09 Obstetric hemorrhage in the second half of pregnancy
advertisement

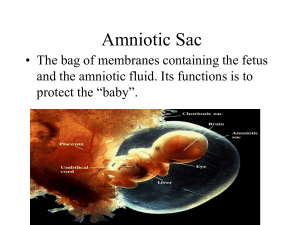
Ministry of Health of Uzbekistan TASHKENT MEDICAL ACADEMY Obstetric hemorrhage in the second half of pregnancy (The text of the lecture) For the 4th year students of medical and medical and pedagogical faculties Tashkent 2013 Obstetric hemorrhage in the II half of pregnancy PURPOSE. To familiarize students with the basic causes of bleeding in the II half of pregnancy, etiology and pathogenesis, symptoms, methods ¬ DAMI relief and prevention in outpatient services. Show that PONRP takes first place among the causes of maternal mortality and perinatal pathology, in connection with which every doctor is not necessary to know ¬ high-risk factors and prevention, emergency care for bleeding in pregnancy. PLAN. 1. Introduction. Relevance. Frequency. 2. Classification of obstetric hemorrhage. 3. PONRP, etiology, classification, symptomatology. 4. Diagnostics. Mode of delivery. Complications. 5. Emergency care and prevention of complications. 6. Risk group of pregnant women for PONRP, methods prevention. 7. Placenta previa. Diagnostics. rendering emergency care. Premature detachment of normally situated placenta Premature detachment of normally situated placenta is a division of ¬ placenta attached to the upper segment of the uterus during pregnancy or whi ¬ in I and II stage of labor. Depending on the size of compartment ¬ loivshegosya plot distinguish partial and full premature otsloy ¬ ku placenta. Clinical manifestations of complications developed if otslai ¬ Vaeth 1/4-1/3 placenta and more. Complication may be due to pre-eclampsia, extragenital pathology primarily kidney (pyelonephritis), diabetes, cardio-vascular disease and other disorders that have the most adverse effects on the peripheral circulatory ¬ Treatment or is the background for the development of hypertensive syndrome. Reports of such etiological factors of premature placental abruption, as trauma and short umbilical cord malodokazatelny. They should be seen as provoking an already existing pathomorphological background. It should be emphasized that the changes of peripheral blood formation in preeclampsia are not only in the utero-placental blood ¬ stream, but also in the vital organs - the liver, kidneys, brain, lungs, dysfunction which essentially determine the symptoms and complications of pregnancy. The deterioration of the micro circulation in the placenta reduces the elasticity of the vascular wall, increasing its permeability. This sposobs ¬ tvuet rupture arterial capillaries, forming micro hematoma, post ¬ merging gradually destroying the basal plate decidual tissue, exciting between villous space and form in placental abruption ever increasing retroplatsentarnoy hematoma. Effused with placental abruption blood diffusely inhibits myometrium up to the visceral peritoneum. Multiple hemorrhages in the thickness of the uterus, edematous swelling of the muscle tissue and the stroma in relation to pre-eclampsia leads to damage of the neuromuscular system mat ¬ ki, violation of its contractility. Blood soaking through the uterus becomes mottled appearance, becomes atonic. This is called the states of coc ¬ uteroplacental apoplexy or uterus Kuvelera by author, first described a similar picture (Couvelaire A. 1912). With all the variety of clinical manifestations of premature compartment ¬ Loic normally located placenta are two types of the course of this complication: 1) the development of generalized bleeding wounds ¬ it through postpartum uterine atony and consumption coagulopathy ¬ tion with the activation of fibrinolysis system 2) with severe functional ¬ tional failure of vital organs (brain, liver, kidneys, lay ¬ KIE), with no bleeding or there is the possibility ¬ sion it relatively easy to stop. Sometimes both options ¬ clinical course who are mixed. The development of a clinical picture depends on the previous background. Placental abruption, accompanied ¬ yuschayasya severe renal failure, pulmonary, stroke, often develops in the recovery or under-treatment of late toxicity and usually occurs during preg ¬ nancy (often premature). Placental abruption with massive bleeding ¬ tion often occurs during childbirth, during the opening of uterine os to 2 cm With significant activation of fibrinolysis, promote bleeding prognosis premature detachment of normally located placenta ¬ zhennoy doubtful. However, it should be recognized that the placental abruption, not accompanied by the activation of fibrinolysis, forecasting an even more unfavorable. In this case, much stronger violation ¬ blood flow, and thus leads to irreversible changes in the vital organs. To factor in the forecast, as relative ¬ syatsya for relatively successful treatment of pathological fibrosis ¬ rinoliza (thanks powerful antifibrinolytic drugs) and at the same time a small efficacy fibrinolizinom. Prevent premature detachment of normally situated placenta can only terminate a pregnancy in a timely manner in case of its long-term complications of hypertension and current severe physical illness. If it is possible to continue the pregnancy, the better the utero-placental circulation reach, using drugs contribute ¬ own normalization of platelet aggregation state and rheology ¬ erties of blood, including the reduction of its viscosity, always high ¬ Coy preeclampsia due to the loss of plasma and the relative increase in erythrocytes. The clinical course of premature detachment of normally located ¬ zhennoy placenta depends on the blood coagulation system (activation or no activation of fibrinolysis), the degree of detachment, the severity of comorbidities (hypertension). Premature detachment of normally situated placenta occurs more frequently in nulliparous women with previous births ¬ is rarely observed. However, the constant backdrop to the development of detachment is oc ¬ hypertensive complications of pregnancy, usually for a long time the current ¬ ing, combined with a particular medical condition. Of somato ¬ České diseases often associated with pregnancy, renal failure, hyper ¬ pertonicheskaya disease, endocrinopathies, including diabetes, obesity and other metabolic diseases. In the course of pregnancy complicated by preeclampsia, often progressing thrombocytopenia. At the same time ¬ me hematocrit and hemoglobin concentration, erythrocyte count is much higher than that of women with placenta previa. Pregnant women who are premature detachment of normally situated placenta is also much more common in intrauterine growth retardation. Acute complication, usually against hypertension varying severity and duration occur rapidly worsening pain, initially ¬ initially localized in the area of the uterus, where the placenta, and gradually extended to the rest of its departments. Pain syndrome is more common in cases of detachment to form retroplatsentarnoy hematoma and uteroplacental apoplexy and can not be expressed (poorly defined) at the end of the blood out. Develops hyper tone of the uterus: it is tense, painful at Pal ¬ dissipation, enlarged, sometimes asymmetrical. These symptoms are also more common in retroplatsentarnoy bruising and less pronounced with a significant external bleeding. Develop symptoms of intrauterine fetal hypoxia or fruit very quickly dies. ¬ there is a definite dependence between the degree of placental abruption, volume retroplatsen ¬ tare hematoma and the degree of tension of the uterus, the fetus. According to the data ¬ nym G.Sber (1980), the appearance of hyper uterine tone indicates that the value retroplatsentarnoy hematoma reached more than 150 ml, and points to the risk of fetal death. In cases of intrauterine fetal death retroplatsentarnoy hematoma volume usually reaches 500 ml or more. When retroplatsentarnoy hematoma volume of 1000 ml or more are necessarily identified ¬ koagulopaticheskogo clinical signs of the syndrome. Vaginal bleeding may be profuse, small or absent altogether. As the volume of blood loss to the clan resolutions are rarely up to 1000 ml due to plugging of the retro placental hematoma, the general condition of patients by developing hyper ¬ yuscheysya volemii at this stage, little disturbed, and clinical manifestations ¬ tion of blood loss may be mild: skin and visible ¬ mye mucous membranes normal color, blood pressure can fall short, and then rise again, but the more common constant high arterial hypertension <170/100-180/110 mmHg and more, in connection with hypertension. That develops moderate ¬ hikardiya. Clinical symptoms of placental abruption can with ¬ putstvovat signs of severe deficiency of vital organs due to pre-eclampsia: oligoanuria, cerebral blood ¬ voobrascheniya, often in the form of symptom complex of pre-eclampsia or coma, etc. These symptoms can be so pronounced that are lead ¬ schimi, disguise placental abruption, especially if there is not at ¬ ruzhnoe bleeding By increasing the time interval from the time of delivery, placental abruption before clinical symptoms may appear incremental consumption coagulopathy with thrombocytopenia: petechial rash on the face and upper limbs, bruising at the injection sites, long ¬ tion bleeding from the injection site, etc. Excessive bleeding usually occurs after the birth of flat ¬ yes (extraction for caesarean section) and is caused by a double violation of hemostasis in the uterus, it atony in combination with acute coagulopathy. ¬ ka mat soaked with blood, loses its ability to contract. Gaping vessels placental site are a constant source of bleeding, blood flows, unable to clot, which contains a very small amount as a result of their prolonged procoagulant previous intravascular consumption. Increased fibrinolytic activity, and Cindy ¬ rum ICE rapidly into IIJ-IV phase. Bleeding can be very strong, takes a generalized and indomitable character: profuse bleeding from the uterus of soft tissue wounds, the wound, venous puncture sites, etc. Common hematoma The detection of small hemorrhages in ¬ ruzhivayut parametrial tissue, fallopian tubes, ligamentous apparatus ¬ those cancer around the injection site on the skin of the neck, trunk, limbs, etc. Duration of the symptoms of coagulopathy during treatment reaches 3-6 hours a rapidly progressive shock, the severity of which increased ¬ tering due to the development of hypo volemii, chronic disorders with degeneration of parenchymal organs due to preeclampsia. Diagnosis abruption normally located pla ¬ cents can be very simple, but may have difficulty if the detachment camouflage comorbidity. Correct diagnosis allows the appearance of bleeding polo ¬ O paths during pregnancy or in early labor amid varying degrees of hypertension, the development of a hyper tone of the uterus, disorders ¬ tion life of the fetus. Diagnosis is difficult in cases when there is no external bleeding ¬ tion, and the patient's condition serious, not only due to placental abruption occurred, but extensive damage to vital organs (coma, anuria, etc.). Diagnosis of placental abruption in these cases ¬ teas help symptoms such as increased tension, stress, lo ¬ locally uterine tenderness, an increase in its volume, signs of fetal life. Considerable potential in the diagnosis of premature detachment of normally situated placenta ultrasound study reveals ¬ tion, which allows to determine the initial stages of this disease. Between the wall of the uterus and the placenta appears echo negative area, indicating the presence of a hematoma. Premature detachment of normally situated placenta should be differentiated from threatening uterine rupture. In patients in whom there was a rupture of the uterus, is often described burdened obstetric and gynecological history. During pregnancy, they have complicated pain in the form of permanent or long-term occasional pain in the abdomen, lower back, in the area of the scar on the uterus or without clear localization ¬ tion. Important components of the treatment of premature detachment of normally situated placenta is to ensure constant contact with us and ve ¬ perform transfusion-infusion therapy, the introduction of tools to facilitate the restoration of peripheral hemodynamics, treatment and prevention of functional impairment of vital organs, etc. From the point of view of patients with premature detachment of normal ¬ mally located placenta is impractical to divide premature detachment of the placenta to the partial and complete. The appearance of clinical symptoms of placental abruption in a hyper tone of disability of the fetus, bleeding, etc. always indicate serious complications irrespective of the placenta by 1/4 - 1/3 full, and thus eliminate the need for its urgent intervention . PRACTICES. First pregnancy 19 years 36 weeks. admitted with complaints of abdominal pain and bleeding from the genital tract, which began 30 min ¬ chickpeas ago. Blood pressure 160/100, protein in the urine, 3.3 g / l, swelling of face, trunk, and legs. Hb 80 g / l, ¬ serdtsebi enie fetus dull. Rhythmical. In an emergency order was in Caesar ¬ section. 2200.0, the girl recovered in asphyxia, animated. PONRP diagnosis is confirmed, the third placenta detached from the edge, no changes in the uterus. Total blood loss 1L, made blood transfusion and infusion of plasma ¬ us. The cause of this disease was severe preeclampsia. Premature birth, timely operation took place, the child is alive. 6.1. Multiparous 38 years enrolled in hemorrhagic shock: BP 70/40 pulse was 120 beats per 1min., Weak filling. Uterus dramatically tense, the fruit is not defined, the heartbeat is not listening. The patient was brought ¬ the neighbors, houses have 4 children, my husband went to Russia for the goods. From the words of the evening, the patient had pain in the stomach, but she was suffering, because there was no one to leave the kids. In the morning it was really bad, she called her neighbor. The patient immediately transferred to the operating room: the two veins ¬ is pouring blood and blood products. Produced by / c removed the dead fetus, free lying placenta and 1.5 kg of blood clots (a 3 liter of blood). The rear wall of the uterus dark purple bluish color, inhibit blood. This is the "queen Kyuvelera." In connection with hemorrhage into the myometrium occurs atony and bleeding from the placental site, is not to cut out the vessels. Therefore performed amputation of the uterus, blood loss, along with the operation of up to 3.5-4 m. From vessels tied translational em ¬ liquid blood that is not being phased out - it's ICE syndrome - koagulopaticheskoe bleeding develops in connection with a large loss of blood, and also due to the fact that more than 6 hours blood clots were retro placental and under great pressure, intrauterine platelet masses began to arrive in the gaping vessels, circulating platelet Plate promoted the formation of blood clots inside the capillary in all parenchymal organs (shock lung, shock kidney, liver shock - remember to pat. Anatomy), even the parietal peritoneum is covered with hemorrhages, POE ¬ that circulate in the blood vessels remains liquid blood - like water from water comes out of it is cut and ligated vessels. Pain ¬ tion of FFP transfused to 120ml of 8 donors, periodically stopped by ICE, but clumps of loose and easily lysed. additional hemostasis. 2n transfused red blood cells from the donor. stabilized blood pressure 100/70 mm Hg ., within 12 hours of doctors fought for his life sick. 3 days later, the patient began a massive transfusion syndrome: hemolysis and oligouriya. Translated into reg. hospital ¬ division of the artificial kidney, and later on the 40th day of renal function recovered. On the day of discharge at 43-D day patient suddenly skoncha ¬ varied from pulmonary embolism. Here it is necessary to know that dialysis was performed by heparin when finished connecting research ¬ artificially kidney was necessary to monitor blood coagulation, as occurs hyper coagulation, and that was the cause of death of the patient. cases show that the late arrival of the patient to the hospital contributed to the development of the uterus and Kyuvelera DIC. Heroic amplification ¬ lence doctors and relatives hardly helped to cope with DIC ¬ nism but further sad outcome. Therefore it is necessary to raise public awareness among the public about the fact that at the slightest pain in the abdomen of a pregnant, an urgent need to hospitalize the patient to the hospital, where specialists will specify the cause of pain - or a P0NRP or premature birth or other pathology and render timely assistance. Thus PONRP - is threatening pathology of the mother and the fetus. Naib ¬ Leia difficult to diagnose placental abruption at the center. Nesvoev ¬ strap treatment of patients in hospitals have deadly conse ¬ tviyam until death. Easier to prevent pathology than to fight it, so in the outpatient general practitioner should allocate pregnant women with high risk factors for PONRP, monitoring and treatment of, antenatal hospitalization to avoid maternal mortality and reduce the incidence of surgical interventions. Placenta praevia Placenta previa (placenta praevia) - attachment of the placenta in the lower uterine segment with partial or complete overlap of its internal cervical os. Distinguish between full, or central ¬ tion (placenta praevia tjtalis s. Centralis), and incomplete (placenta rgaevia partialis) placenta previa. With full placenta previa completely covers the inner mouth, the area of incomplete internal os ¬ him down only a part (lateral previa-placenta praevia lateralis) or the edge of the placenta (marginal previa placenta praevia marginalis). Attachment of the placenta in the lower uterine segment ¬ th, but without capturing the internal os is called low attachment of the placenta. In cases of placenta previa is 5-6 times higher than in general during pregnancy develops its increment (placenta accreta). Even higher frequency of dense attachment of the placenta (placenta adhaerens). Frequent complications of placenta previa with a very unfavorable prognosis ¬ more unlikely is a partial cervical placentation (placenta cervicalis). The frequency of placenta previa is 0.4 - 0.6% of the total number of births. In the etiology of placenta previa are important distrofiches ¬ Kie, inflammatory scarring endometrium that inhibit implantation of the ovum in the uterine wall. Confirm the importance of these factors by high rate of obstetric and gynecological burdened ¬ cal history in pregnant women with placenta previa. Placenta previa rarely develops in the first pregnancy of women who have it may be due to malnutrition of the endometrium in relation to the general and genital infantilism. In recent years, with the development of ultrasound (SPL) placenta previa started to learn from a new angle. ¬ dock was shown the ability to migrate the placenta during pregnancy. The frequency of placenta previa in the II trimester is 8-10 times higher than the beginning of the birth, and that the placenta previa in II or III trimesters gradually migrates from the neck up to the body of the uterus. Placental migration mechanism is not completely clear. Suggested carrying ¬ Kolk assumptions. Migration of the placenta associated with changes in archi ¬ tectonics of the lower segment of the uterus during pregnancy. The influence of this factor on the migration of the placenta, from our point of view finds support in C.Mittelstaedt et al 1979). Authors on the outside ¬ placenta previa, which was located on the front or back wall of the uterus, in the II trimester of pregnancy in 98 pregnant women. By the beginning of birth placenta previa persisted for most women who have placenta was implanted on the back wall of the uterus, whereas at its location on the front of the presentation is almost always eliminated ¬ nyalos. There is also the hypothesis of "dynamic placenta", according to which ¬ swarm during pregnancy there is a microscopic abruptio pla ¬ cents, which is re-attached to other parts of the uterus. As a result of this gradual ¬ area decreases uterine wall, the placenta of the cover ¬: it becomes a more compact. Availability Perma ¬-component processes of placental abruption with hemorrhage found histologically Placenta previa: detected diffuse hyperplasia end villi, edge thrombosis and marginal necrosis of decidual tissue (Naeye R., 1978). Predlezhashey abruption placenta, accompanied by bleeding in late pregnancy is associated with the formation of the lower uterine segment at the end of pregnancy and during labor: maloelastichnaya placental tissue, unable to stretch after stretch of the uterine wall, partially detached and exfoliate. At the same time opened the intervillous space and starts bleeding. Observations showed that the bleeding with placenta previa develops not only closer to the on ¬ chalu birth, but in earlier periods: first, due to the fact previa vetvis ¬ chorion (I trimester) and then, form and branching ho ¬ Rion placenta. Usually in cases of previa branching chorionic preg ¬ variables women are under observation for a long time with a diagnosis threaten ¬ schego abortion. Meanwhile, the cause of bleeding in the previous period ¬ ti Pregnancy is a "dynamic placenta", ie constant branching mikrootsloyka chorion, and then the placenta, resulting in their migration. Thus, the clinic placenta previa describes one ve ¬ duschy symptom - a recurring vaginal bleeding during pregnancy, bleeding may be significant in dilitelnym an amount of blood lost, appears spontaneously in a period of 12 to 40 weeks. pregnancy. After 26-28 weeks. pregnancy bleeding can be carried-induced physical activity, sexual intercourse, defecation, vaginal examination. Placenta previa often described the non-threat of pregnancy, stages of pregnancy, in which there is a threat of miscarriage (from 6 to 33 weeks), suggest that threatening ¬ yuschy abortion can a life backdrop for the presentation formed pla ¬ cents, and vice versa, previa branching chorionic may contribute to threatened abortion. A characteristic feature of placenta previa is a common development in pregnant hypertensive syndrome: 1/3 - 1/4 of them in late pregnancy developed persistent hypotension during initial normotonii. Placenta praevia occurs more frequently in pregnant women older than 30 years who have had abortions or childbirth. Repeated bleeding in pregnancy complicated by placenta previa, reflected on red blood. In this pathology observed the lowest hemoglobin and red blood cells as com ¬ pared with other complications of pregnancy, leading to bleeding ¬ pits. Placentation in the lower uterine segment is reflected in the growth of BCC with ¬. Placenta previa have a high perinatal mortality ¬ sion of children (10-15%). This is due to the fact that with this patho ¬ energy is often a premature birth, abnormal fetal presentation and position.