenses
Surface defenses: Skin & mucous membranes, first line of defense
Skin & mucous membranes are physical barriers to entry
Protective chemicals on skin & mucous membranes
Innate internal defenses: Cells & chemical defenses, 2 nd
line of defense
Phagocytosis (neutrophils, macrophages)
Natural killer cells
Fever
Kill virally-infected & cancerous cells before adaptive defenses kick in
“Hypothalamic thermostat” resets to a higher temp
Activates heat-generating & heat-conserving mechanisms
Higher temp may lead to greater biochemical activity of defensive systems (but also of pathogens?)
Higher temp may cause sequestration of Fe & Zn which may slow bacterial growth
Inflammation
Signs: heat, redness, swelling, pain – what causes these?
Steps in inflammation – see figure
Antimicrobial defenses
Interferons
Interfere with viral replication - know how
Complement
System of plasma proteins which, when activated, can kill target cells and can help activate other defensive systems
Multiple ways to activate complement system: Classical, alternative, & lectin
Adaptive Defenses
Antigens
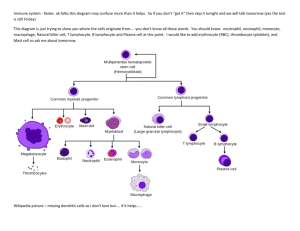
Lymphocytes & antigen-presenting cells (APCs)
B lymphocytes (B cells)
T lymphocytes (T cells) (subtypes: helper T, cytotoxic T, regulatory T, memory T…)
APCs: dendritic cells, macrophages. B cells can act as APCs.
How & where do B cells & T cells develop?
What are the different functions of B & T cells?
Developing mymphocytes are “screened” as they mature to make sure they are immunocomptent
(can recognixze & respond to antigens) and self-tolerant (i.e. do not attack body’s own tissue)
Humoral Immune Response
Mediated by circulating antibodies
Clonal selection of B cells
Only the B cell(s) that recognize the antigen are selected for proliferation (i.e. mitosis to make many copies) and differentiation (i.e. making specialized daughter cells including plasma cells and memory B cells)
Role of plasma cells
Role of memory B cells
Primary & secondary immune responses: Why is secondary response faster & bigger?
Vaccines: Work by “priming the system” or “creating a memory”, so that if/when we get infected, we have a secondary response , i.e. a big & fast response
Active vs passive humaopral immunity
Natural vs acquired humoral immunity
Antibody structure
See the figure
Variable & constant regions
Tips of the Y are the antigen binding sites. The 2 tips match.
Five antibody classes:
IgM (pentamer) first to appear in large numbers in a new response; causes agglutination
IgA (dimer) mucous membranes, tears, saliva, etc. “Surface” defense
IgG (monomer) most common type in plasma most of the time
IgE (monomer) defense against parasitic worms; causes allergic responses
IgD (monomer) on surface of B cells
How antibodies help
Neutralization, agglutination, precipitation, complement fixation & activation of complement system – know what these mean
Cellular Immune Response
Mediated by T cells
CD4 cells and CD8 cells
When activated, CD4 cells usually become helper Ts
When activated, CD8 cells usually become cytotoxic Ts
Antigen presentation and MHC proteins
Class I MHC proteins found on all cells (except RBCs) in body
Display antigens from within the cell – fragments of what’s inside the cell
CD8 cells are activated if/when they bind to an antigen that matches their antibody, and if (only if) the CD8 molecule recognizes the presence of the MHC I protein presenting the antigen
Class II MHC proteins found on APCs
Present antigens from ingested foreign objects that the APC has “eaten” by phagocytosis
CD4 cells are activated if/when they bind to an antigen that matches their antibody, and if (only if) the CD4 molecule recognizes the presence of the MHC
II protein presenting the antigen
T cell activation & differentiation
See figure
T cell must recognize the antigen (i.e. antigen must match the antibody on that T cell) and the T cell must recognize the MHC protein that is presenting the antigen (CD4 cell must
“see” an MHC II protein; CD8 cell must “see” an MHC I protein)
Co-stimulation from the APC also required for T cell activation
Clonal selection of T cell: the activated T cell then divides many time by mitosis to make active daughter cells. Daughter cells differentiate to become helper Ts, regulatory Ts, memory Ts, cytotoxic Ts. Which type they become depends partly on whether the cell was a CD4 or CD8.
Cytokines: chemicals that amplify the immune reposnse. Interferons, interleukins.
Know what helper Ts, cytotoxic Ts, regulatory Ts do.
Organ transplantation
Blood easiest to transplant because RBCs don’t have MHC proteins on surface – only need to match A, B, & Rh antigens
For other organs: match as many as possible of the MHC proteins. Some are more important to match than others.
Autograft – from self
Isograft – from identical twin
Allograft – from another person, not a twin
Xenograft – rom another species
Immune System Challenges and Dysfunction
Immunodeficiency diseases
AIDS (stands for what?)
Infection by HIV
HIV preferentially infects & kills helper T cells
Helper Ts are essential for both humoral and cellular immune responses, so knockout of helper Ts leaves patient extremely vulnerable to infection
Patients often succumb to opportunistic infections (infections that wouldn’t stand a chance against a normal immune system)
Severe combined immune deficiency
Genetic defect (inborn error of metabolism)
Hypersensitivity diseases
Mounting an immune response against something that is not a major threat
Immediate hypersensitivity (allergic response)
Antigen binding to IgE is involved; histamine release from mast cells
Subacute hypersensitivity response
Delayed hypersensitivity response
Autoimmune diseases
Immune system attacks body’s own tissues
More specifically, lymphocytes mistake body tissues for “foreign antigens” & mount an attack
Type I diabetes: beta cells of the pancreas get attacked & wiped out
Rheumatoid arthritis: synovial membrane of joints gets attacked & damaged & scarred
Copyright © 2015, William C. Rose