Cases-Who Should Decide - Providence Health Care
advertisement
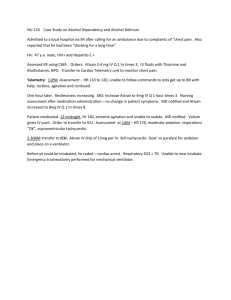
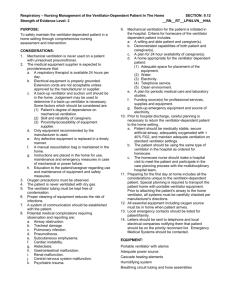
Cases-Who Should Decide? Case #1- Competent but ‘different’ Mary is 75yrs old, long estranged from her husband and has been living an independent and reclusive life for many years. She does not keep in touch with her two children or any friends. She has been diagnosed with metastatic colon cancer and declined anything more than minimal home support. She is admitted after being found by a Visiting Nurse on the floor from a fall. The staff believes that she belongs in a long term care facility but she adamantly refuses. She wants to go home and continue with palliative home support Case #2-The daughter from ‘hell’ Jack is a 72yr old widower with a long and complicated history of progressive heart failure. He has been living in a rural area with a son, Tom, who has been very involved in his care. Jack and Tom have had their nightly tea together for the last three years. Jack has spoken often about the death of friends and how he would “like to go at the end”. After an acute deterioration Jack is resuscitated, intubated and admitted to the ICU of the regional hospital. Tom is told that his father will not recover and to prepare for his death. Tom informs his sister, Martha, an accountant in Toronto, that she should come home to say good-bye. She has not been to visit in over two years. She is very angry at the plan to discontinue the ventilator and threatens to sue if that occurs. Jack has no advance directive; Martha is the eldest child. Case #3-Unilateral DNR Samuel Golubchuk was an 84 yr old long term care resident with a complex history of illness and brain damage at the Deer Lodge Care Facility when he was admitted to the ICU of the Winnipeg Salvation Army General Grace Hospital with pneumonia and pulmonary hypertension. Initially, he was placed on a ventilator. After assessment, the ICU physicians determined that further medical intervention was of no benefit and recommended that ventilator and life supports should be withdrawn. Mr Golobchuk’s family believed that Jewish law prohibited discontinuation of ventilatory support. ICU physicians then claimed that it was unethical to continue medical interventions here as they were doing harm (e.g.trying to surgically treat bed sores) and providing no benefit. The College of Physicians of Manitoba issued Statement No 1602 Withholding and Withdrawing Life-Sustaining Treatment indicating that while consultation with the family in these cases was necessary, the ultimate decision about discontinuation of life support was the doctor’s. Case #4-Adolescents Tom is a 14yr old who has just been diagnosed with early-stage Hodgkin’s lymphoma. He has been acting out and truant since his father abandoned him and his mother two years ago. He is refusing to participate in treatment even though he has been assured of a 90% probability of cure. Andrea is a 12yr old with cystic fibrosis. She has had a very stormy course with frequent hospitalizations, intensive care admissions and long periods of ventilator support. She has become increasingly non-compliant with therapy and tells you she wants to “stop all this.” She wants to be sure that the next time she deteriorates she is not put back on the ventilator.