History Psych paper Final - St. Francis Xavier University
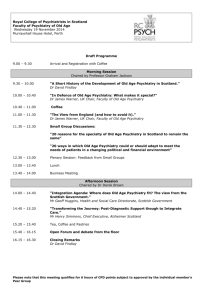
advertisement

Running head: ANTIPSYCHIATRY: EVOLUTION AND CONTEMPORARY INFLUENCE Antipsychiatry: Evolution and Contemporary Influence by Brianna E. Cheyne 201104592 Presented to Dr. J. Edwards in Psychology 300 History and Theory of Psychology Department of Psychology St. Francis Xavier University November 13, 2013 1 ANTIPSYCHIATRY Psychiatry, or the study of mental suffering, is centrally involved in the complex world of human reality (Bracken & Thomas, 2010). Its efforts lie at the interface of a number of discourses, such as genetics, neuroscience, psychology, sociology, philosophy, and anthropology. These areas of study provide society with lenses through which different conceptions of mental disorder could be understood. At various times in the history of psychiatry, particular manifestations of understanding have become dominant and worked to marginalize the contributions of others. The antipsychiatry movement thrived in the 1960s and 1970s by challenging the dominant view of mental disorder of its time. It served as the product of a growing counterculture movement that helped to question the scientific and ethical legitimacy of the psychiatric medical model. With the backing of intellectual psychiatrists like Thomas Szasz and R.D. Laing, this initial phase established antipsychiatry as a formal movement. Although the movement gained momentum during this time period, it has endured as an ex-patient consumerist coalition. It is evident that antipsychiatry is not simple a historical curiosity; rather it is a living tradition that continues to fight for justice in the mental health system. While the antipsychiatry movement is largely viewed as being a product of the 1960s and 1970s, its antecedents can be traced to the beginning of the twentieth-century when psychiatry experienced divisions from the field of medicine (Rissmiller & Rissmiller, 2006). During this time, psychiatry transformed from a relatively small, unified, institutionally based specialty to a large bifurcated field (Dain, 1989). This field consisted of its traditional element – the hospital practice that treated severe mental disorders, or psychoses, and the private practice that treated a new, less severe set of 2 ANTIPSYCHIATRY disorders called “neuroses.” New psychotherapeutic techniques were developed to treat neuroses, with the most popular being psychoanalysis. The grounds for accepting psychiatry as a medical specialty had always been that insanity was a natural disorder like any other (Dain, 1989). Disease was only said to be present when the physical soma became involved. At most, a patient’s outward expression of emotional disturbance was viewed as behavioural. The medical model of the early 1900s clearly distanced itself from a discussion of the mind, psyche, or soul in favour of observable, material causes. Psychoanalytic psychiatrists and neuropsychiatrists struggled to balance their support of this physical etiology with an absence of evidence for it in their practice (Dain, 1989). Although psychoanalytic psychiatry’s focus on psychogenesis (psychological causes) made the private practice fashionable, it also made it vulnerable to the challenges put forward by the biological bases of medicine. Rather than including biological intervention, it was centered on subjective non-somatic treatment that relied heavily on talk therapy. In hospital settings, biological successes in discovering the causes or cures of psychoses were often credited to medical science instead of psychiatry (Dain, 1989). As a result, hospital psychiatry lacked conclusive research or reliable treatments for many of the disorders that it dealt with. Patients were routinely admitted involuntarily to these institutions, where they were encouraged to take high does of antipsychotic drugs and underwent convulsive and psychosurgical procedures with limited value and negative side effects (Rissmiller & Rissmiller, 2006). Despite these discrepancies, psychiatry increased in status and prestige in the years after World War II. Wartime experiences were thought to have shown that 3 ANTIPSYCHIATRY community and outpatient treatment of persons with mental and psychological disorders was more effective than institutional care (Grob, 2010). Within the field of psychiatry itself, there was increasing receptivity to the psychoanalytic approach and its focus on the potential role of life experiences and socio-environmental conditions in the development of mental disorders. Psychiatrists and other mental health professionals began to believe that psychiatry could work in tandem with social and behavioural sciences to improve these conditions. In this way, psychiatry expanded its professional sphere beyond the traditional boundaries of diagnostic and therapeutic medicine and opened the field to greater sources of criticism (Grob, 2010). The late 1950s saw the emergence of a critical body of literature that analyzed the field of psychiatry in sociological and anthropological terms. This literature sparked a wide range of debate, including the questioning of traditional mental hospitals and the belief that psychiatry had gone beyond its medical boundaries by exploring socioenvironmental issues. While the context and specific subject matter of these works differed, they acted as a prelude to the formal antipsychiatry movement that appeared at the beginning of the 1960s. Antipsychiatry originated as a transnational movement consisting of individuals from within the profession as well as scholars from other fields. Most influential among the antipsychiatric views of mental disorder were those of Thomas Szasz and R.D. Laing. While the theories that they propounded were disparate, they each questioned the “medical model” of psychiatry and even the existence of mental illness itself. It was not a coincidence that a powerful critique of mainstream medicine flourished at this time. The middle to late 1960s were characterized by intense political and social activism, as 4 ANTIPSYCHIATRY previously accepted authorities and systems of belief were challenged (Rissmiller & Rissmiller, 2006). Antipsychiatry evolved alongside a predominantly Western counterculture that rebelled against several forms of political, sexual, and racial injustice and inequality. The civil rights movement of the United States brought attention to the seemingly arbitrary commitment of individuals with mental disorders to institutions and the dubious treatment that they received. This interest in civil rights was accompanied by a new claim that psychiatry served as an instrument of social control (Grob, 2010). Prominent voices of the antipsychiatry movement were influenced by and attempted to address these issues. Arguably the most instrumental internal critic of psychiatry was Thomas Szasz of the United States. Nineteenth-century liberalism and its assertion that individual liberty was the highest virtue formed the basis of many of Szasz’s intellectual convictions. Szasz was deeply critical of any actions of the government, noble or not, that served to limit individual liberty. He expressed the view that psychiatry was a specific tool implemented by the state to inhibit individuals’ liberty, stating that it rejected values such as “personal autonomy, liberty, and responsibility” (Grob, 2010). In other words, the state perceived psychiatry as a means for excluding nonconformists and dissidents from society. This provided sufficient reasoning for enforcing psychiatry’s use coercion. Citing the principle of “separation of church and state,” Szasz argued for a similarly clear division between psychiatry and state (Rissmiller & Rissmiller, 2006). In his pivotal paper and book by the same name, The Myth of Mental Illness, Szasz contended that mental disorder existed outside of the boundaries of what could be legitimately considered an illness. He described diseases as being pathological and 5 ANTIPSYCHIATRY maintained that difficulties with our thoughts, feelings, behaviour, and relationships were simply “problems of living.” In his view, medicine was only scientific if it dealt strictly with the workings of the body. The standard scientific measure that he supported, or his “gold standard” of disease was “bodily lesion identifiable by anatomical, physiological, or other physico-chemical observation or measure” (Bracken & Thomas, 2010). Throughout the 20th century, schizophrenia was the object of substantial research initiatives, enabling it to serve as a convenient reference point for criticism of the conventional view of mental illness. Szasz claimed that schizophrenia was incorrectly classified as a disease because it demonstrated no discernible brain lesion (Bracken & Thomas, 2010). Overall, Szasz believed that there was little reliability or validity to the classification of “problems of living” as mental illnesses and that subjective forms of human and social sciences were ineffective in the treatment of legitimate illnesses (Grob, 2010). To Szasz, the term mental illness amounted to a form of social labeling that only served to secure power for organized psychiatry and the state . He suggested that “autonomous psychotherapy” was the only sound response to states of distress and madness (Bracken & Thomas, 2010). This would involve individuals voluntarily seeking therapy from members of society that they saw adequate to help them. Szasz believed that psychotherapy was a non-medical process that could be performed by anyone and should never be provided by the state (Bracken & Thomas, 2010). R.D. Laing, a citizen of Great Britain, offered an additional critique of antipsychiatry. While Szasz’s main objective was to testify that, “mental illness” was a myth and that the medical model could not effectively alleviate so-called psychiatric problems, Laing challenged common ways of understanding psychotic experience. Laing 6 ANTIPSYCHIATRY joined the forces of many authors of the 1950s and 1960s that attempted to identify the social origins of behaviour. He held that mental illness had social causality, stating that insanity was a label that resulted from an individual’s refusal to adapt to social and cultural norms. Laing participated in existential philosophy in order to, “locate patients within their intersecting personal and social worlds” (Halliwell, 2013). In The Divided Self: An Existential Study in Sanity and Madness, Laing stated that it was misguided to view a patient with psychosis as showing signs of a disease; instead it was more accurate to view this behaviour as being expressive of the individual’s existence. Rather than being indicative of an illness, the paranoid delusions associated with schizophrenia were a justifiable response to an “inescapable and persecutory social order” (Rissmiller & Rissmiller, 2006). Laing articulated that the concept of insanity did not have biological roots; it was based on a statistical statement of normality (Grob, 2010). According to Laing, defining insanity in such terms originated from a failure to question or to criticize dominant societal and cultural values. Since insanity was not a disease, but an existential struggle for personal freedom, it could be treated through social remediation. Laing actively practiced such remediation by establishing over 20 therapeutic communities throughout England. Each community was intended to be an asylum in the original Greek sense of the word: a refuge from unwanted or unwarranted interference (Rissmiller & Rissmiller, 2006). Staff and patients were equal in status, medication used was voluntary, and it was accepted that people could come and go as they pleased. By the 1980s, organized psychiatry had addressed a number of the key grievances of the antipsychiatry movement. Consequently, antipsychiatry diminished in its sway as 7 ANTIPSYCHIATRY an organization (Rissmiller & Rissmiller, 2006). Involuntary commitment to state institutions decreased dramatically, high dosage and overreliance on antipsychotic drugs was reduced, and electroconvulsive therapy and psychosurgery became last resort treatments. Antipsychiatry’s criticisms and attacks on the specialty of psychiatry encouraged biological psychiatrists to strengthen their research in order to move in line with mainstream medical practice. Ironically the, the medical model that many critics of psychiatry disagreed with was what aided the reform that they had strived for; new pharmaceutical agents managed patients’ symptoms to the extent that they could be safely released into the community (Dain, 1989). The discovery of neurotransmitters and the study of twin registries demonstrated that biology played a role in the appearance schizophrenia (Grob, 2010). Overall, empirical research began to support a biopsychosocial model of psychiatry, changing psychiatry from a bifurcated field to a united front once more. Perhaps most damaging to the antipsychiatry movement was its loss of broadbased counterculture support. The political landscape of the Western world transformed from being radically leftist to representing a prevalence of conservative sentiments (Rissmiller & Rissmiller, 2006). Antipsychiatry could no longer retain the backing of other student, feminist, black, and gay coalitions. The utopian, antiestablishment ideal of many counterculture movements became increasingly irrelevant in the political arena. The rising mental health consumerist movement provided a new platform for the antipsychiatry coalition to be heard amongst changing social and political attitudes. The consumerist movement appealed to conservative politics because of its reliance on political alliances opposed to confrontation. The idea that patients might be able to help 8 ANTIPSYCHIATRY other patients posed the possibility of reducing costs of mental health treatment (Rissmiller & Rissmiller, 2006). The 1980s saw the antipsychiatry movement change hands from psychiatrists and scholars to those of prior patients. Ex-patients were viewed as most capable to carry the antipsychiatry message because they had actually experienced pharmacological treatment, coercive hospitalizations, and authoritarian psychiatric practices. These individuals believed that it was unnecessary to give leadership to intellectuals that had not reached out to them during the formal antipsychiatry movement. In this new era, the founders of antipsychiatry became “bystanders to the movement that they had begun” (Rissmiller & Rissmiller, 2006). Ex-patients began to create their own organizations in which they could express their feelings of pain and abuse, deny the appropriateness and effectiveness of the therapies offered to them, proclaim that they could pass judgment on their own treatment as well as establish their own alternative programs to hospitals and mental health facilities (Dain, 1989). These new organizations sought to foster a new generation of consumerism in which clients were inclined to be active, informed participants in the mental health system. While ex-patients and consumerists were of diverse backgrounds, they shared a common ideology that societal change was the only solution to the improving the circumstances of those deemed mentally ill (Dain, 1989). In particular, the consumerist movement regarded accountability of psychiatrists and other mental health providers as being central to this reform. The consumerist movement began as a series of small, disconnected entities like the Insane Liberation Front and the Network Against psychiatric Assault that came to fruition in the United States (Rissmiller & Rissmiller, 9 ANTIPSYCHIATRY 2006). These groups functioned fairly independently because they were only able to meet through annually held national conferences. The appearance of a growing Internet community in the 1990s saw antipsychiatry websites that linked antipsychiatry movements in over 30 countries. The consumerist movement in the past and present has shown concern for many issues undertaken by the antipsychiatry movement of the 1960s and 1970s. The medical model of mental health continues to fall under scrutiny, as the consumerist movement argues that it marginalizes and oppresses consumers that do not accept psychiatry’s diagnostic labels or do not respond in the desired way to an accepted medicalized treatment of their distress (Hopton, 2006). Consumerists encourage advocacy and selfdeterminism among patients in order to combat this issue. Biologically based treatments are still questioned on the basis of safety and effectiveness. Heavy reliance on chemicals and medical “experimentation” on mental patients is seriously opposed. The nature of modern research has been criticized for what consumerists view as an overemphasis on the value of randomized controlled trials as the most reliable form of evidence (Hopton, 2006). This stands in sharp contrast with the early antipsychiatry movement that provided very limited evidence to support its therapeutic interventions. The current consumerist movement argues that mental health professionals should consider a wider picture than that provided by random controlled trials. This issue may have existed in the evaluation of selective serotonin reuptake inhibitor antidepressant drugs. There is evidence that possible problems of dependence and withdrawal were overlooked due to the focus on specific clinical trials for the effectiveness of these drugs. As pharmaceutical research has grown, there have also been 10 ANTIPSYCHIATRY apprehensions about the role of manufacturers in the generation of the available information about psychiatric drugs (Hopton, 2006). The consumerist movement has been criticized for having internal conflicts of its own. One significant point of criticism has been that of voluntarism, which is at the heart of antipsychiatry and consumerist philosophy. Some activists condemn psychiatry under any conditions, voluntary or involuntary, while others believe that it is the right of the people to choose to undergo psychiatric treatment (Dain, 1989). A heavy concentration on alternative, voluntary, treatment centres is perceived by consumerists as a means to give patients the ability to control their lives. Critics have brought attention to the large masses of people like the criminally insane, terminally ill, and the elderly who may need assistance in finding psychiatric help. The consumerist movement has also been criticized for focusing too heavily on the wrongdoings of specific psychiatrists while downplaying the surge of mental health services like nursing homes and community mental health centres that are run by nonpsychiatric professionals. Critics contend that this new system has generated its own problems and abuses that should be taken into account. To many activists, the existence of psychiatry has legitimized the existence of mental illness. Many critics believe that even if this were true, it would not follow that if there were no psychiatrists that there would be no such disorder (Dain, 1989). Although psychiatrists of the past could be conveyed as authoritative, unapologetic, and obstinate, the profession always included a minority of members that did not display these tendencies and actively criticized their own field. Consumerists have been urged to increase their collaboration with such psychiatrists who can help to implement their reforms. 11 ANTIPSYCHIATRY Throughout history there have been dramatic changes to the mental health system, including changes to nomenclature, to those in charge of giving care, and to the body of available research. Still, people continue to suffer from behavioural, emotional, and cognitive disorders. The key issue has and always will be the perplexing phenomenon of mental disorder, as it remains imperfectly understood, interwoven throughout public policy and public opinions, and is inconsistently responsive to known therapies. This conclusion is evident in many years of progression and regression, optimism and pessimism, and reform and reaction throughout the world. Antipsychiatry, with its new embodiment in the consumerist movement, continues to have a role in stimulating debates and discussion about this phenomenon and how society approaches it. The existence of the consumer movement is vital to providing patients with an independent voice that shares their perspectives and plights. This voice needs to be accessible in professional and academic research and publications. As our understanding of mental disorder evolves alongside changing political, economic, and social forces, it is important that the consumer coalition poses similar questions to those of the original antipsychiatry movement in the 1960s and 1970s. Issues of the origins and management of mental distress, the validity of involuntary treatment, and other potential forms of oppression still hold relevancy today. The goal of an integrated forum of reform has become realizable through growing discussion of these issues between psychiatrists and consumerists. It is clear that the antipsychiatry movement is here to stay. 12 ANTIPSYCHIATRY 13 References Bracken, K. Thomas, P. (2010). From Szasz to Foucault: on the role of critical psychiatry. Philosophy, Psychiatry, & Psychology, 8(3), 219-228. Dain, N. (1989). Critics and dissenters: Reflections on 'anti-psychiatry' in the United States. Journal Of The History Of The Behavioral Sciences, 25, 3-25. doi:10.1002/1520-6696(198901)25:1<3::AID-JHBS2300250102>3.0.CO;2-G Grob, G.N. (2011). The attack of psychiatric legitimacy in the 1960s: rhetoric and reality. Journal of the History of Behavioural Sciences, 47, 398-416. doi:10.1002/jhbs.20518 Halliwell, M. (2013). Therapeutic revolutions: medicine, psychiatry, and american culture, 1945-1970. New Brunswick, NJ: Rutgers University Press. Hopton, J. (2006). The future of critical psychiatry. Critical Social Policy, 26, 57-73. doi:10.1177/0261018306059776 Rissmiller, D.J., Rissmiller, J.H. (2006). The evolution of the antipsychiatry movement into mental health consumerism. Psychiatric Services, 57(6), 863-866.