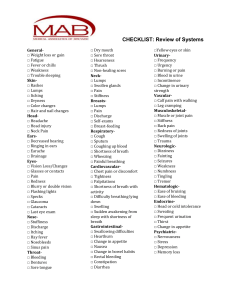
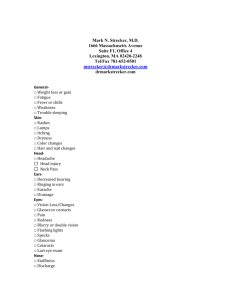
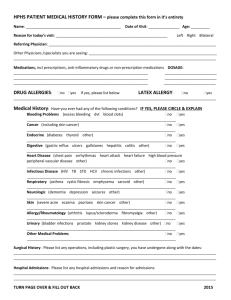
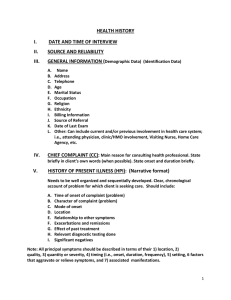
Source: Reliability: Time of Evaluation: GENERAL DATA Patient initials/ full name: Age: Gender: Nationality: Religion: Occupation: Marital Status: Current Residence: Place of birth: Date of birth: Number of admissions: (Date & time) Institution: CHIEF COMPLAINT One or more symptoms or concerns cause the patient to seek care. HISTORY OF PRESENT ILLNESS Amplify the chief complaint while describing how each symptom developed in a chronological fashion (OLD CARTS) Onset, Location, Duration, Character, Aggravating/ Alleviating Factors, Radiation, and Timing, Location Quality Quantity or severity (Pain score) Timing, onset, duration, frequency Setting in which symptom occurs Aggravating/relieving factors Pertinent positives/pertinent negatives medication use, name (generic and brand, dose, route, frequency of use, total # of tablets/capsules taken) Any other signs/symptoms. Skin lesions: PAST MEDICAL HISTORY Childhood illness Immunizations (BCG, DPT, POLIO, MMR)- COVID vaccine. Known childhood illnesses, year diagnosed, maintenance medications, compliance to meds, any known complications (MMR, whopping cough, chickenpox, rheumatic fever, scarlet fever, polio) History of admissions Adult illness Medical Known medical illnesses, year diagnosed, maintenance medications, compliance to meds, any known complications: ( DM, ASTHMA, HTN, RENAL PROBLEMSPROBLEMA SA BATO, CANCER) Screening tests/Annual medical exam findings (CBC, U/A, X-RAY, LIPID PROFILE) Admission History of Blood transfusion/donation (Blood type) Surgical: Accidents, injuries. Obstetric/Gynecologic: Age at menarche. regularity, frequency duration of periods amount of bleeding; bleeding between periods or after intercourse last menstrual period dysmenorrhea premenstrual tension Vaginal discharge, itching, sores, lumps, sexually transmitted infections and treatments. Number of pregnancies, number and type of deliveries, number of abortions (spontaneous and induced), complications of pregnancy, (GTPAL) No. of children birth-control methods/ FAMILY PLANNING Sexual preference, interest, function, satisfaction, any problems, including dyspareunia. Concerns about HIV infection. Psychiatric illnesses PERSONAL AND SOCIAL HISTORY Smoking history Alcohol use Illicit drug use Educational level Occupation Personal interests Lifestyle Travel Exercise habits Dietary practices Personal Hygiene Sleeping Habits Sexual orientation and practices Current household members and health status Marital relationship status if any Home safety, garbage and waste disposal Food and water supply Electrical supply FAMILY HISTORY Heredo-familial diseases in the maternal and paternal side Age, health, cause of death, comorbidities, medications of parents, siblings and grandparents. Presence of hypertension, diabetes, asthma, cancer, early cardiovascular deaths- cardiac arrest, psychiatric illnesses in the family REVIEW OF SYSTEMS System General: State of consciousness (conscious, lethargic, stuporous, comatose), coherent or incoherent, cooperative, ambulatory, nutritional status, severity of illness (Stable, toxic, moribound), febrile, emotional (in respiratory distress Skin: Rashes, lumps, sores, itching, dryness, color change, changes in hair or nails Head: Headache, head injury, dizziness, lightheadedness Eyes: Vision, glasses or contact lenses, last examination, pain, redness, excessive tearing, double vision, blurred vision, spots, specks, flashing lights, glaucoma, cataracts Ears: Hearing, tinnitus, vertigo, earaches, infection discharge. If hearing is decreased, use or non-use of hearing aids Throat (or mouth and pharynx): Condition of teeth, gums, bleeding gums, dentures if any and how they fit, last dental examination, sore tongue, dry mouth, frequent sore throats, hoarseness. Neck: Lumps, "swollen glands", goiter, pain, or stiffness in the neck. Breasts: Lumps, pain or discomfort, nipple discharge, self-examination practices. Respiratory: Cough, sputum (color, quantity), hemoptysis, dyspnea, wheezing, pleurisy, last chest x-ray, asthma, bronchitis, emphysema, pneumonia, and tuberculosis. Cardiovascular: Heart trouble, high blood pressure, rheumatic fever, heart murmurs, chest pain or discomfort, palpitations, dyspnea, orthopnea, paroxysmal nocturnal Comment dyspnea, edema, past electrocardiographic or other heart test results Gastrointestinal: Trouble swallowing, heartburn, appetite, vomiting, nausea, regular bowel movements, color and size of stools, change in bowel habits, rectal bleeding or black or tarry stools, hemorrhoids, constipation, diarrhea, abdominal pain food intolerance, excessive belching or passing of gas, jaundice, liver or gallbladder trouble, hepatitis. Urinary: Frequency of urination, polyuria, nocturia, urgency, burning or pain on urination, hematuria, urinary infections, kidney stones, incontinence Genital (Male): Hernias, discharge from or sores on the penis, testicular pain or masses, scrotal pain or swelling, history of sexually transmitted infections and their treatments. Sexual habits, interest, function, satisfaction, birth control methods, condom use, and problems. Concerns about HIV infection. Genital (Female): Age at menarche; regularity, frequency, and duration of periods; amount of bleeding, bleeding between periods or after intercourse, last menstrual period: dysmenorrhea, premenstrual tension; age at menopause, menopausal symptoms, postmenopausal bleeding. If the patient was born before 1971 exposure to diethylstilbestrol (DES) from maternal use during pregnancy, vaginal discharge, itching, sores, lumps, sexually transmitted diseases and treatments. Number of pregnancies, number and type of deliveries, number of abortions (spontaneous and induced); complications of pregnancy; birth control methods. Sexual preference, interest, function, satisfaction, any problems inducing dyspareunia, exposure to HIV infection Peripheral Vascular: Intermittent claudication, leg cramps, varicose veins, past clots in the veins Musculoskeletal: Muscle or joint pains, stiffness, arthritis, gout and backache. If present, describe location of affected joints or muscles, presence of any swelling redness, pain, tenderness, stiffness, weakness, or limitation of motion or activity; include timing of symptoms (for example, morning or evening), duration, and any history of trauma Hematologic: Anemia, easy bruising or bleeding, past transfusions and/or transfusion reactions. Endocrine: Thyroid trouble, heat or cold intolerance, excessive sweating, excessive thirst or hunger, polyuria, change in glove or shoe size. Psychiatric: Nervousness, tension, mood, including depression; memory change, suicide attempts, if relevant. Neurologic: Fainting, blackouts, seizures, weakness, paralysis, number or loss of sensation, tingling or pins and needles sensation, tremors or other involuntary movements PHYSICAL EXAMINATION General Survey 1. Observes for signs of distress; alters approach if patient is distressed. 2. Observes apparent age, gender, and race. 3. Notes facial characteristics, symmetry of features, expression, and condition and color of skin. 4. Notes body type and posture. 5. Greets patient with handshake to assess muscle strength (if culturally appropriate). 6. Observes gait and any abnormal movements (or ability to move about in bed). 7. Listens to speech pattern, pace, quality, tone, vocabulary, and sentence structure. 8. Obtains interpreter if there is a language barrier. 9. Assesses general mental state and affect. 10. Observes dress, grooming, and hygiene. 11. Measures vital signs. 12. Measures height and weight. a. Adults: Calculates BMI from height and weight measurement. b. Infants and children < 2 years: Height— positions supine with knees extended; also measures head circumference. c. Infants: Weighs without clothing; d. Older children: Weighs in underwear. 13. For children, plots height and weight on growth chart and evaluates trends. Vital Signs Blood pressure (mmHg) Pulse rate (bpm) Respiratory rate (cpm) Temperature (ºC) O2 Saturation (%) Mental Status Examination