HPHS Patient Medical History Form
advertisement
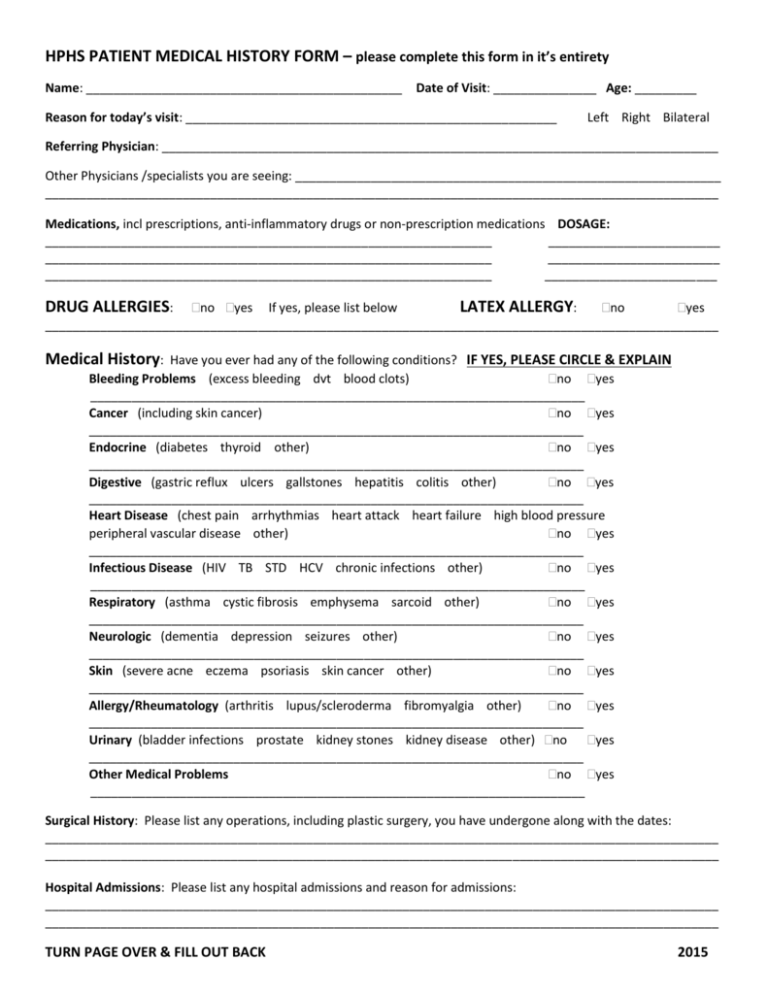
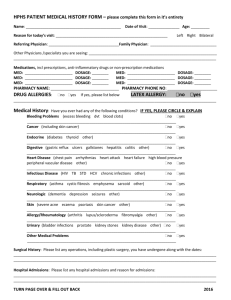
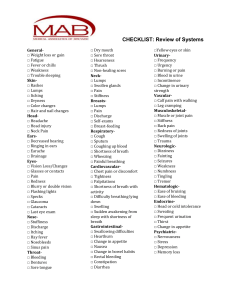
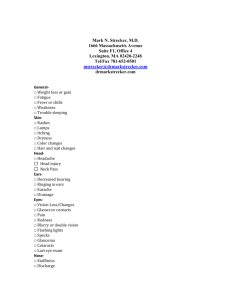
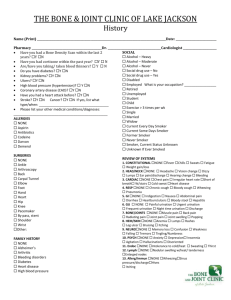
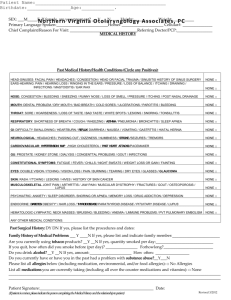
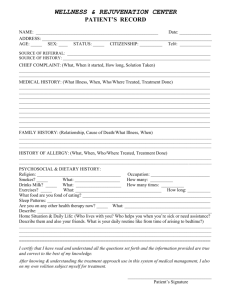
HPHS PATIENT MEDICAL HISTORY FORM – please complete this form in it’s entirety Name: ______________________________________________ Date of Visit: _______________ Age: _________ Reason for today’s visit: ______________________________________________________ Left Right Bilateral Referring Physician: _________________________________________________________________________________ Other Physicians /specialists you are seeing: ______________________________________________________________ __________________________________________________________________________________________________ Medications, incl prescriptions, anti-inflammatory drugs or non-prescription medications DOSAGE: _________________________________________________________________ _________________________ _________________________________________________________________ _________________________ _________________________________________________________________ _________________________ no yes If yes, please list below LATEX ALLERGY: no yes __________________________________________________________________________________________________ DRUG ALLERGIES: Medical History: Have you ever had any of the following conditions? IF YES, PLEASE CIRCLE & EXPLAIN Bleeding Problems (excess bleeding dvt blood clots) no yes ________________________________________________________________________ Cancer (including skin cancer) no yes ________________________________________________________________________ Endocrine (diabetes thyroid other) no yes ________________________________________________________________________ Digestive (gastric reflux ulcers gallstones hepatitis colitis other) no yes ________________________________________________________________________ Heart Disease (chest pain arrhythmias heart attack heart failure high blood pressure peripheral vascular disease other) no yes ________________________________________________________________________ Infectious Disease (HIV TB STD HCV chronic infections other) no yes ________________________________________________________________________ Respiratory (asthma cystic fibrosis emphysema sarcoid other) no yes ________________________________________________________________________ Neurologic (dementia depression seizures other) no yes ________________________________________________________________________ Skin (severe acne eczema psoriasis skin cancer other) no yes ________________________________________________________________________ Allergy/Rheumatology (arthritis lupus/scleroderma fibromyalgia other) no yes ________________________________________________________________________ Urinary (bladder infections prostate kidney stones kidney disease other) no yes ________________________________________________________________________ Other Medical Problems no yes ________________________________________________________________________ Surgical History: Please list any operations, including plastic surgery, you have undergone along with the dates: __________________________________________________________________________________________________ __________________________________________________________________________________________________ Hospital Admissions: Please list any hospital admissions and reason for admissions: __________________________________________________________________________________________________ __________________________________________________________________________________________________ TURN PAGE OVER & FILL OUT BACK 2015 Review of Systems: Constitutional: none Eyes: none Ears: none Nose: none Neck: none Mouth/Throat: none Heart/Lungs: none Digestive: none Urinary none Muscular: none Skeletal: none Neurologic: none Psychiatric: none Skin: none Are you currently experiencing any of the following? If yes, circle weakness fever weight loss weight gain itching excess tearing change in vision or double vision pain ringing buzzing imbalance loss of hearing obstruction bleeding chronic drainage stiffness swelling lumps chronic sores pain difficulty swallowing chest pain palpitations shortness of breath chronic cough heartburn nausea/vomiting constipation diarrhea incontinence retention bleeding swelling weakness difficulty moving leg cramps back pain joint pain stiffness headaches migraines tremors numbness and tingling anxiety depression hallucinations chemical dependency lesions rashes lumps itching Social History: occupation (now or before retirement) ___________________________________________________ recreational activities: ________________________________________________________________________ smoking current every day smoker current some day smoker former smoker never smoked alcohol no yes recreational drugs no frequent occasional social yes ________________________________________________________________ Family History: Please list any major medical problems with parents, grandparents, and/or siblings: __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ Height: ________________ Weight: ____________________ Date of Birth: ___________________ If pertinent, any recent X-rays, CT Scans or MRIs? no yes Date studies performed: _____________________ Location _________________________________________ If pertinent, any recent nerve conduction studies (EMG/NCV)? no yes Date studies performed: _____________________ Location _________________________________________ Females: Date of last mammogram ___________________ Location _________________________________________ Anesthesia: Have you or anyone in your family had a problem with anesthesia: no yes If yes please explain________________________________________________________________________ Patient’s Signature: ____________________________________________ Date: __________________________