Antepartum haemorrhage
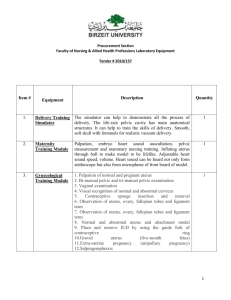
advertisement
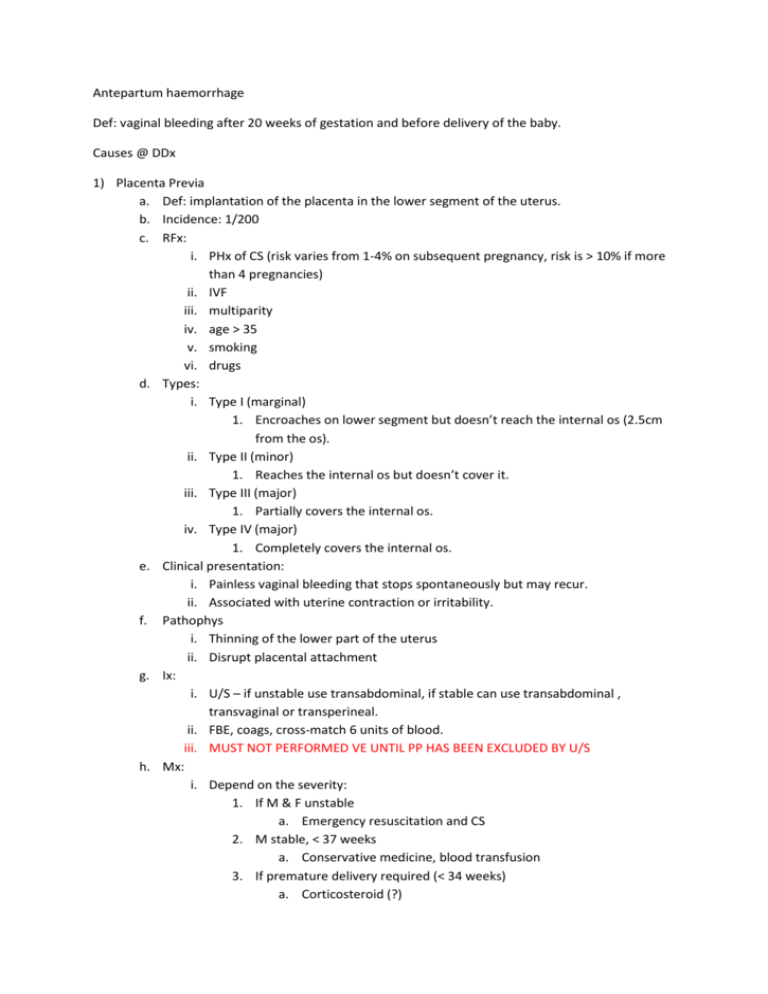
Antepartum haemorrhage Def: vaginal bleeding after 20 weeks of gestation and before delivery of the baby. Causes @ DDx 1) Placenta Previa a. Def: implantation of the placenta in the lower segment of the uterus. b. Incidence: 1/200 c. RFx: i. PHx of CS (risk varies from 1-4% on subsequent pregnancy, risk is > 10% if more than 4 pregnancies) ii. IVF iii. multiparity iv. age > 35 v. smoking vi. drugs d. Types: i. Type I (marginal) 1. Encroaches on lower segment but doesn’t reach the internal os (2.5cm from the os). ii. Type II (minor) 1. Reaches the internal os but doesn’t cover it. iii. Type III (major) 1. Partially covers the internal os. iv. Type IV (major) 1. Completely covers the internal os. e. Clinical presentation: i. Painless vaginal bleeding that stops spontaneously but may recur. ii. Associated with uterine contraction or irritability. f. Pathophys i. Thinning of the lower part of the uterus ii. Disrupt placental attachment g. Ix: i. U/S – if unstable use transabdominal, if stable can use transabdominal , transvaginal or transperineal. ii. FBE, coags, cross-match 6 units of blood. iii. MUST NOT PERFORMED VE UNTIL PP HAS BEEN EXCLUDED BY U/S h. Mx: i. Depend on the severity: 1. If M & F unstable a. Emergency resuscitation and CS 2. M stable, < 37 weeks a. Conservative medicine, blood transfusion 3. If premature delivery required (< 34 weeks) a. Corticosteroid (?) 4. If bleeding stops a. Observation In hospital at least 48 hrs (60% chance to recur) 2) Placental Abruption a. Def: uterine bleeding following premature separation of the placenta from the uterus, total or partial. b. Incidence: 0.5 – 2.0%, 20% perinatal mortality c. RFx: i. Advanced maternal age ii. Multiparity iii. Multipregnancy iv. Smoking v. Drugs (anti coags) vi. Maternal HT vii. PPROM viii. Chorioamnionitis ix. Abdominal trauma x. Maternal thrombophilia xi. PHx of PA xii. IUGR, polyhydramnios xiii. Low SES d. Clinical presentation i. Sx: 1. Abdominal pain (tender tense uterus) 2. Vaginal bleeding (dark, non-clotting) 3. Uterine contraction 4. Usually close to term 5. Nausea, faintness and restlessness Minor Mild VB With or w/o contraction normal Fetal HR Major Sever VB Bleeding from venupuncture sites Bruising (DIC) ii. Sg: 1. 2. 3. iii. Types: 1. Tachycardia, hypotension, signs of peripheral vasoconstriction ‘woody hard’ uterus on palpation, maybe larger than gestation suggests Difficult to palpate fetus Revealed haemorrhage a. VB, pain not significant 2. Concealed haemorrhage a. Slight bleeding, tense uterus, ?pain (due to retroplacental clot) 3. Mixed haemorrhage a. Some VB, some passage of clots, build up of clots behind placenta 4. Large haemorrhage a. Bruised uterus (blood forced into muscle layers) b. IUF demise iv. Dx: 1. Exam placenta after delivery (?send to laboratory for biopsy) 2. U/S – if negative, it doesn’t exclude PA. v. Mx: Minor Emergency CS (stop DIC) Investigate coags on M (APTT, PT, fibrinogen, DDimer) but if results are abnormal consult with haematologist for transfusion Major Conservative or CS Baby is monitored in NICU 3) Vasa Previa a. Def: umbilical vessels run in the membrane close to the internal os instead of the placenta b. Clinical presentataion: i. Small VB at the time of rupture c. Mx: i. CS (because it can cause fetal blood loss) 4) Bleeding from LGT a. Cuases: i. Post coital ii. Cervical condition (ectropion and polyps, carcinoma) iii. Infection (candida, trichomonas)