PATHOPHYSIOLOGY
advertisement

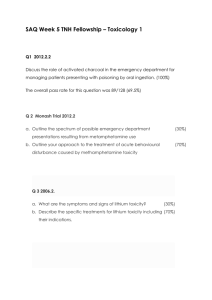
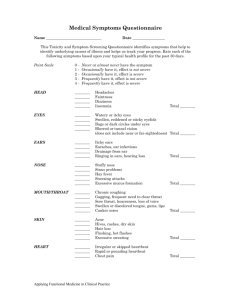
CNS stimulant PATHOPHYSIOLOGY Caffeine has many effects in the body. The three most commonly documented effects are (1) adenosine receptor antagonism, (2) phosphodiesterase inhibition, and (3) enhanced intracellular calcium levels.[13] Adenosine receptor antagonism leads to vasoconstriction, hypertension, tremor, and agitation. These effects are frequently seen in caffeine overdose.[72] These effects are the reverse of those seen with adenosine agonist activity, such as arterial vasodilation, inhibition of catecholamine release, and slowing of cardiac pacemaker cells.[13][50] Caffeine inhibits phosphodiesterases, causing increased levels of cyclic AMP, which results in increased levels of catecholamines. Muscle contractility is enhanced through increased intracellular calcium levels and increased permeability of the sarcoplasmic reticulum to calcium.[50][75] Stimulation of gastric acid and intestinal secretions and lowering of lower esophageal sphincter tone by caffeine commonly result in diarrhea and abdominal cramping.[50] Beneficial effects of caffeine include bronchodilation and vasodilation in the treatment of apnea in premature infants. Although caffeine-induced vasodilation may lower blood pressure, caffeine-induced medullary stimulation and increased catecholamine release offset this effect. Phenylpropanolamine and ephedrine act primarily via increased β1- and β2-adrenergic receptor agonist activity and enhanced release of catecholamines.[36] Phenylpropanolamine is as potent as ephedrine but causes less central nervous system (CNS) stimulation. Phenylephrine is a selective α1-adrenergic receptor agonist.[36] It is a derivative of epinephrine and produces similar therapeutic and adverse effects. Peripheral vasoconstriction and tachycardia are the most common adverse effects. Table 36–3 compares the α- and β-adrenergic receptor activity and CNS stimulation of caffeine and other nonprescription sympathomimetics. Chronic misuse of these agents may lead to cardiovascular abnormalities, such as vasculitis, stroke syndrome, cardiomyopathy, hypertension, and dysrhythmias. Table 36-3 -- Actions of Selected Sympathomimetic Agents at Peripheral Adrenergic Receptors in the Central Nervous System Alpha-Adrenergic Beta-Adrenergic CNS Substance Response Response Stimulation Amphetamine ++ ++ +++ Caffeine ++ + + Ephedrine ++ +++ ++ Phenylephrine ++++ 0 + Phenylpropanolamine +++ + +++ +, week activity. ++++, strongest activity. Oral preparations of these drugs are the most common forms available, but each of these agents may also be used intravenously. Phenylephrine is also available as a nonprescription inhaler. Phenylpropanolamine and caffeine may be sold on the street falsely as cocaine or amphetamines. In these cases, the agents may be snorted, ingested, or taken intravenously. CLINICAL PRESENTATION All the nonprescription sympathomimetics (i.e., caffeine, ephedrine, phenylpropanolamine, and phenylephrine) share some similar clinical features when taken in excessive amounts. Common symptoms include nausea, vomiting, diarrhea, abdominal pain, tremors, anxiety, agitation, and headaches.[1] Less common but more severe symptoms include delirium, seizures, hypertensive crisis, intracerebral hemorrhage, and myocardial infarction. Debate still exists as to whether or not a single dose of caffeine or phenylpropanolamine can result in clinically significant hypertension.[44][57][59] However, hypertensive crisis is documented in significant acute overdoses.[29] Phenylpropanolamine differs from caffeine in that phenylpropanolamine-induced hypertension is associated with a reflex bradycardia.[36] Caffeine overdose is most commonly associated with tachycardia. Although severe toxicity and death may be caused by any of these agents in an overdose situation, ephedrine, phenylpropanolamine, and phenylephrine appear to have more reported cardiovascular complications than caffeine.[10][25][50][51][58] Although hyperthermia is frequently seen with severe overdose of the psychostimulants (amphetamines, methamphetamines, and cocaine), it is rarely seen in caffeine overdoses. Sympathomimetic overdoses, however, can cause severe hyperthermia that may be lethal if untreated.[7][11] The hyperthermia is thought to be due to activation of specific dopamine receptors.[11] Increased motor activity and stimulant-induced seizures are also possible causes of hyperthermia after sympathomimetic overdose. Acute Toxicity In adults, ingestion of 500–1000 mg of caffeine may result in nausea, vomiting, diarrhea, tremors, and agitation.[1][50] Most patients have sinus tachycardia and a mild hypertension. Increases in cardiac output and glomerular filtration rate (GFR) can increase urine production. Dehydration and hypokalemia are common. Death due to caffeine overdose is rare but can result from the spontaneous vomiting that occurs with ingestion of large amounts. Caffeine-related deaths from dysrhythmias, seizures, and neurologic effects have been reported.[17][20][43] The estimated lethal dose of caffeine in an untreated adult is 5–10 g,[12][50] and in children 78 mg/kg has caused serious symptoms.[47][50][66] This may be due to the slower elimination of caffeine by children. Table 36–4 summarizes the clinical effects of over-the-counter sympathomimetics. Table 36-4 -- Clinical Effects of Caffeine Toxicity Mild and Common Sinus tachycardia Severe and Uncommon Seizure Reflex bradycardia with phenylpropanolamine Hypertensive crisis Hypertension Hyperthermia Nausea, vomiting, diarrhea, cramps Myocardial infarction/chest pain CNS agitation, anxiety Delirium Palpitations Intracerebral hemorrhage Chronic Toxicity Chronic excessive ingestions of over-the-counter sympathomimetic and caffeine frequently result in tachycardia, hypertension, and palpitations. Myocardial infarction, vasculitis, cardiomyopathy, and dysrhythmias (paroxysmal atrial tachycardia, premature ventricular contractions, bigeminy, ventricular tachycardia, and ventricular fibrillation) have been reported in large and chronic overdoses.[3][17][37][47][50][81] A cerebral vasculitis from chronic use and misuse of ephedrine may cause an acute intracerebral hemorrhage.[80] Chronic use and misuse may also lead to sustained hypertension and subsequent hemorrhage.[5] With chronic use, certain individuals may tolerate extremely large ingestions with minimal side effects, although others may experience severe symptoms at a fraction of the dose DIFFERENTIAL DIAGNOSIS Multiple medical and psychological conditions may mimic sympathomimetic toxicity ( Table 36–5 ). Serious medical conditions, including sepsis, intracranial hemorrhage, metabolic disorders, myocardial infarction, and primary dysrhythmias, must be excluded when patients present with signs of stimulant overdose. Psychiatric complications such as mania, anxiety, and panic attacks must also be considered in the differential diagnosis. Sympathomimetic abuse and overdoses may exacerbate preexisting psychiatric, neurologic, and cardiac conditions.[25][40][52] Table 36-5 -- Differential Diagnosis of Caffeine Toxicity Other drugs MAO inhibitors Cocaine Amphetamines Theophylline PCP LSD Anticholinergics Cardiac abnormalities Cardiomyopathy Hypertensive crisis Myocardial infarction Primary dysrhythmia Metabolic dysfunction Hyperthyroidism Pheochromocytoma Hypoxia Hypoglycemia Hyperthermia/sepsis Psychiatric disorders Anxiety Mania Panic disorder Sleep disorder CNS disturbances Intracranial hemorrhage Headache: migraine or tension TREATMENT ( Table36–6 ) Acute Overdose Treatment in all cases is supportive with attention to airway, breathing, and circulation. Oral activated charcoal, 1–2 g/kg of body weight is the primary mode of gastrointestinal decontamination. Gastric lavage may be considered if the patient presents to the emergency department within 1 hour after ingestion, has ingested a potentially life-threatening amount of drug, and does not have nausea and vomiting. Table 36-6 -- Treatment Essentials in Caffeine Toxicity Effect Therapy Dose (Adult) Decontamination Activated charcoal 50–100 g PO Dysrhythmia Diazepam: 5–10 mg IV q 5–10 min Benzodiazepines Lorazepam: 1–2 mg IV q 5 min Esmolol Esmolol: LD 500 μg/kg IV over 1 min; follow with 50 μg/kg/min IV infusion; titrate up q 5 min to a max of 200 μg/kg/min prn Effect Hypertension Therapy Dose (Adult) Lidocaine Lidocaine: 1–1.5 mg/kg IV bolus over 2– 3 min; may repeat dose of 0.5 mg/kg in 5–10 min up to a total of 3 mg/kg Procainamide Procainamide: LD 15–18 mg/kg given as slow infusion over 25–30 min; maintenance dose 1–6 mg/min by continuous IV infusion Benzodiazepines Diazepam: 5–10 mg IV q 5–10 min Lorazepam: 1–2 mg IV q 5 min Seizures Sodium nitroprusside Sodium nitroprusside: 0.5 μg/kg/min, increase by 0.5 μg q 5 min until desired effect; maximum dose of 10 μg/kg/min Benzodiazepines Diazepam: 5–10 mg IV q 5–10 min Lorazepam: 1–2 mg IV q 5 min Phenobarbital Nausea/vomiting Rehydration if necessary Potassium/electrolyte replacement Phenobarbital: 10–20 mg/kg IV given at a rate of 25–50 mg/min Titrate crystalloids to maintain urine output of 1–2 mL/kg/hr Replace electrolytes as needed. Antiemetics Metoclopromide Metoclopromide: Adult= 5–10 mg IV, PO, or IM up to a maximum dose of 1 mg/kg Pediatric: 0.1 mg/kg to maximum 10 mg dose Ondansetron Ondansetron Adult: 0.15 mg/kg IV (maximum 8 mg dose) Pediatric: ≤40 kg 0.15 mg/kg/IV >40 kg 4 mg IV Intravenous crystalloids are indicated for significant vomiting or diarrhea, and electrolyte losses should be replaced. Urine output should be maintained at 1–2 mL/kg/hour. Rhabdomyolysis may result in acute intrinsic renal failure, which may be avoided with intravenous (IV) crystalloids and IV mannitol, 0.5–1 g/kg over 5–10 minutes to maintain urine output of 1–2 mL/kg/hour. With significant aciduria the addition of sodium bicarbonate to maintain a urine pH value greater than 6.0 may protect the renal tubules and improve the prognosis of acute renal failure associated with rhabdomyolyisis.[34][65] If these treatments fail to produce diuresis or if electrolyte abnormalities persist, hemodialysis may be required. Caffeine may produce hypokalemia directly by activation of the Na+/K+-ATPase pump or secondarily by induction of emesis and diuresis.[61][67] Metabolic acidosis and catecholamine-induced intracellular shifts of potassium may also potentiate electrolyte abnormalities.[67] Potassium and other electrolytes should be monitored and replaced as needed. An antiemetic such as metoclopromide or ondansetron may be considered if protracted vomiting occurs. Temperature should be monitored closely. Stimulantinduced hyperthermia should be treated aggressively utilizing fans, ice water lavage, and ice water baths when necessary. Benzodiazepines such as diazepam and lorazepam should be given to patients who are agitated, hypertensive, or tachycardic. Benzodiazepines are frequently underutilized and often will decrease blood pressure and heart rate without further complications. Benzodiazepines may decrease or stop agitation, which can contribute to the development of rhabdomyolysis. The dose should be titrated intravenously to effect. The patient should be monitored for respiratory depression. The over-the-counter sympathomimetics may precipitate seizures in overdose.[43] Intravenous diazepam or lorazepam should be administered until seizures subside. If seizures persist, phenobarbital should be administered. With hypertensive crisis unresponsive to benzodiazepines, sodium nitroprusside is the drug of choice because of its short duration of action. The dose can be titrated to maintain a normal blood pressure. Phentolamine, an α-adrenergic receptor antagonist, has a longer duration of action and cannot be titrated as easily to effect. Nitroglycerine should be considered in cases with myocardial ischemia and infarction. Beta-adrenergic receptor antagonists should be avoided in a hypertensive crisis because unopposed α-adrenergic receptor agonist effects may result in further increases in blood pressure and adverse cardiac effects. Although labetolol blocks both α1- and β2-adrenergic receptors, its α1-adrenergic antagonist effect is one-fifth to one-tenth that of its β-adrenergic receptor antagonism. Use of labetolol may still result in unopposed α-adrenergic receptor agonism and further increases in blood pressure, and is not recommended. Reflex bradycardia should resolve with treatment of hypertension. Chronic Toxicity Treatment of chronic stimulant overdoses is more complicated because of the lack of well-controlled, long-term studies on chronic abuse of stimulants other than caffeine. Most data is extrapolated from acute toxicity or individual case reports. Chronic ingestion of caffeine is usually benign, but a withdrawal syndrome may be encountered if caffeine is stopped abruptly.[26][73] Headaches, lethargy, and agitation are the most commonly encountered effects. Reintroduction of caffeine followed by a gradual taper should relieve symptoms and prevent any further withdrawal symptoms. Diet aids containing phenylpropanolamine are frequently abused by women.[10][14][17][46] Increasing doses over months to years may be used to maintain diet and weight. Tolerance to these products develops readily, and large amounts may be ingested daily.[64] Prolonged and excessive misuse or abuse of these products has led to cardiomyopathy.[10] Hemorrhagic stroke and intracerebral hemorrhage may be encountered with both acute or chronic misuse or abuse of phenylpropanolamine and ephedrine.[15][25][35][42][51][77] Phenylpropanolamine-induced psychosis or relapsing of underlying psychiatric conditions has been documented.[52][68] Standard medical therapies are recommended for these complications. Antiarrhythmic KARL A. SPORER The action potential of a ventricular or Purkinje fiber ( Fig. 41–1 ) is generated by the flux of ions through specific channels in the cell membrane. Membrane depolarization results from the net influx of positive charges (sodium [Na+] and calcium [Ca2+]), and repolarization occurs secondary to the net efflux of positive charges (potassium [K+]) ( Table 41–1 ). Figure 41-1 EKG recording of ventricular muscle cell action potential. (Redrawn from Tan HL, Hou JY, et al: Electrophysiologic mechanisms of the long QT interval syndromes and torsade de pointes. Ann Intern Med 1995; 122:701–714.) Table 41-1 -- Major Ion Currents Underlying the Cardiac Action Potential * Effect of Current on Action Action Potential Phase Current Direction Potential Phase 0 (upstroke; inward > outward currents) Phase 1 (initial repolarization; outward > inward currents) Phase 2 (plateau; inward ∼ outward currents) INa Inward ITO Outward ICa Inward Slow inactivation maintains early plateau phase INaCa Inward May assist in maintenance of plateau phase ITO Rapid upstroke or action potential in atrial, ventricular, and Purkinje fibers Rapid early repolarization after overshoot of action potential Residual slowly inactivating Outward outward current during plateau phase Action Potential Phase Phase 3 (rapid repolarization; outward > inward currents) Current Direction IK Effect of Current on Action Potential Delayed rectifier repolarizes Outward membrane to near resting potential Phase 4 (Diastole; Inward ∼ Maintains high negative resting IK1 Outward or > outward currents) potential near -90 mV From Tan AHL, Hou CJY, Lauer MR, Sung RJ: Electrophysiologic mechanisms of the long QT interval syndromes and torsades de pointes. Ann Intern Med 1995; 122:701– 714. * INa, Fast inward sodium current; ITO, transient outward potassium current; Ica, slow inward L type calcium channel; INaCA, electrogenic sodium-calcium exchange current; IK, outward delayed rectifier potassium; IK1, outward potassium current that exhibits anomalous (inward-going) rectification. Phase 0 depolarization is mainly caused by the opening of the fast Na+ channels, allowing the influx of Na+ from a high concentration gradient toward a low concentration gradient. Phase 1 is a small depolarization mediated by the transient outward current of K+. The plateau phase, or phase 2, is maintained by the relatively slow influx of Ca2+through the L-type Ca2+channel. The rapid repolarization of phase 3 is generated by the efflux of K+ through the delayed rectifier K+ channel. The Na+/K+ adenosine triphosphatase (ATP) pump and the Na+ concentration–dependent electrogenic Na+/Ca2+exchange pump function between action potentials to maintain electrolyte balance. Na+ channel blockers will slow the phase 0 rapid upstroke and prolong the length of the entire action potential. For a given resting membrane potential, depolarization is associated with a reduced rate of voltage change and reduced maximum voltage. In addition, the higher threshold requires a greater stimulus to initiate the action potential. Clinically, this is manifested as Q-Tc prolongation in therapeutic concentrations and QRS widening in toxic concentrations. In higher doses, the Na+ channel blockade diminishes cardiac output; and in even higher concentrations it will also slow the heart rate. Ca2+ channel blockers in toxic doses will develop bradycardia from the slowing of atrial and ventricular action potentials. In addition, the slow and diminished action potential along with the low intracellular Ca2+ concentration will manifest as a diminished cardiac output, relative bradycardia, and peripheral vasodilation. K+ channel blockers prolong the action potential by slowing the efflux of K+. In addition to prolonging the action potential, this will also increase the resting membrane potential. There are currently no pure K+ channel blockers, and thus their clinical effects in isolation have not been determined. The treatment of toxicity due to Ca2+ channel blockers and β-adrenergic receptor antagonists is covered in Chapters 43 and 42 , respectively. CLASS IA: QUINIDINE, PROCAINAMIDE, DISOPYRAMIDE Essentials • Lethargy, confusion, coma • Widened QRS and Q-Tc intervals • Hypotension without tachycardia • Anticholinergic symptoms (primarily from disopyramide) The action potential of a ventricular or Purkinje fiber results from the rapid flux of Na+, Ca2+, and K+ through various transmembrane channels (see Fig. 41–1 and Table 41–1 ).[63] Antidysrhythmics work by partially blocking the function of specific ion channels and thus slowing various phases of the action potential. In the exaggerated response of toxicity, the surface electrocardiographic (EKG) abnormalities can be predicted. Quinidine, procainamide, and disopyramide are antidysrhythmic drugs in the class IA category and function as antidysrhythmics by blocking both the Na+ and K+ cardiac channels. Pharmacology/Pathophysiology Pharmacology See Tables 41–2 and 41–3 . Table 41-2 -- Modified Vaughan-Williams Classification of Antidysrhythmic Drugs Class Pharmacologic Effect Antidysrhythmic Drug IA Depresses rapid action potential upstroke and decreases conduction velocity (Na+ channel Quinidine, procainamide, blockade) and significantly prolongs disopyramide + repolarization (K channel blockade) IB Depresses rapid action potential upstroke in Mexiletine, lidocaine, tocainide, abnormal tissue (little effect in normal tissue) moricizine * and enhances repolarization IC Markedly depresses rapid action potential upstroke and decreases conduction velocity Propafenone, encainide, † (Na+ channel blockade) but exerts little effect flecainide, moricizine * on repolarization (little or no K+ channel blockade) II Blocks β-adrenergic receptors Propranolol, metoprolol, atenolol, esmolol, labetalol, Class Pharmacologic Effect Antidysrhythmic Drug nadolol, pindolol, sotalol, timolol and others III Primarily blocks K+ channels and slows repolarization (little or no Na+ channel blockade) Sotalol, amiodarone, bretylium Verapamil, diltiazem, nifedipine, and others From Tan AHL, Hou CJY, Lauer MR, Sung RJ: Electrophysiologic mechanisms of the long QT interval syndromes and torsades de pointes. Ann Intern Med 1995; 122:701– 714. IV Blocks L-type Ca2+ channels * Moricizine has been variously classified as a class IB and class IC agent. † Encainide was removed from US market in 1991. Table 41-3 -- Antidysrhythmics: Therapeutic Levels and Elimination Characteristics Therapeutic HalfElimination Active Levels Life Pathway Metabolites Class IA Quinidine 2–7 μg/mL 6–8 hr Hepatic Yes Procainamide 4–10 μg/mL 3 hr Hepatic/renal Yes Disopyramide 2–5 μg/mL 4–10 hr Renal/some hepatic No Class IB Lidocaine 3–5 μg/mL 1.5–2 hr Hepatic Yes Tocainide 3–9 μg/mL 10 hr Hepatic/renal No Mexiletine 1–2 μg/mL 10 hr Hepatic No Encainide 15–100 ng/mL 1–3 hr Hepatic Yes Propafenone 0.2–0.4 μg/mL 6–7 hr Hepatic No Moricizine 0.25–3 μg/mL 2–4 hr Hepatic Unknown Amiodarone 1–2 μg/mL 20–30 d Hepatic No Bretylium Not available 5–10 hr Renal No Sotalol 1.4–1.7 mg/L 9–11 hr Renal No Class IC Class III Pathophysiology Type IA agents depress the rapid action potential upstroke (phase 0) and decrease conduction velocity by Na+ channel blockade. They also significantly prolong repolarization and depress the slope of phase 4 depolarization by K+ channel blockade.[38][63] At therapeutic doses, patients will commonly manifest a prolonged QTc interval and an increased risk of torsades de pointes (polymorphic ventricular dysrhythmia). At toxic doses, patients will demonstrate increased Q-Tc and QRS intervals. Hypotension in type IA intoxication is caused by depressed myocardial contractility from the Na+ channel blockade and peripheral vasodilation from the K+ channel blockade. Procainamide is hepatically metabolized to the pharmacologically active N-acetyl procainamide (NAPA), which is renally excreted. Toxicity of NAPA commonly occurs in patients on therapeutic doses of procainamide in the setting of decreasing renal function.[14] Hypotension occurs mainly with intravenous infusions that exceed 20 mg/min. The Na+ channel blockade of quinidine and probably the other type IA agents has been demonstrated to increase in acidotic environments and worsen its toxicity.[30] Clinical Presentation The most serious manifestations of a type IA intoxication are primarily cardiovascular ( Table 41–4 ).[38] Mild intoxications may only manifest sinus tachycardia with Q-Tc prolongation and a normal blood pressure. Almost any dysrhythmia can occur in more serious cases, but the most common ones are QRS and Q-Tc interval prolongation, bundle branch blocks, ventricular tachycardia (often polymorphic), and ventricular fibrillation.[3][4][9][16][17][31][35][37][48][50][54][55][56][57][59][60][66][68][70] Table 41-4 -- Clinical Presentation of Antidysrhythmic Intoxication Type IA Mild or early intoxication—tachycardia, normal blood pressure, and Q-Tc prolongation Moderate to severe intoxication—QRS widening, hypotension with relative bradycardia, lethargy, confusion, coma (anticholinergic symptoms, mostly disopyramide) Type IB Confusion, coma, seizures Hypotension, widened QRS, ventricular dysrhythmias, and asystole in massive intoxication Type IC Q-Tc prolongation Hypotension Bradycardia Coma, respiratory depression, seizures Type III Amiodarone—increased PR interval, rare sinus bradycardia Sotalol—rapid-onset hypotension, bradycardia, Q-Tc prolongation, ventricular dysrhythmias Bretylium—profound coma, occasional transient hypertension followed by hypotension Hypotension commonly develops in severe intoxications and may be accompanied by a relative bradycardia. Central nervous system (CNS) symptoms are also commonly noted in type IA intoxication and can range from lethargy, confusion, coma, and respiratory depression to seizures. Quinidine has been noted to cause cinchonism, a syndrome characterized by tinnitus, vertigo, blurred vision, headache, and confusion. Disopyramide can produce significant anticholinergic effects in overdose and rarely has produced hypoglycemia during therapeutic use.[16][45] The anticholinergic effects of disopyramide are mostly mediated through its main metabolite, mono-Ndealkyldisopyramide. Differential Diagnosis The differential diagnosis of patients who present with a prolonged QRS interval, hypotension, relative bradycardia, and CNS symptoms includes a consideration of other drugs that possess type IA toxicity, other cardiotoxic agents, as well as severe electrolyte abnormalities ( Table 41–5 ). Table 41-5 -- Differential Diagnosis of Antidysrhythmic Intoxication Types IA, IC Other Agents That Can Prolong Q-Tc and Cause Torsades Cyclic antidepressants Phenothiazines Chloroquine, quinine Cocaine Propoxyphene (norpropoxyphene) Amantadine Arsenic Choral hydrate Organophosphates Diphenhydramine Terfenadine Astemizole Other Agents with Cardiac Toxicity β-Blockers Calcium channel blockers Electrolyte Abnormality Hypokalemia Hypomagnesemia Hypocalcemia Type IB Other causes of seizures (see Chapter 18 ) Severe intoxications Type IA drugs Calcium channel blockers β-Blockers Type III Amiodarone, sotalol Other β-blockers Calcium channel blockers Flecainide, encainide Bretylium Any sedative/hypnotic Clonidine Tetrahydrozoline Laboratory Studies The EKG is critical in predicting and following toxicity. An increase in the QRS complex width of more than 25 per cent over baseline has been used as a reliable indication of quinidine toxicity and has been commonly seen in both disopyramide and procainamide toxicity.[11] Drug levels of quinidine, procainamide, and NAPA are available, but rarely on a timely basis. Serum K+, Ca2+, and magnesium (Mg2+) levels can help to rule out significant electrolyte abnormalities. Treatment Early cardiac monitoring with intravenous access is important in these patients with a potential for lethal dysrhythmias ( Table 41–6 ). Aggressive gastrointestinal decontamination will be most useful early after ingestions. Attention to airway management in patients with lethargy or coma is important because type IA toxicity can be worsened by acute respiratory acidosis. Table 41-6 -- Treatment of Antidysrhythmic Intoxication All Classes Airway management, supportive care Gastrointestinal decontamination—activated charcoal Electrocardiographic monitoring Type IA, IC[38][40] Cardiac Conduction Delays NaHCO3 1–2 mEq/kg IV boluses. Maintain arterial pH at 7.4 to 7.5. Hypotension 0.9% NaCl 200–500 mL bolus infusions to correct hypovolemia NaHCO3 1–2 mEq/kg IV boluses. If still hypotensive, consider a pressor agent. Dopamine, norepinephrine, or epinephrine. Central hemodynamic monitoring may be helpful in guiding this therapy. Consider the use of an intra-arterial balloon pump or temporary cardiopulmonary bypass for intractable hypotension. Dysrhythmias Bradydysrhythmias—isoproterenol or epinephrine infusion. Consider a pacemaker. Polymorphic ventricular tachycardia (torsades de pointes) Magnesium, 2 g IV bolus. May repeat in 5–15 minutes. Isoproterenol or overdrive cardiac pacing Other Consider hemodialysis or hemoperfusion in patients with procainamide intoxication and large ingestions, high plasma concentrations, presence of circulatory collapse, or renal insufficiency. Type IB Seizures Lorazepam IV Phenobarbital IV load for persistent seizures Hypotension 0.9% NaCl 200–500 mL bolus infusions to correct hypovolemia Dopamine, norepinephrine or epinephrine. Central hemodynamic monitoring may be helpful in guiding this therapy. Consider the use of an intra-arterial balloon pump or temporary cardiopulmonary bypass for intractable hypotension. Type III Treat as for types IA and IC. Amiodarone—cholestyramine may be useful for gastrointestinal decontamination. Sotalol—glucagon may reverse β-adrenergic receptor antagonist effects (see Chapter 42 ). Sodium bicarbonate (NaHCO3) has been shown to be an effective therapy in reversing the EKG and cardiac contractility changes caused by quinidine in both animal models and in case reports.[4][15][38] It has also been reported effective in procainamide toxicity and logically should be helpful in disopyramide toxicity.[23] Several mechanisms may account for the efficacy of NaHCO3 in quinidine toxicity. Increasing the extracellular Na+ concentration may overcome the inhibition of conductance through Na+ channels. Alkalinization has been demonstrated to diminish the relative potency of quinidine at the Na+ channel.[30] There may also be some beneficial effect of lowering the serum K+. It is generally recommended that the serum pH be kept between 7.45 and 7.5. Patients who develop torsades de pointes should be treated with the usual pharmacologic interventions. Magnesium sulfate, overdrive pacing, and isoproterenol infusions have been very effective in suppressing this dysrhythmia.[67] Logically, NaHCO3 should lessen the QTc prolongation and also be helpful in suppressing torsades de pointes, but this has not been demonstrated clinically. Ventricular ectopy and ventricular dysrhythmias related to class IA toxicity can be more difficult to treat. The use of either class IA or IC (flecainide, encainide or propafenone) antidysrhythmics would be expected to be ineffective or to worsen the dysrhythmia. There is modest evidence that bretylium may be helpful in this scenario. NaHCO3 and lidocaine would be logical therapies. Hypotension should initially be treated by fluid resuscitation and administration of NaHCO3. Hypotensive patients unresponsive to fluids have been treated successfully with norepinephrine, isoproterenol, and dopamine. The only animal studies evaluating this question concluded that isoproterenol was superior to dopamine and glucagon in providing cardiovascular support.[28][32] An intra-aortic balloon pump has been used successfully in one patient and should be considered along with cardiopulmonary bypass for those patients with refractory hypotension.[60] Extracorporeal drug removal is useful in procainamide and NAPA toxicity, of little benefit in quinidine toxicity, and of questionable usefulness in disopyramide toxicity. Numerous case reports of procainamide poisonings have demonstrated clinically significant clearance by both hemoperfusion and hemodialysis and should be considered early in any large procainamide intoxication with hemodynamic instability, especially in the setting of renal insufficiency or failure.[3][9][17][55][57] Case reports and studies of disopyramide intoxications demonstrated modest usefulness of hemodialysis and hemoperfusion.[27][33][35] The role for extracorporeal drug removal in disopyramide toxicity is not well defined. Disposition Because of the rapid absorption of all these drugs, symptoms of toxicity and EKG changes will be apparent in the first few hours after ingestion. Patients who develop QRS widening, mental status changes, hypotension, or dysrhythmias need hospital admission and telemetry monitoring. Patients who are observed for 4 to 6 hours and do not develop QRS widening or other symptoms can be safely discharged if they are not suicidal. Sequelae The QRS complex may take up to several days to return to baseline even though most of the significant symptoms occur in the first 12 hours after ingestion. Other longterm sequelae are related to the severity of hypotension and hypoperfusion. CLASS IB: LIDOCAINE, TOCAINIDE, MEXILETINE Essentials • Confusion, coma, seizures • Hypotension, widened QRS complex, ventricular dysrhythmias, and asystole in massive intoxication Class IB antidysrhythmics act primarily by inhibiting Na+ channels selectively at ischemic and rapidly depolarizing myocytes.[5] Pharmacology/Pathophysiology Pharmacology See Tables 41–2 and 41–3 . Pathophysiology These Na+ channel blocking agents have little electrophysiologic activity on normal cells at therapeutic or moderately toxic doses. Because of these properties, there are no common EKG changes noted in intoxications. Cardiac dysfunction is only noted in massive intoxications when high concentrations partially block all cardiac sodium channels similar to type 1A agents. CNS toxicity is more common and is manifested as confusion or seizures. Ion transport is disturbed in the brain, and inhibitory neurons are initially blocked, causing excitatory stimulation and seizures. Higher concentrations will inhibit both excitatory and inhibitory neurons and induce coma and respiratory depression. Lidocaine has been shown to develop toxicity when administered orally, mucosally, and parenterally.[1][26][34][61] Oral lidocaine is well absorbed but undergoes significant first-pass metabolism. Lidocaine is hepatically metabolized to two active metabolites, monoethylglycinexylidide (MEGX) and glycine xylidine (GX), that may contribute to toxicity. The oral bioavailability of tocainide and mexiletine approaches 100 per cent, and neither compound is metabolized to any active metabolites. Clinical Presentation The majority of these intoxications will present as confusion, agitation, or seizures (see Table 41–4 ). There will likely be no finding other than history to differentiate this from other causes of seizure activity. Most of these cases will have a normal EKG and relatively normal vital signs. Severe intoxications can inhibit the Na+ channel in even normal cardiac tissue and will be similar to quinidine toxicity with a widened QRS complex and a diminished cardiac output. Almost any dysrhythmia can be seen in this setting. Mexiletine and tocainide intoxications are similar in presentation.[13][46][62] Differential Diagnosis The differential diagnosis includes any cause of seizures (see Chapter 18 ). The differential diagnosis of a severe intoxication with hypotension and dysrhythmias includes other antidysrhythmics and Ca2+ channel blockers (see Table 41–5 ). Laboratory Studies Determination of serum electrolyte levels is done to rule out metabolic causes of seizures. The EKG is monitored for QRS complex widening in cases of severe intoxication. Lidocaine levels are not readily available, but therapeutic concentrations are 3 to 5 μg/mL. Treatment General supportive care and control of the seizures is done first. Repetitive seizures should be controlled with escalating intravenous doses of lorazepam. Patients whose seizures are not controlled with high-dose lorazepam should be given intravenous phenobarbital. At this point these patients will likely require intubation and ventilatory support. Phenytoin acts as a class IB antidysrhythmic and should not be used. After airway management and seizure control, appropriate gastric decontamination with activated charcoal can be accomplished if necessary. Bradydysrhythmias may require a temporary pacemaker. Hypotension should be treated first with a normal saline bolus, then with a vasopressor. A temporary pacemaker may be helpful in these patients. Theoretically, NaHCO3 should be efficacious, but it has not been used clinically or studied experimentally. Extracorporeal cardiac support to maintain blood pressure and improve hepatic metabolism has proven useful in one experiment and one case report.[21][22] The experience of treating tocainide and mexiletine intoxications is limited but should be similar to that of lidocaine. Disposition These three agents are quickly and reliably absorbed. All patients should develop signs of toxicity in the first 1 or 2 hours. Any patient with mental status changes, seizures, hypotension, or dysrhythmias should be admitted to a monitored bed. Patients who do not develop symptoms within 4 hours can be safely discharged if they are not suicidal. Sequelae There are no sequelae. Specific Situations Special concern should be emphasized about the potential for toxicity with the use of oral lidocaine. Even though there is extensive first-pass metabolism with oral ingestion, seizures have been noted to occur with the misuse of oral lidocaine preparations.[26][34][61] The maximal doses of subcutaneous lidocaine tolerated are 4.5 mg/kg for plain lidocaine and 7 mg/kg with lidocaine with epinephrine. CLASS IC: FLECAINIDE, ENCAINIDE, PROPAFENONE, AND MORICIZINE Essentials • Q-Tc prolongation • Hypotension • Bradycardia • Coma, respiratory depression, seizures Type IC antidysrhythmics markedly depress the phase 0 rapid action potential upstroke by blocking the Na+-fast channels. These drugs have little or no effect on the K+ channels and thus have no effect on repolarization. Moricizine has some features in common with type IB antidysrhythmics.[20] Propafenone also exhibits minor βblocking and Ca2+-channel blocking activities. Encainide is no longer available in the United States after being withdrawn because of a prodysrhythmic effect. Pharmacology/Pathophysiology Pharmacology See Tables 41–2 and 41–3 . Pathophysiology The agents in this class have much in common with the type IA antidysrhythmics. In toxicity, the Na+ channel blocking effect will manifest itself as widened QRS and QTc intervals, hypotension, and bradycardia.[2][10][12][29][36][40][42][44][51][52][69] In addition, PR interval widening has been noted in flecainide intoxications.[42][69] Clinical Presentation Flecainide and encainide are both quickly absorbed, very bioavailable, and rapidly toxic. Most severe cases have demonstrated signs of toxicity within 30 to 120 minutes of the ingestion.[40] The most prominent signs and symptoms include hypotension, bradycardia, QRS complex widening, coma, respiratory depression, and seizures (see Table 41–4 ). Differential Diagnosis The differential diagnosis of patients who present with a prolonged QRS interval, hypotension, relative bradycardia, and CNS symptoms includes other agents that possess type IA properties and other cardiotoxic agents such as Ca2+ channel blockers or β-adrenergic blockers (see Table 41–5 ). Laboratory Studies The EKG is useful in predicting and following toxicity. In case reports, QRS complex widening has been consistently useful in predicting the presence and severity of poisoning.[69] Treatment Cardiac monitoring, intravenous access, airway management, and early gastrointestinal decontamination are important in managing these potentially severe intoxications. NaHCO3 boluses have been reported useful in treating the cardiotoxic effects and preventing dysrhythmias and hypotension.[52][58] There is no clear choice of a vasopressor for those patients who do not respond to crystalloid infusion and NaHCO3. Rapidly escalating doses of dopamine or epinephrine should be titrated to a reasonable blood pressure. Pacing has been successful in improving the hemodynamics in some patients. Extracorporeal cardiac support, including balloon counterpulsation or cardiac bypass, should be considered in severe refractory cases. Efforts at resuscitation should be prolonged because several cases of flecainide and propafenone poisoning survived extended periods of cardiopulmonary resuscitation with asystole or pulseless electrical activity and were discharged with normal neurologic status.[10][36][42][51] Disposition Patients with significant ingestions will manifest symptoms in 30 to 60 minutes. All patients with QRS widening, mental status changes, hypotension, or bradycardia should be monitored closely in an intensive care unit. These patients should be monitored for 8 to 12 hours after their symptoms have resolved. There has been one reported case of late-appearing dysrhythmias in a patient with severe flecainide intoxication.[29] Patients who have not developed symptoms in 4 to 6 hours can be safely discharged if they are not suicidal. Sequelae There are few or no long-term sequelae. One patient with an acute intoxication of propafenone had persistent QRS complex widening and diminished cardiac function at 4 months after ingestion.[36] Most other patients demonstrated complete recovery, with QRS widening resolving over hours to days. CLASS III: AMIODARONE, SOTALOL, BRETYLIUM Essentials • Amiodarone—increased PR interval, rare sinus bradycardia • Sotalol—rapid onset hypotension, bradycardia, Q-Tc prolongation, confusion; severe cases— respiratory depression, ventricular dysrhythmias • Bretylium—profound coma, occasional transient hypertension followed by hypotension Amiodarone, sotalol, and bretylium are type III antidysrhythmics because they function by blocking K+ channels. This slows the action potential repolarization and produces Q-Tc prolongation. Despite this one similar function, all of these drugs act differently in overdose because of their other pharmacologic properties and their differing pharmacokinetics.[41] Pharmacology/Pathophysiology Pharmacology See Tables 41–2 and 41–3 . Pathophysiology The toxicities of this group of antidysrhythmics cannot be predicted or explained by K+ channel blockade alone. A pure K+ blocker would slow the action potential’s return to baseline and reset the myocardial cell at a higher level that would make it more prone to ventricular irritability. Amiodarone has well-documented chronic toxicities (pulmonary fibrosis, Q-Tc prolongation, and thyroid abnormalities) but little acute toxicity because of its poor absorption.[53] The prolonged period of absorption allows the logical use of late gastrointestinal decontamination and dictates a long observation period. Sotalol is rapidly and completely absorbed and demonstrates toxicity within an hour of ingestion. In addition to the K+ channel blockade, it also has a significant βadrenergic receptor antagonist effect that explains most of the hemodynamic changes in overdose. Bretylium is only available in intravenous form, and intoxication is usually iatrogenic. In addition to its type III antidysrhythmic properties, bretylium affects the autonomic nervous system. An initial release of norepinephrine from sympathetic ganglia results in a transient increase in blood pressure and heart rate. Later, the drug blocks the release of norepinephrine by depressing adrenergic nerve excitability, causing hypotension and bradycardia. The severe coma caused by bretylium remains unexplained. Clinical Presentation Most acute amiodarone intoxications are benign and manifest little or no EKG changes. Reported EKG abnormalities include prolongation of the PR and Q-Tc interval, mild bradycardia, and one case of self-limited ventricular tachycardia.[7][8][25] More severe toxicity can be predicted in the future with the availability of an intravenous form of amiodarone. Sotalol intoxications can be expected to develop Q-Tc prolongation, bradycardia, and hypotension soon after ingestion. More severe intoxications will manifest as coma, respiratory depression, seizures, and ventricular dysrhythmias.[18][19][43][47][65] There have only been three reported cases of bretylium overdose.[6][24][64] These patients developed profound coma lasting 1 to 3 days. One patient developed transient tachycardia and hypertension, followed by a reduced cardiac output and refractory hypotension. No specific EKG changes were noted in any of these patients (see Table 41–4 ). Differential Diagnosis (see Table 41–5 ) The differential diagnosis for the cardiovascular effects caused by amiodarone and sotalol include other β-adrenergic receptor antagonist drugs, Ca2+ channel blockers, type 1A and 1C antidysrhythmics, and the other drugs that can cause prolonged Q-Tc and torsades. Differential considerations for bretylium toxicity include toxicity of any sedative/hypnotic agent, clonidine, and tetrahydralazine. Laboratory Studies The EKG may reveal Q-Tc interval prolongation in significant amiodarone or sotalol intoxication. Serum K+, Ca2+, and Mg2+ levels will be helpful in gauging the extent of electrolyte replacement necessary. Serum levels of class III antidysrhythmic drugs are not readily available. Treatment The slow absorption of amiodarone allows for late gastrointestinal decontamination in cases of significant ingestion. Activated charcoal has been effective in binding amiodarone and is the therapy of choice.[39] Cholestyramine binds amiodarone in the gastrointestinal tract as well as reduces the elimination half-life of absorbed drug, but its role in this ingestion is currently unclear.[49] Intravenous potassium should be given slowly to increase the serum potassium to greater than 4.5 mmol/L. K+ repletion alone has been noted to have a protective effect from the dysrhythmias caused by amiodarone.[53] Occasionally, torsades de pointes occurs in amiodarone intoxication (usually in combination with a type IA agent). This should be treated with intravenous magnesium and an isoproterenol infusion or overdrive pacing to increase the heart rate.[67] Sotalol ingestions resemble β-blocker intoxications, with a greater propensity for ventricular dysrhythmias. The initial treatment includes appropriate gastrointestinal decontamination, cardiac monitoring, and K+ repletion. Hypotension has been successfully treated with isoproterenol (to increase myocardial rate), dopamine, and cardiac pacing. Glucagon, commonly employed in β-adrenergic receptor antagonist intoxication, is a logical choice in a patient refractory to other pressors. Patients with recurrent ventricular dysrhythmias have been successfully treated with defibrillation and lidocaine. The treatment of bretylium intoxication includes airway management and other supportive measures. Coma may be prolonged and can resemble brain death. In addition, hypotension may require vasopressors or extracorporeal cardiac support. Disposition Amiodarone’s prolonged absorption, up to 15 hours, dictates a long observation period and will require the admission of all but the most trivial of ingestions. Clinical endpoints for amiodarone ingestions are unclear, owing to limited clinical experience. Sotalol intoxications will demonstrate EKG and vital sign changes within the first few hours. A patient monitored for 4 to 6 hours without EKG changes, hypotension, bradycardia, or mental status changes can be safely discharged if the patient is not suicidal. The Q-Tc prolongation can persist for days and is not a useful endpoint of observation. Late-presenting torsades has not been reported in these cases. Patients should be observed for 6 to 8 hours after vital sign abnormalities and dysrhythmias have resolved. Bretylium intoxications are usually iatrogenic. These patients require admission and should be observed for 12 to 24 hours for mental status changes. Sequelae Q-Tc interval prolongation can persist for days. There are no other significant sequelae of these ingestions.