infection control procedures
advertisement
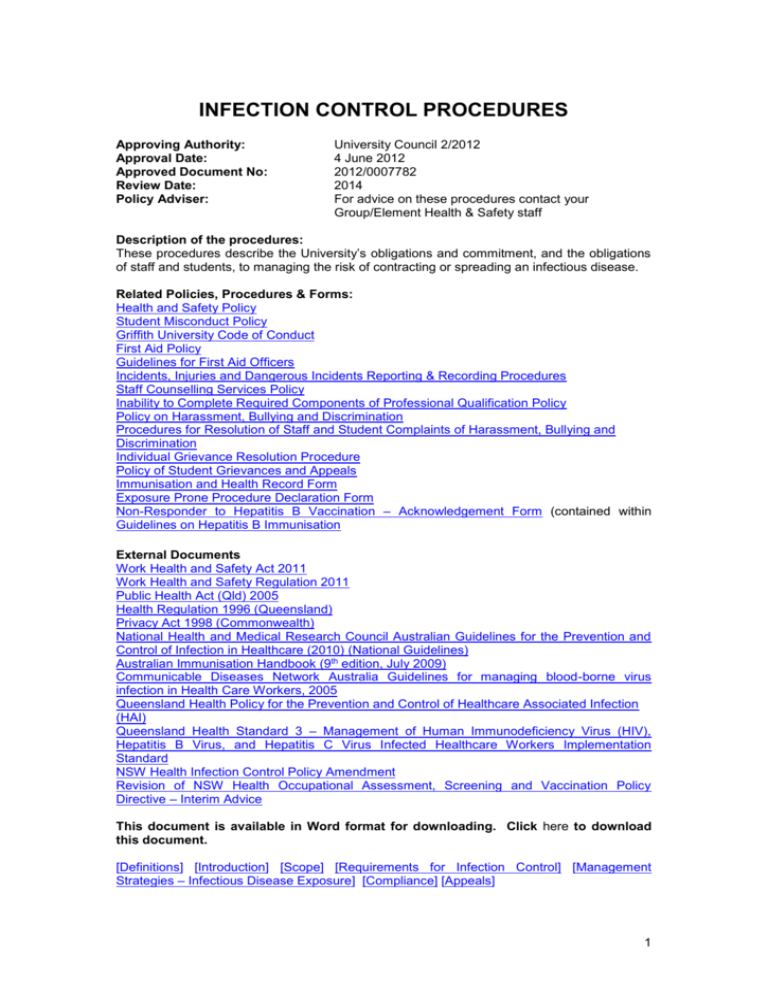
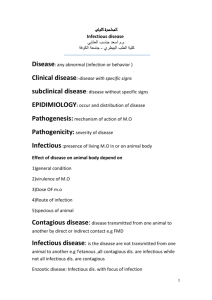
INFECTION CONTROL PROCEDURES Approving Authority: Approval Date: Approved Document No: Review Date: Policy Adviser: University Council 2/2012 4 June 2012 2012/0007782 2014 For advice on these procedures contact your Group/Element Health & Safety staff Description of the procedures: These procedures describe the University’s obligations and commitment, and the obligations of staff and students, to managing the risk of contracting or spreading an infectious disease. Related Policies, Procedures & Forms: Health and Safety Policy Student Misconduct Policy Griffith University Code of Conduct First Aid Policy Guidelines for First Aid Officers Incidents, Injuries and Dangerous Incidents Reporting & Recording Procedures Staff Counselling Services Policy Inability to Complete Required Components of Professional Qualification Policy Policy on Harassment, Bullying and Discrimination Procedures for Resolution of Staff and Student Complaints of Harassment, Bullying and Discrimination Individual Grievance Resolution Procedure Policy of Student Grievances and Appeals Immunisation and Health Record Form Exposure Prone Procedure Declaration Form Non-Responder to Hepatitis B Vaccination – Acknowledgement Form (contained within Guidelines on Hepatitis B Immunisation External Documents Work Health and Safety Act 2011 Work Health and Safety Regulation 2011 Public Health Act (Qld) 2005 Health Regulation 1996 (Queensland) Privacy Act 1998 (Commonwealth) National Health and Medical Research Council Australian Guidelines for the Prevention and Control of Infection in Healthcare (2010) (National Guidelines) Australian Immunisation Handbook (9th edition, July 2009) Communicable Diseases Network Australia Guidelines for managing blood-borne virus infection in Health Care Workers, 2005 Queensland Health Policy for the Prevention and Control of Healthcare Associated Infection (HAI) Queensland Health Standard 3 – Management of Human Immunodeficiency Virus (HIV), Hepatitis B Virus, and Hepatitis C Virus Infected Healthcare Workers Implementation Standard NSW Health Infection Control Policy Amendment Revision of NSW Health Occupational Assessment, Screening and Vaccination Policy Directive – Interim Advice This document is available in Word format for downloading. Click here to download this document. [Definitions] [Introduction] [Scope] [Requirements for Infection Control] [Management Strategies – Infectious Disease Exposure] [Compliance] [Appeals] 1 1.0 Definitions Exposure-prone procedures are a limited subset of invasive procedures characterised by the potential for contact between the skin (usually finger or thumb) of a person and sharp surgical instruments, needles or sharp tissues (splinters/pieces of bone/tooth) in body cavities or in poorly visualised or confined body sites including the mouth. Infectious Diseases are caused by pathogenic microorganisms, such as bacteria, viruses, parasites or fungi; the diseases can be spread, directly or indirectly, from one person to another. Invasive Procedure is any procedure that pierces the skin or mucous membrane or enters a body cavity or organ. This includes surgical entry into tissues, cavities or organs or repair of traumatic injuries. 2.0 Introduction Griffith University is committed to providing staff and students with a healthy and safe environment in which to work and study. The University acknowledges that some staff and students as a part of their work or study at the University may be at increased risk of exposure to infectious diseases as a result of involvement in areas including but not limited to: Work with infectious organisms; Work with human blood or body fluids; Clinical work with humans (including work undertaken by students on workintegrated placement in either University-run clinics or in facilities, including healthcare facilities, run by external organisations); Work with animals; First aid; Cleaning and maintenance; Overseas travel on University business. Griffith University staff and students have an obligation to care for the safety of others (including but not limited to fellow staff members and students of the University, patients/clients and members of the public with whom they are in contact through the course of their University activities) under both common law and the Workplace Health and Safety Act 1995. This duty of care includes a duty to minimise the risk of spreading or contracting infectious diseases. The University is required to comply with the Public Health Act (Qld) 2005, the Work Health and Safety Act 2011 and other legislation to ensure the health and safety of the University community and the wider community with respect to infectious diseases. The University must also comply with other State and Commonwealth legislation that enables it to provide an environment free from unlawful discrimination, harassment and vilification, which includes persons in the University community who have an infectious disease. The purpose of these procedures is to outline the precautions that should be taken with respect to infectious diseases to protect the health of staff, students and the community during the course of staff employment and students’ studies with the University (including during the course of any fieldwork, placements, practicum or the like that occurs at sites other than on University campuses). 3.0 Scope These procedures apply to all staff and students of the University who are or may be required to undertake activities as part of their work, research or study (eg. course / program / research project), which may cause them to come into contact, either on2 campus or on sites external to the University, with potentially infectious/hazardous (biological) material, or may potentially make them an agent of transmission of infection. These procedures also cover those staff members or students who are aware that they have a notifiable disease or acquire such a disease during their study or employment at the University. 4.0 Requirements for Infection Control Staff and students must understand their responsibilities to protect themselves and others from the hazards of blood-borne and other infectious diseases. Pregnant or immuno-compromised staff and students are encouraged to declare their status to their supervisor or course convenor in order that risks to their health and the health of others can be appropriately assessed and managed. 4.1 Risk Assessment Each Element (e.g., academic school or department, administrative department and / or research Element) is responsible for assessing the infection control risks related to the activities for which they are responsible. The University promotes ongoing risk assessment and management of exposure to infectious diseases according to the National Guidelines (www.nhmrc.gov.au/node/30290). The risk assessment by academic Elements must include courses and programs for which the Element is the host, student placements, and research projects or consultancy activities in which staff members and/or students are engaged. 4.2 Documentation of Procedures Where risk is identified, the Element is responsible for documenting infection control procedures and requirements applicable to the activities of the Element. Infection control procedures and requirements may include but are not limited to: 4.3 Cleaning, disinfection and sterilisation; Hand hygiene and hand washing protocols; Handling and disposal of potential infectious / hazardous material (biological); Handling and disposal of sharps; Provision and use of protective clothing and equipment; Requirements for immunisation of staff and students; Processes to be followed in the event of occupational exposures via percutaneous and non-percutaneous injury (e.g. needlestick injury or body fluid exposure), including follow-up procedures; Standard precautions and additional precautions. Communication, Education and Management Where risk is identified, the Element is responsible to ensure that the documented infection control requirements are supported by an appropriate education and management program. The education and management program shall include, but not be limited to: Provision of, or reference to, material, informed by the National Guidelines, covering topics including infection control requirements related to the work and study areas of staff and students, prior to them undertaking any activity that may expose them, or anyone they come into direct contact with, to an infectious disease. Where possible, the information should be located on the Griffith University website and be publicly accessible. Elements must also advise their staff and students of any subsequent changes to requirements throughout the duration of their employment or studies. Staff and students are required to read and comply with infection control guidelines provided to them, either by the University or, in the event that they are to undertake work or study (including work integrated placement) within external organisations, by the relevant external organisation; Provision of appropriate training in infection control requirements in which staff and students are required to participate; 3 4.4 Ensuring staff and students have access to appropriate protective clothing and equipment and that this is used appropriately; Ensuring all accidents / incidents which may place staff, students or others at risk of infection are recorded and actioned in accordance with the infection control requirements determined by the University or other relevant authority (e.g., Queensland Health Communicable Diseases Unit); In the case of exposure, provision of advice about appropriate counselling/support where required. Immuno-compromised persons and pregnant staff and students (where this is known) are provided with relevant information from the University Health Service and/or Queensland Health to assist them to avoid infectious circumstances; Steps are taken to ensure that the risk of possible transmission of infection among clients accessing University facilities and services is minimised, and that where appropriate clients are advised of risks of transmission of infection. Requirements for Immunisation and/or Health Certification Where, as a part of the Element’s infection control requirements, students undertaking a particular course or program are required to provide evidence of immunisation or to provide any other form of health certification, these specific requirements must be conveyed to students via the Program Catalogue. Requirements set down by Elements may include, but are not limited to: documentary evidence signed by a medical practitioner that staff/students have received required immunisations and/or achieved required levels of immunity against infectious diseases within the timelines specified on the Program Catalogue; requiring staff/students to take responsibility for maintaining ongoing awareness of their own infectious disease status and taking appropriate action to ensure their own safety and the safety of others in the event that they contract an infectious disease. The relevant Element in which staff or students are employed or enrolled is responsible for recording required evidence of immunisations and immunity against infectious diseases and for maintaining confidentially the records relating to each staff or student’s compliance with the requirements. The Element is responsible for ensuring that no information gathered through the operation of these procedures is disclosed to any person outside of the provision of these procedures without the express consent of the staff or student to whom the information relates. Where a staff member or student has failed to comply with an Element’s infection control (including immunization and/or health certification) requirements, the Element may prevent the staff member or student from undertaking certain activities. In the case of a student, the Element may progress the matter through the Inability to Complete Required Components of a Professional Program Policy through which the University may impose a range of measures including, but not limited to, preventing a student from enrolling in a course in which risk of them contracting or transmitting an infectious disease as a result of their failure to comply with the Element’s infection control requirements has been identified. Students are responsible for all costs associated with meeting the immunisation/vaccination requirements specified for their program. Where staff require screening or administration of vaccines, due to the nature of their work, the Element is responsible for the associated costs. 4.5 Practicum and Placements Staff and students who undertake practical educational experiences and/or workintegrated placements either on a University campus or at an organisation external to the University are required to comply with the relevant infection control and immunization requirements of the organization in which they are undertaking 4 the practicum or placement, (and where required provide evidence of subsequent levels of immunity achieved). Staff and students who undertake, or could reasonably be expected to undertake invasive or exposure-prone procedures as a part of their work or study with the University, including work or study undertaken on work-integrated placement must: undergo testing to determine their infectious disease status prior to commencing their studies and prior to their first clinical placement; undergo further testing to detect changes in their infective status at least every 12 months while enrolled in their program, or as recommended by current medical guidelines; in the event they have been at risk of acquiring a blood borne virus (e.g., through occupational exposure or through unprotected sexual activity or unsafe injecting practice with a partner whose infection status is not definitely known) arrange further blood borne virus testing at an appropriate interval after any exposure, and must refrain from participating in exposure prone procedures until they have been definitely determined not to be infected; complete documentation relevant to their work or studies. Students must complete all documentation specified on the Program Catalogue as required for their program including where required but not limited to the Exposure Prone Declaration Form relating to infectious disease management; and take all reasonable steps to protect other staff, students, patients/clients and members of the community with whom they interact from adverse outcomes including the acquisition of avoidable infectious diseases. Staff and students undertaking invasive or exposure-prone procedures should employ precautions against infectious diseases including adopting safe work practices to all persons with whom they are interacting in the work environment regardless of those persons’ known or presumed infectious status. Standard precautions constitute the frontline approach to infection control and include hand washing, use of appropriate personal protective equipment, management of sharps and immunization. A staff member or student who is aware that he or she is infected with a bloodborne virus must not undertake exposure-prone procedures and should seek urgent confidential advice from an appropriate staff member in their School, or from the Queensland Health Communicable Diseases Unit. If exposure-prone procedures are a required component of a student’s program, a student who is infected with an infectious disease may not be able to complete practical aspects of their program. In this instance the matter will be dealt with under the Inability to Complete Required Components of a Professional Qualification policy. 4.6 Notification of Communicable Disease There are certain infectious diseases that legislation such as the Public Health Act (Qld) 2005 (and other comparable laws that exist in all Australian states and territories and the Commonwealth) mandates as notifiable to State, Territory or Commonwealth health departments. Infectious diseases that are notifiable are generally highly communicable and/or are associated with a high severity of illness. They may be spread by contact, droplet or airborne transmission, and include (but are not limited to): Acquired Immune Deficiency Syndrome (AIDS)/Human Immunodeficiency Virus (HIV) infection, Hepatitis B virus (HBV) infection, Hepatitis C virus (HCV) infection, Neisseria Meningitis infection, Whooping Cough, Measles, Rubella, Legionellosis and Tuberculosis. In accordance with State legislation, staff and students of the University do not have to disclose notifiable diseases they may have to the University, however they are required to disclose to the appropriate State Health Department. 5 Disclosure to the University is encouraged so that the University can take steps to support infected staff and students and minimize the risk of harm to others. Staff and students who are involved in programs in which Hepatitis B immunization is mandatory are required to disclose to their School if they have a Hepatitis B infection. Disclosure is necessary as many clinical institutions in which students attend placements have a mandatory requirement for Hepatitis B immunity and confidential negotiation may be required between the School and placement provider for an appropriate placement to be arranged. This information will be held in the strictest confidence. 5.0 Management Strategies – Infectious Disease Exposure 5.1 Known use of biological infectious agents Where a known biological infectious agent is being used by staff or students (e.g., in research activities), there must be a standard protocol developed and located within the facility in which the agent is being used which can be referenced by all staff, students, cleaners and/or external clients or visitors for the management of that agent including: the procedural steps for containment (including where relevant PC2 or PC3 laboratory containment of infectious agents); management protocol for exposure; and procedures for reporting. 5.2 Incidence of infectious disease In the event of an occurrence of an infectious disease involving a University staff member or student, of which the University is made aware, the University (via the head of Element or nominee) will immediately contact the relevant state or territory health department within the jurisdiction in which the occurrence took place (or health department of the country in which the occurrence took place in the event of international incidents) and will comply with advice received from this organisation. In the event of an occurrence of an infectious disease involving a University staff member or student of which the University is not made aware, it is the responsibility of the infected person(s) to immediately contact the Queensland Health Communicable Diseases Unit or other relevant state, territory or international health department and comply with advice received from this organisation. 5.3 Incident involving occupational exposure Elements must have procedures in place for dealing with occupational exposures, which are relevant to their staff and students. Examples of exposure-prone activities include activities undertaken in: the clinical context (e.g. needlestick/sharps injury, body fluid exposure, splashes, aerosols, contact transmission); and the laboratory and practical class context (e.g. use of equipment, splashes, aerosols from body fluids, sharps injury). An exposed person should follow the required protocol and procedures and report the incident immediately to their supervisor, who is responsible for ensuring the safety of the area. The designated supervisor must follow the appropriate procedures as determined by the Element for such an injury or incident, and complete the appropriate documentation at the time. The exposed person should have a medical evaluation at an appropriate health care facility, e.g., the nearest Griffith University Health Service, Emergency Department at the nearest local hospital, or their own medical practitioner. 6 If an injury occurs outside of normal working hours, the staff member or student at risk should contact the Emergency Department at their nearest local hospital. An Incident / Injury Report Form must be completed detailing the incident and forwarded to the Office of Human Resource Management. 6.0 Compliance All staff and students are expected to follow instructions of safe practice in work/study activities and to act in a manner that does not place themselves or others at risk of contracting an infectious disease. It is the responsibility of staff and students to ensure that they comply with the instructions given for workplace health and safety in regard to infection control. Deliberate disregard for workplace health and safety instructions may be the subject of action under the University’s Student Misconduct Policy or Staff Misconduct Policy and may result in a report being made by the University to the relevant professional registration board. Failure by a staff member or student to comply with relevant infection control protocols and requirements, including conscientious objection to immunization, may lead to an increased risk of serious illness for that person or other persons with whom a staff member or student comes into contact in the course of their work or studies. Failure to comply may also mean that staff and students may be prevented from engaging in activities (e.g., work-integrated learning placements) that place themselves and those persons with whom they may come into contact with at risk of infection. 7.0 Appeals Where a member of staff or a student has a grievance concerning a decision made under these procedures, they are entitled to raise the grievance under the provisions of the Grievance Resolution Procedure (for staff) or the Policy on Student Grievances and Appeals (for students). 7