Genetic Disorders IP Lab
advertisement

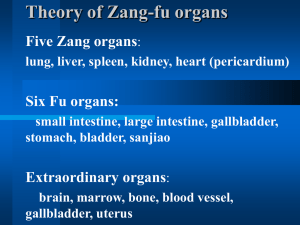
CLASS: 11:00 – 12:00 DATE: November 11 2010 PROFESSOR: Peterson Genetic Disorders (IP LAB) Scribe: Allison O’Brien Proof: Christine Sirna Page 1 of 3 Spleen-Gaucher’s disease (Lysosomal storage disorder) a. a lot of people have this disease b. even though its autosomal recessive kind of look, It “doesn’t know its supposed to be lethal”, meaning there are multiple sites within the gene for glucocerebrosidase that might be affected; DNA segment that encodes for a particular enzyme and there are lots of points along the gene that can result in lysosomal disorder of gangliocytes (glucocerebrocytes). If it affects a later place in enzyme production, you might have enough enzymatic function that you wont die of it-called autosomal recessive adverse (instead of lethal). Majority is not infantile onset where it is lethal (die early because of storage problems in their brains). c. 1st case study-23 year old African American woman delivered stillborn infant C-section, severe bleeding. She has spontaneous bleeding because she is missing platelets. Why is she missing platelets? Large spleen(spleen removes bad RBC, actived platelets) if it is overly large, takes too long to filter, you have overdone your job as a spleen_> functional hypersplenism. This is part of the reason she has low platelet count. But, after taking out her spleen, they discovered she had a hip fracture. Aseptic necrosis means it wasn’t an infection, bone just collapsed. Looked in Bone marrow and determined she had Gaucher’s (neurons and macrophages-Mostly a macrophage problem). Lots of monocytes /macrophages (MQs) in bone marrow. You don’t get rid of them and they take up space for RBC and platelet production particularly for oxygen carrying platelets. Replacement problem in bone marrow. d. Picture-spleen, big. These are the white pulp of the spleen-where MQs generally live. There are Arterioles (penicillar arteries) and around them is the lymphoid follicle stuff to initiate immune response. In Sinusoidsblood channels -RBC have to percolate through have to get out. e. 2 functions of spleen 1-get out platelets, blood cells 2-get an immune response. Here we have Basically have replaced follicles with macrophages. (gaucher’s) f. Spleen is normally red brown.this picture is very pale, kind of friable (fibers that hold together are spread apart because of all the macrophages). g. Picture of normal spleen with arterioles and follicles and here its obliterated-can’t see sinusoids because of proliferation of macrophages. Move forward and look at these cells-literally the whole spleen is a huge conglomerate of macrophages with a fibrillar looking macrophages. Undigested glucocerebrocyte. This is Gaucher’s in a nutshell. *3 different types of Gauchers -Type 1( what this is)-autosomal recessive disorder, but its not complete deficiency of the enzyme, enough function. So dentists be aware of bleeding in patients, could be many things but just keep in mind. Optometrists-Yellowish white inclusions on eye-stuffed macrophages what to look for. -Type 2-infantile onset, severe loss no functional enzyme -Type 3-intermediate; not as bad as type 2 but worse than type 1 II. Lung: Alpha 1 Antitrypsin Deficiency (A1AT) a. Antitrypsin is an enzyme to prevent trypsin from digesting everything –keep tissues from chewing itself up-produced in lung and liver b. these patients are at risk for overdigesting lung tissue c. Case study- 68-year-old white female, was a smoker, afflicted with severe emphysema due to alpha 1-antitrypsin deficiency. Emphysema term used to describe destruction of lung tissue due to damage of tissue (not pneumonia or neoplastic) but from smoking or enzymopathy-she has both. -Lung tissue has elastic fibers in it, when lung tissue is destroyed, elasticity destroyed. You continue to take in air, but keep lungs hyperinflated. Treatment is lobectomy so you have room for expansion. -Tried to do this for her but Post-operatively, she was ventilator dependent and her liver function declined. Further studies revealed hepatic cirrhosis. d. Picture of Lungs-huge, combined lung weight 3500g should be half that size~ 150g good for each organ..Liver 1500 -This has lots of adhesions on the surface, she also blew out=ruptured lung. -Its Heavy because very hemorragic- get with destruction of tissue e. Here is what happened to her lung-these are Alveolar septa- pink (stringy picture)-Lung is a tree-trachea->main stem Bronchii->lobar bronchi->segmental bronchi->subsegmental bronchi on down to terminal bronchiole (finally), this now has a family of respiratory bronchioles. At the end of these are little packages of alveoli (increase SA, “air grapes”) -Everything distal from terminal bronchi is destroyed by smoking. Smoking destroys whole family of tissue. -If you have alpha 1 antitrypsin deficiency-alveoli are destroyed, A1AT destroys leaves, here see 1 instead of 15 that should have. This puts patient at risk for pneumothorax. So this explains her lung damage-Alpha 1 anti-trypsin is supposed to be functioning in the lung a. CLASS: 11:00 – 12:00 Scribe: Allison O’Brien DATE: November 11 2010 Proof: Christine Sirna PROFESSOR: Peterson Genetic Disorders (IP LAB) Page 2 of 3 f. Also got liver damage-micronodular cirrhosis because you are unable to make/process enzyme=destruction of liver tissue Lung and liver are both supposed to produce alpha 1 antitrypsin-damage to both organs without. g. Liver also develops little scars, if you do this enough and stain for mature collagen (remember trichrome stain stains mature collagen blue) this picture the blue shows the scarring, nodular things, this is micronodular cirrhosishappens with A1AT -liver makes all coagulation factors except 1 so your patient will have bleeding tendencies. Most patients diagnosed in childhood and given enzyme replacement. III. Liver: Hemochromatosis-iron coloration going on a. Will probably see this, Good carrier rate among whites. b. You might get this from lots of transfusions because heme is in the RBCs, your spleen (responsible for getting rid of senescent cells) too much iron buildup and get too much iron stored in MQs-that is the secondary type -Primary type actually is an enzymopathy. c. Case study: 61 year old female, liver biopsy (not really the first thing they should do) showed marked Intracellular accumulation of iron, iron is toxic to liver, iron all throughout organs of body -Abnormal glucose tolerance test, iron toxicity in pancreas so can’t make insulin -She got Hepatic failure, jaundice, and died -Liver 800 g. (Picture) 1-liver 2-pancreas. pancreas should be yellow/tan glandular looking thing, this one is red brown throughout because full of iron -Liver is extremely dark, should not be this dark d. Let’s Flashfoward to look at real pathology- notice hepatic lobules but in between them inflammation and scarring. And pigmentation (dark reddish brown color of hepatocytes is not normal color) (pink pic with two black arrows) -Trichrome stain shows scarring-blue; Iron is hepatotoxin-why we get the scarring -How can we look for excess iron-Prussian blue stain-stain iron in nice blue color -Instead of nice pinky tan tissue get Prussian blue when filled with iron Again, primary is enzymopathy. -brownish discoloration of gumline, or around iris of eye-at risk for bleeding tendencies because of cirrhosis of liver..not able to make coagulation factors that they need *Enzyme deficiency causes them to take up more iron from their diet than they need. Unusual for women to get thisMenstruation, men tend to have much higher clinical bronze skin, cardiac failure also ah ah ah oh no mr. bill whikehart to the rescue… andddd we’re back IV- Gout A. Defect in purines in DNA metabolites. Fairly common. B. Gout-deficiency in the ability to get rid of uric acid, inability to excrete uric acid in urine, buildup in blood and crystallizes as little needle like shards in places like joints and peripheral sites on body and worsens when you get cold. Increases crystallization in joints, affects traumatized joints- ankle, feet, big toe, elbow. C. Precipitates from blood are toxic and cause literal mechanical damage to vessels and build little shards called tophi. Swelling of big toe. D. Cause not entirely clear, patients who undergo rapid cell turnover (chemotherapy) are however at risk for gout. E. Dehydration is a problem for these patients and go through episodes of inflammation F. This is a Microscopic picture of tophi with connective tissue scarring around them-pink blobs G. Picture of shards is red pictures.. V. Kidney: Nodular Intercapillary glomerulosclerosis A. Common, Complication of diabetes mellitus-multifactorial disorder (many causes, genes) B. Type 2 diabetes-adult onset, insulin resistance, diet exceeds pancreatic ability to keep glucose in normal range and develop insulin resistance C. Type 1-juvenile onset, insulin dependent, inability to make insulin, more serious problems -Cardiovascular abnormalities and renal problems. This is what this case is about, renal lesion. Diabetes increased incidence of infection (lots of sugar in their blood stream, more likely to have infectious complications and poor wound healing, retinopathy storage material and buildup in retinal vessels=neovascular proliferations. This is what happens to their kidneys-renal failure D. How does this happen? 2 things against them CLASS: 11:00 – 12:00 Scribe: Allison O’Brien DATE: November 11 2010 Proof: Christine Sirna PROFESSOR: Peterson Genetic Disorders (IP LAB) Page 3 of 3 1-Hyperglycemia-going through glomeruli (filtering to get urine through tufts with incomplete cell junctions and fluid leaks out and is specifically modified and goes out as urine-this is normal kidney function) -hyperglycemia cell junctions and ability of golmeruli is altered and can’t do its job. -There is a byproduct of glucose called sorbitol. - Connective tissue of glomerular tuft becomes full of material-expansion, now glomeruli looks smashed against wall called Kenistial Wilsons disease –diabetic renal disease *all the symptomatogly-mycoardial infarction diabetes also have cardiovascular sclerotic disease really profusing kidneys-not sending enough blood and also having to deal with glomerular lesions -poor renal function not able to resorb protein you have let out from plasma leaking through capillaries and lose ability to reabsorb protein-proteinuria -unable to take glucose out of blood stream start to digest muscles=nitrogen problem E. picture-(two balls with black dots) example of glomerular tuft – cellular outline of tubules that function to resorb leaked materials F. These nodular lesions-disease of kidney Can happen in other capillaries also Question: All macrophages are affected-reduce marrow space. [End 41:03 mins]