Summary of Zoonotic Diseases
advertisement

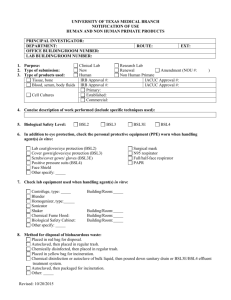
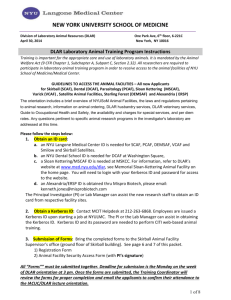
Occupational Medicine Program for Research Personnel Working With Animals – Non - DLAR Employees People who work with animals in a modern setting are at risk for occupational related disease and injury. The risks are variable depending upon the species one is using, the source of the animals, the amount and type of contact one has with the animals, etc. Potential problems include animal related allergies, injuries and infectious diseases. The quality of today’s research animals greatly limits the chance of acquiring an infectious disease from the animals at SUNY-Stony Brook (SUSB). This is particularly true for anyone using purpose-bred rodents or rabbits. The other animals used at SUSB pose slightly higher but still very small risks from infectious disease. A brief list of zoonotic diseases is attached. The DLAR maintains a library with more complete information. Anyone desiring further information can contact the DLAR Director. Allergies are common in people working with laboratory animals. These include both inhalant and contact allergies. Nearly every species housing in the DLAR has the potential to cause allergic reactions in susceptible individuals. In most cases the allergies develop after employment begins. Symptoms can vary but can include conjunctivitis, dermatitis, respiratory problems and anaphylaxis. Injuries are the most common occupational adverse health outcome for DLAR staff. These injuries are often related to the amount of lifting performed, use of heavy equipment, movement across wet floors, etc. The risk of these types of injuries for most non-DLAR staff is lower but still exists. Investigators and their staff should be watchful for wet floors and practice proper lifting techniques. In addition, both groups are at risk from animal scratches and bites. Proper animal handling greatly reduces the potential for a bite or scratch. An effective Occupational Medicine Program includes training, prevention and clinical care. A. Training 1) All research staff members will receive a handout entitled, “The Potential Risk of Disease from Animals”. 2) Staff intending to work with animals should contact the DLAR to attend the next Introduction to the DLAR training class. This class reviews animal handling and disease hazards and provides additional sources of information on these topics. These classes are available quarterly. 3) A web-based training program, providing information on working with laboratory animals, different species of animals and special technical procedures is available. Contact Dr. Jan Wyrick Gnadt for more information (444-2194). 4) DLAR provides hands-on training, upon request of individual research personnel or the IACUC, in humane methods of restraint and laboratory procedures with emphasis on injury prevention for both personnel and animals. 5) Training sessions in chemical, radiation and bio-hazardous material safety and ergonomics are provided by the Department of Environmental Health and Safety through the DLAR. Research staff members are strongly encouraged to attend these sessions. 6) The Center for Occupational and Environmental Medicine (COEM) provides training in proper wound management techniques, utilizing Bite and Scratch Kits provided by DLAR in non-human primate housing areas, for personnel working with macaques. All personnel working with macaques are required to receive information. B. Prevention 1) Protective clothing must be worn in animal facilities (lab coats, scrubs, etc.) 2) Wash hands thoroughly after handling animals, animal tissues or animal fluids. 3) Wear disposable gloves when handling animals, animal tissues or animal fluids. 4) Wear a face mask in all non-human primate, sheep and poultry housing areas. 5) Use and dispose of sharps with care. 6) Allergies to animal dander are common and may increase with long term exposure to animals. Wearing a respirator, face mask and/or gloves may help alleviate allergy symptoms. For information and medical surveillance, contact your primary care physician or the COEM. 7) If you are bitten by an animal and the skin is punctured, or you receive a needle stick: a) Identify the animal species and ID #. b) Clean the wound. c) Report to the COEM, the University Hospital Emergency Room or your private physician. An incident report should be completed by the treating physician. 8) If you are bitten or scratched by a non-human primate or from primate equipment or have any mucous membrane exposed to non-human primate secretions (urine, saliva, etc.): a) Follow the instructions for wound care management found in the “Bite and Scratch Kit” located adjacent to the non-human primate room. b) Immediately report the injury to the DLAR Director or to a DLAR clinical veterinarian. c) Report to the COEM, the University Hospital Emergency Room or their private physician for evaluation for Herpes B infection. An incident report should be completed by the treating physician. C. Clinical 1) A Health History Survey must be completed by all research staff working with animals (see attached survey). The surveys will be assessed by the COEM and the following will be evaluated: a) Tetanus toxoid - valid for 10 years, otherwise a booster will be required (unless medically contraindicated) b) Rabies - 3 doses will be available to employees working with cats, dogs, sheep and other livestock and carnivores. c) TB screening – PPD testing; if PPD is positive, a chest x-ray and referral for further evaluation. d) Measles – available for personnel working with non-human primates. 2) Based on review of the Health History Survey, the COEM will contact personnel directly if additional information or surveillance is needed. 3) When employees are ill or injured, they should inform their primary care physician about their occupational exposure to animals. D. Program Implementation 1) All research staff should receive a copy of the program and a Health History Survey Form. The IACUC will send this information to all Principal Investigators with an IACUC approved animal care and use protocol. The information will also be sent to investigators requesting the IACUC application form. 2) All completed risk assessment surveys must be returned directly to the COEM, who will review information and provide risk assessment. They will also provide, or certify receipt of, vaccinations (if indicated) and medical surveillance. 3) The COEM will forward the names of all research staff who have completed the Health History Survey and have been medically evaluated to the IACUC Office. All medical history information will be kept within the COEM. All personnel listed on a research protocol must have completed the Health History Survey before the IACUC protocol can be approved or renewed. Health History Surveys, risk assessment and medical evaluation will be done annually for all research personnel. Summary of Zoonotic Diseases There are many viral, bacterial, fungal and parasitic diseases of animals that are mildly or severely infective to humans. A few of the most common zoonotic diseases found in the laboratory animal environment are reviewed here. Many laboratory animals are now purchased from commercial vendors who have extensive health prevention programs in place, therefore the risk of exposure has been reduced. The proper use of personal protective equipment (e.g. labcoats, gloves, masks, bonnets, shoe covers) and appropriate training in handling and restraint of laboratory animals can also decrease the risk of acquiring infections by research personnel. Herpes B Virus A viral disease in Macaca sp. (e.g. rhesus, bonnet, cynomolgus monkeys) that is much like Herpes simplex in humans (causing fever blisters). If untreated, Herpes B virus is usually fatal in humans. Treatment with acyclovir® or gancyclovir® has prevented the disease to date but people have to stay on the drug indefinitely. Very few clinical cases reported. Hosts – macaca sp. Common route of infection – bite or scratch from an infected monkey (monkey shows no sign of illness). Also scratches from contaminated equipment. Vaccine available – None Histoplasmosis A fungal disease. Hosts – A variety of species carry histoplasmosis. The agent is found in the dropping of chickens and other birds. Soil may be contaminated with infected droppings. Biologicals – none Important preventive measures – wear a face mask and protective gloves when working with these animals since infection is usually from inhaling organisms. Organisms are aerosolized from dried infected droppings. Lymphocytic choriomeningitis (LCM) A viral disease that can be fatal. No specific treatment is available. Hosts – LCM is most common in wild mice and rats. The agent has been reported in research animal facilities. Most common route of infection – infected urine. The agent has also been transmitted through cell culture. Vaccine available – None. Q Fever Rabies A rickettsial disease caused by Coxiella burnetti. Host – can be found in sheep, goats, cattle, cats, dogs and domestic fowl. The agent is most commonly found in sheep, with pregnant sheep being the greatest hazard. Can be fatal in humans who have valvular heart disease. Animals normally are asymptomatic. Most common route of infection – the agent is shed in the urine, feces, milk, and in amniotic fluids. Inhalation of infectious aerosols is the most common route of infection. Diagnostic testing of animals – titer negative animals may be infected and shed organisms. Important preventative measures – wear protective clothing including mask and gloves when handling sheep or sheep by-products such as placenta, amniotic fluids or stillborn lambs. Personnel with valvular heart disease should limit exposure or have no contact with sheep. A viral disease that is usually fatal if not treated properly and promptly prior to the onset of symptoms. Hosts – dogs, cats and bats account for the largest percentage of human exposures. All warm-blooded animals are susceptible. Route of infection – bite wounds. Vaccine available – vaccines are available for the prevention of rabies for dogs, cats and humans. The DLAR orders only USDA Class A dogs and cats, which are vaccinated against rabies before arrival at the facility. Shigellosis and Salmonellosis Bacterial diseases causing primarily gastrointestinal signs. Hosts – a variety of species, but poultry and non-human primates are the most common carriers. Most common route of infection – oral. Bacterin available – none. Important preventive measures – personnel should wear disposable gloves and/or wash hands frequently when working with these species. Tuberculosis (TB) A mycobacterial disease. Hosts – reported in most mammals and a variety of birds, including pigeons and chickens. Aquatic species can transmit a cutaneous form of the disease. Most common route of infection – inhalation of infected air since the most common site of infection is the lung. TB can also infect the skin, bones, intestines and any other organ system, therefore all excretory products can be infectious in certain cases. Humans and animals are all susceptible to human and animal strains of the mycobacterium. Vaccine available – a bacterium called Bacillus Calmet Gruen (BCG) is available and is used in many countries. Important preventive measures – personnel should wear face masks and disposable gloves when working with these species. Note – There has been a resurgence of TB due in large part to drug users and AIDS victims. New treatment resistant TB strains have been reported.