Patients Record - Wellness & Rejuvenation Center
advertisement
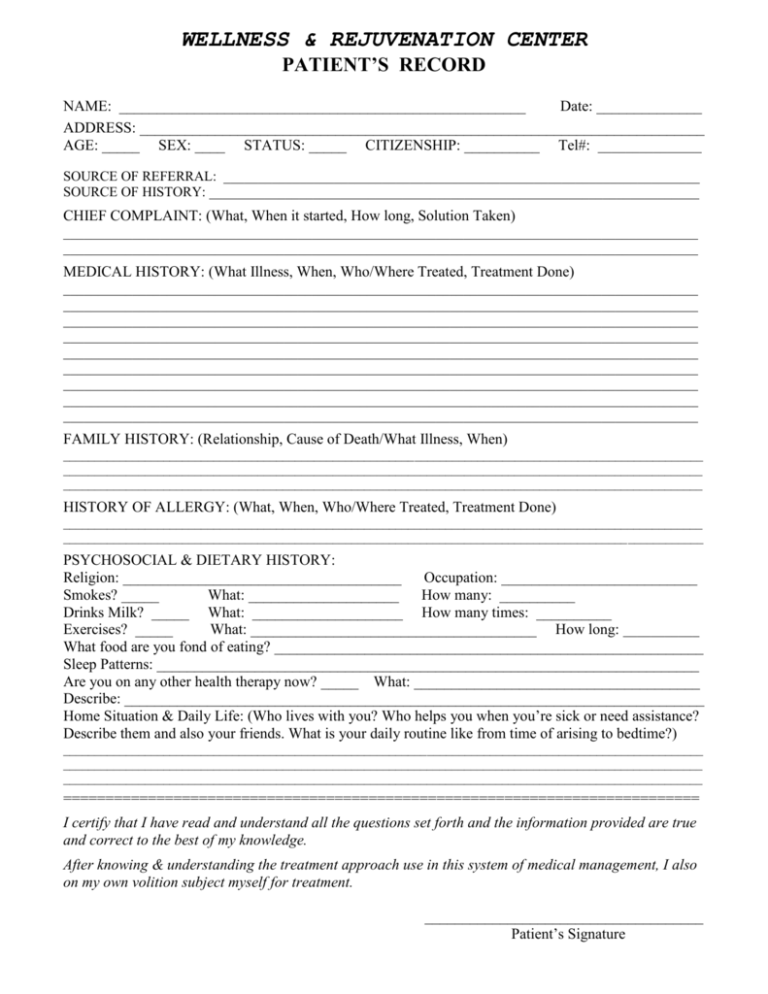
WELLNESS & REJUVENATION CENTER PATIENT’S RECORD NAME: ______________________________________________________ Date: ______________ ADDRESS: ___________________________________________________________________________ AGE: _____ SEX: ____ STATUS: _____ CITIZENSHIP: __________ Tel#: _______________ SOURCE OF REFERRAL: _____________________________________________________________________ SOURCE OF HISTORY: _______________________________________________________________________ CHIEF COMPLAINT: (What, When it started, How long, Solution Taken) ____________________________________________________________________________________________ ____________________________________________________________________________________________ MEDICAL HISTORY: (What Illness, When, Who/Where Treated, Treatment Done) ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ FAMILY HISTORY: (Relationship, Cause of Death/What Illness, When) ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ HISTORY OF ALLERGY: (What, When, Who/Where Treated, Treatment Done) ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ PSYCHOSOCIAL & DIETARY HISTORY: Religion: _____________________________________ Occupation: __________________________ Smokes? _____ What: ____________________ How many: __________ Drinks Milk? _____ What: ____________________ How many times: __________ Exercises? _____ What: ______________________________________ How long: ___________ What food are you fond of eating? _________________________________________________________ Sleep Patterns: ________________________________________________________________________ Are you on any other health therapy now? _____ What: ______________________________________ Describe: _____________________________________________________________________________ Home Situation & Daily Life: (Who lives with you? Who helps you when you’re sick or need assistance? Describe them and also your friends. What is your daily routine like from time of arising to bedtime?) ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ =========================================================================== I certify that I have read and understand all the questions set forth and the information provided are true and correct to the best of my knowledge. After knowing & understanding the treatment approach use in this system of medical management, I also on my own volition subject myself for treatment. _____________________________________ Patient’s Signature PERTINENT PHYSICAL FINDINGS: General Survey: Height: _____ Weight: _____ Sensorium: (Alert, Drowsy, Lethargic/Stuporous, Semicoma or Coma/Comatose) Attention Span: (Confused, Grossly disoriented, Demented) Orientation: to Time? _______________ Place? _______________ Person? _______________ Communication Ability: Can express or communicate thoughts or needs? ___ (Verbally, in Writing or by Gestures). If able to communicate verbally, is it (Clear or Dysarthria, Coherent or Incoherent), Can understand and respond appropriately to question or task? _________ What form of communication is he responsive to? (verbal, gestural or written). If able to comprehend, can follow instructions? ____________ Physique or built of patient: (Endomorphic, Ectomorphic, Mesomorphic, Sthenic, Hypersthenic, Hyposthenic or Asthenic). Nutritional Status: (Well-nourished, Overnourished/Obese, Undernouriished) If undernourished, what degree? ________ Development: (Well-developed, Fairly developed, Underdeveloped) Ambulation Status: (Bedridden, Wheelchair-borne, ambulant with or without assistance) Severity of Illness: (Presence or absence of an apparent distress and its relative intensity) If having difficulty in breathing, is respiratory distress (mild, moderate or severe). In pain? ___ intensity? Depressed? _____ intensity? _____ Vital Signs: Usual BP: _______ BP: _______ HR: ______ PR: ___ Rhythm: ________ RR: __ Skin: (Rashes, lumps, sores, itching, dryness, color change, changes in hair & nails) _______________________________ Head: (Headache, head injury) __________________________________________________________________________ Eyes: (Vision, glasses or contact lenses, pain, redness, tearing, blurring, double vision, spots or specks, glaucoma, cataracts, last eye examination) _____________________________________________________________________________ Ears: (Decreased hearing, tinnitus, vertigo, earaches, infection, discharges, hearing aids) ____________________________ Nose & Sinuses: (Frequent colds, nasal stuffiness, discharge, itching, hay fever, nosebleeds, sinus trouble) ______________ _______________________________________________________________________________________________ Mouth & Throat: (Dry mouth, sore tongue, frequent sore throats, hoarseness, condition of teeth & gums, bleeding gums, dentures?, if any, how they fit & last dental examination) ________________________________________________ Neck: (Lumps, “swollen glands”, goiter, pain or stiffness) ____________________________________________________ Breast: (Lumps, pain or discomfort, nipple discharge, self-examination?) ________________________________________ Respiratory: (Cough, sputum (color & quantity), hemoptysis, wheezing asthma, bronchitis, emphysema, pneumonia, tuberculosis, pleurisy; last x-ray film) ________________________________________________________________ Cardiac: (Heart trouble, high blood pressure, rheumatic fever, heart murmur, chest pain or discomfort, palpitations, dyspnea, orthopnea, paroxysmal nocturnal dyspnea, edema, past ECG or other heart test) _______________________ _______________________________________________________________________________________________ Gastrointestinal: (Trouble swallowing, heartburn, appetite, nausea, vomiting, regurgitation, vomiting blood, indigestion; Frequency of vowel movements, color & size of stools, change in bowel habits, rectal bleeding or black tarry stools, hemorrhoids, constipation, diarrhea; Abdominal pain, food intolerance, excessive belching or passing of gas, jaundice, liver or gallbladder trouble, hepatitis) ________________________________________________________________ Urinary: (frequency of urination, polyuria, nocturia, burning or pain on urination, hematuria, urgency, reduced caliber or force of urinary stream, hesitancy, dribbling, incontinence, urinary infections, stones) _________________________ _______________________________________________________________________________________________ Genitals: (Discharge, itching, sores, lumps, STD and treatments done, Sexual preference, interest, function, satisfaction and problems; MALE: Hernia? FEMALE: Age at menarche, regularity, frequency, and duration of periods, amount of bleeding, bleeding between periods or after intercourse, last menstrual period; age at menopause, menopausal symptoms, postmenopausal bleeding) ________________________________________________________________ _______________________________________________________________________________________________ Peripheral Vascular: (Intermittent claudication, leg cramps, varicose veins, past clots in the veins) ____________________ _______________________________________________________________________________________________ Musculoskeletal: (Muscle or joint pains, stiffness, arthritis, gout, backache. If present describe location & symptoms, i.e.; swelling, redness, pain, tenderness, stiffness, weakness, limitation of motion or activity) ________________________ _______________________________________________________________________________________________ Neurologic: (Fainting, blackouts, seizures, weakness, paralysis, numbness, tingling or “pins & needles”, tremors, other involuntary movements)___________________________________________________________________________ Hematologic: (Anemia, easy bruising or bleeding, past transfusions and any reactions)______________________________ _______________________________________________________________________________________________ Endocrine: (Thyroid trouble, heat or cold intolerance, excessive sweating, diabetes, excessive thirst or hunger, polyuria) _______________________________________________________________________________________________ Psychiatric: (Nervousness, tension, mood including depression, memory) _______________________________________________________________________________________________ =========================================================================================== DIAGNOSIS: ________________________________________________________________________________ INITIAL TREATMENT: _____________________________________________________________________ ____________________________________________________________________________________________ WELLNESS & REJUVENATION CENTER FOLLOW-UP RECORD NAME: ______________________________________________________ Page: ______________ =========================================================================================== PATIENT FEEDBACK/COMPLAINT: Date: __________ BP: ________ Weight: ________ Height: ________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ASSESSMENT/FOLLOW-UP TREATMENT: ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ PATIENT FEEDBACK/COMPLAINT: Date: __________ BP: ________ Weight: ________ Height: ________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ASSESSMENT/FOLLOW-UP TREATMENT: ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ PATIENT FEEDBACK/COMPLAINT: Date: __________ BP: ________ Weight: ________ Height: ________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ASSESSMENT/FOLLOW-UP TREATMENT: ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ PATIENT FEEDBACK/COMPLAINT: Date: __________ BP: ________ Weight: ________ Height: ________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ASSESSMENT/FOLLOW-UP TREATMENT: ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ PATIENT FEEDBACK/COMPLAINT: Date: __________ BP: ________ Weight: ________ Height: ________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ASSESSMENT/FOLLOW-UP TREATMENT: ____________________________________________________________________________________________ ____________________________________________________________________________________________ ____________________________________________________________________________________________ PATIENT FEEDBACK/COMPLAINT: Date: __________ BP: ________ Weight: ________ Height: ________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ASSESSMENT/FOLLOW-UP TREATMENT: ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________