Cummings
advertisement

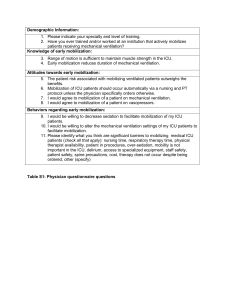
Early Mobilization of LVAD Recipients Christiane S. Perme, PT, Robert E. Southard, MD, David L Joyce, MD George P Noon, MD, Matthias Loebe, MD, PhD Tex Heart Inst J. 2006; 33(2): 130–133. Conclusions/Clinical Significance Abstract Early mobilization and aggressive physical therapy are essential in patients who receive left ventricular assist devices (LVADs) due to long-term, end-stage heart failure. Some of these patients remain ventilator dependent for quite some time after device implantation. We report our regimen of mobilization with the aid of a portable ventilator, in patients with cardiac cachexia and LVAD implantation. Further, we describe the specific physical therapy interventions used in an LVAD patient who required prolonged mechanical ventilation after device implantation. The patient was critically ill for 5 weeks before the surgery and was ventilator dependent for 48 days postoperatively. There were significant functional gains during the period of prolonged mechanical ventilation. The patient was able to walk up to 600 feet by the time he was weaned from the ventilator and transferred out of the intensive care unit. He underwent successful heart transplantation 6 weeks after being weaned from the ventilator. We believe that improving the mobility of LVAD patients who require mechanical ventilation has the potential both to facilitate ventilator weaning and to improve the outcomes of transplantation. The concept of early intervention of rehab for patients in the ICU is significantly important to physical therapist. Articles like this, and others provided proof of the impact physical therapy plays on critically ill patients and improving quality of life and functional status. The more research that is done in this field the more insurance will be compelled to reimburse for skilled services as well as provides hospitals with data that demonstrates physical therapies effectiveness. It also allows physical therapist the opportunity to have the most current information to practice with the best evidence based medicine. Background/Introduction Further research has been done in the area of skilled physical therapy involvement with patients who are critically ill and on mechanical ventilation. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial, is an article that supports the case study. This article has good quality support of the first article due to the fact the it is a randomized control study. The population for the study was ICU patients who were on mechanical ventilation and the size for the article was significant enough with 104 patients. The intervention group received physical and occupational therapy , while the control group only received what the physician ordered. In the study researchers found that patients in the intervention group had a shorter duration of ICU associated delirium by 2•0 days and spent 2•4 more days alive and breathing without assistance than did controls. Researchers also looked at other outcomes such as ability to complete ADL, hand grip, walking distance, and how long it took the patients to reach certain milestones in the hospital all of which were in favor of the intervention group. LVAD are implanted when a person is at end-stage heart failure, but are not eligible for a heart transplant. Theses patients are often severely deconditioned and have to be placed on mechanical ventilation secondary to respiratory failure. Patients are often put on bed rest in the ICU after undergoing LVAD leading to significant loss of function. In addition patients who remain on mechanical ventilation are prone to high costs of care, poor functional outcomes, and high morbidity rates. The concepts behind this case study are that early intervention of a physical therapy programing the ICU that focuses on early mobilization and ambulation will improve over all strength and endurance as well as assist in weaning the patient off mechanical ventilation. Purpose There is a lack of research on the effects of early intervention on LVAD patients. Researchers intend to see how effective early mobilization and ambulation through physical therapy treatment is at assisting with ventilator weaning and improving over all strength and endurance. Methods and Materials This case is a 51-year-old man was admitted to the hospital with HF due to dilated cardiomyopathy and a right lower lobe nodule. During the 5 weeks after hospital admission, the patient's condition progressively worsened despite optimal inotropic and intra-aortic balloon pump support. He developed renal insufficiency and respiratory failure that required mechanical ventilation. During this period, the patient was on bed rest and dependent upon help with all ADL’s. The patient underwent insertion of a VAD and right lower lobe wedge resection of a pulmonary granuloma. The postoperative period was complicated by multiple medical problems, which included respiratory failure that led to prolonged mechanical ventilation. The patient was referred PT on postoperative day 7, after the 1st ventilator weaning trial failed. Following a complete PT evaluation, treatments were initiated. These included lower-extremitystrengthening exercises and mobilization: sitting on the edge of the bed, standing at the bedside, and moving from the bed to a chair. Once the patient was able to stand safely with a walker and assistance, gait-training activities were initiated around the bed and progressed to the hallway in the ICU. The patient was mobilized and started walking while still on the ventilator. Aggressive early PT was provided in order to enhance the overall recovery of this multimorbid patient. The POC was the standard protocol from the cardiovascular ICU at The Methodist DeBakey Heart Center, Houston. References -Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. May 30 2009;373(9678): 1874-1882 Fig 2: Perme, 2006 Results Patient stayed in the ICU for 49 days and was ventilator dependent for 48 days. The patient received 25 daily physical therapy sessions. Sessions included Lower-extremity exercises: 17 sessions, sitting on edge of bed: 22 sessions, standing: 21 sessions, gait training with walker: 18 sessions. A portable ventilator was used in 4 gait-training sessions, and it enabled a significant increase in distance walked, as well as improvement in activity tolerance. After this, the patient was able to start trials of spontaneous breathing while off the ventilator, with supplemental oxygen provided by a tracheostomy. He subsequently tolerated ambulation without ventilatory support, and progressed rapidly with the ventilator-weaning process. It is important to consider that this patient was critically ill during the 5 weeks preceding LVAD implantation. Despite this, the patient showed substantial functional gains during the period of prolonged mechanical ventilation and bed rest after LVAD implantation. Upon transfer from the ICU, the patient required minimal assistance for out-of-bed activities and was able to walk 600 feet with the aid of a rolling walker and supervision. After 6 weeks in acute care, the patient underwent successful heart transplantation. The patient was discharged from the hospital but has had recurrent respiratory problems that have led to hospital readmissions. -- Rogers JG, Aaronson KD, Boyle AJ, et al. Continuous flow left ventricular assist device improves functional capacity and quality of life of advance heart failure patients. Journal of the American College of Cardiology. April 27 2010; 55(17): 1826-1836 Another study that adds evidence to patients with left ventricular assist devices improving with therapy is Continuous Flow Left Ventricular Assist Device Improves Functional Capacity and Quality of Life of Advanced Heart Failure Patients. In this retrospective cohort study researchers looked at a total of 655 patients who had recently had a left ventricular assist device implanted due to end stage heart failure. Researcher used three measurements to assess quality of life and functional status. Subjects improved distances on the 6-min walk test, scores on the quality of life questionnaire(MLWHF) and patient activity scores increased significantly. Summary Discussion The implementation of an early physical therapy program with focus on early mobilization and ambulation is essential to minimize functional decline. This therapy is well accepted by patients, physicians, nurses, therapists, and family members. It appears to improve functional outcomes by optimizing cardiopulmonary and neuromuscular status, as well as by maximizing independence. In this patient, the improvement in overall strength and endurance may have facilitated weaning from mechanical ventilation. Early mobilization and ambulation of patients who require prolonged mechanical ventilation contributes to higher functional capability and an improvement in patients' quality of life. early physical therapy can significantly improve the outcomes of subsequent transplantation for selected mechanically ventilated LVAD patients. Based on the best current evidence it can be concluded that early intervention and mobilization of patients who are on mechanical ventilators in the ICU by skilled physical therapist accelerate several parts of the healing process and improve quality of life and functional status. The benefits of early physical and occupational therapy are not limited to ventilation patients either. According to research from these articles the majority of patients in the ICU make great improments when their plan of care includes rehab intervention early on. Poster by Tony K Cummings, DPT Student