chapter_28
advertisement

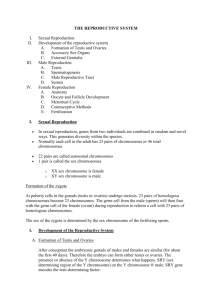
Biology 233 Human Anatomy and Physiology Chapter 28 Lecture Outline REPRODUCTIVE SYSTEM Functions of Reproductive System production of offspring – continuation of species genetic recombination – individual variation, adaptation SEXUAL REPRODUCTION gametogenesis – production of gametes (reproductive cells) female – oogenesis produces oocytes (eggs) male – spermatogenesis produces spermatozoa (sperm) fertilization – male and female gametes united coitus (sexual intercourse) – male gametes transmitted to female prenatal development – development of fetus in uterus GAMETOGENESIS gonads – site of gamete production female – ovaries male – testes Distribution of Genetic Material somatic (body) cells diploid (2N) – contain 23 pairs of chromosomes (total 46) homologous pairs (1 homlog from each parent) gametes (reproductive cells) – oocytes and spermatozoa haploid (1N) – contain 23 unpaired chromosomes zygote – cell produced by fertilization diploid – 23 pairs of chromosomes (total 46) 23 chromosomes from female gamete 23 chromosomes from male gamete Mitosis – cell division which produces 2 identical, diploid daughter cells Interphase – chromosomes replicate to form sister chromatids Prophase – chromosomes condense and become visible Metaphase – chromosomes line up at equatorial plate Anaphase – sister chromatids separate and migrate to opposite poles Telophase – cytoplasm divides to form 2 identical, diploid daughter cells MEIOSIS – 2 stage cell division which produces 4 haploid gametes occurs in gonads gametes produced are not genetically identical to parent cell 1 STAGES OF MEIOSIS: Meiosis I – a diploid cell divides and forms 2 haploid cells Interphase I - chromosomes replicate each chromosome is joined to an identical sister chromatid Prophase I – chromosomes condense, genetic recombination occurs synapsis – pairing of homologous chromosomes tetrad – 4 chromosomes (homologous pair + their sister chromatids) crossing-over – exchange of genes between homologous pairs Metaphase I – homologous chromosomes line up at center Anaphase I – homologous chromosomes separate Telophase I – 2 haploid daughter cells formed each has only one homolog with its sister chromatid Meiosis II – the 2 haploid cells divide again, forming 4 haploid cells Prophase II – chromosomes condense Metaphase II – chromosomes line up Anaphase II – sister chromatids separate Telophase II – 4 haploid daughter cells formed none are identical due to crossing-over MALE REPRODUCTIVE SYSTEM TESTES – male gonads site of spermatogenesis – production of spermatozoa produce male hormones (androgens) develop in abdominal cavity near kidneys Descent of the Testes – testes move out of abdomen and into scrotum begins at about 7th month of fetal development inguinal canals – tunnels through anterior abdominal wall inguinal rings – openings at either end of canal spermatic cord – ductus deferens, blood vessels, and nerves running through inguinal canal to supply testes also surrounded by fascia and muscle scrotum – sac of integument and superficial fascia suspends testes at root of penis scrotal septum divides into 2 halves Purpose of Descent – cools testes normal sperm production requires temperature below body temp regulation of temperature – testes elevated in response to cold dartos muscle – smooth muscle in scrotum cremaster muscle – skeletal muscle in spermatic cord and surrounding testis inguinal hernia – abdominal contents slip through inguinal canal 2 ANATOMY OF TESTES tunica vaginalis – superficial layer; serous membrane covering testis derived from peritoneum tunica albuginea – deep layer; dense irregular connective tissue covers surface of testes and divides it into lobules seminiferous tubules – coiled tubules within lobules sites of spermatogenesis 2 types of cells: spermatogenic cells – form spermatozoa sustentacular (Sertoli) cells – support spermatogenesis secretions – nutrients, chemical stimuli, hormones blood-testis barrier – regulates environment, protects spermatogenic cells from immune destruction phagocytosis Leydig (interstitial)cells – lie between seminiferous tubules secrete androgens – mainly testosterone SPERMATOGENESIS – in seminiferous tubules spermatogonia (stem cells) – diploid attached to basement membrane undergo mitosis – produce many primary spermatocytes 1) primary spermatocyte – diploid undergoes meiosis I 2) 2 secondary spermatocytes – haploid 1 of each homolog + its sister chromatid undergoes meiosis II 3) 4 spermatids – haploid 1 copy of each chromosome spermiogenesis – spermatids differentiate (grow flagellum, etc.) 4) 4 spermatozoa (sperm) – 300mil/day, 65-75 days for development released into lumen of seminiferous tubule sustentacular cell secretions wash sperm out of tubule Anatomy of Spermatozoa head acrosome – tip containing lysosome-like vesicle contains enzymes to penetrate oocyte nucleus – genetic material; haploid midpiece mitochondria – produce ATP for movement centrioles in neck tail flagellum (microtubules) – propels sperm 3 REGULATION OF SPERMATOGENESIS Hypothalamus – Gonadotropin Releasing Hormone (GnRH) released regularly in pulses; stimulates anterior pituitary Anterior Pituitary – gonadotropins (normal blood levels maintained) Luteinizing Hormone (LH) – targets Leydig cells Leydig cells produce testosterone Follicle Stimulating Hormone (FSH) – targets sustentacular cells sustentacular cells secrete androgen-binding protein (ABP) ABP binds testosterone from Leydig cells synergism of FSH and testosterone stimulates spermatogenesis Negative Feedback high testosterone inhibits GnRH release high spermatogenesis rate sustentacular cells secrete inhibin inhibin inhibits FSH release Other Functions of Testosterone prenatal – male reproductive development puberty – maturation of testes and genitals secondary sexual characteristics hair growth pattern, deep voice anabolic – stimulate protein synthesis increase mass of tissues (bone, muscle) behavior and libido (sex drive) MALE REPRODUCTIVE TRACT EPIDIDYMIS – long (20ft) comma-shaped, coiled tube on posterior testis collects sperm from testis site of sperm maturation (10-14 days) – maintain environment that favors development; secretes nutrients, reabsorbs wastes Anatomy of Epididymis: head – superior portion body tail – inferior portion Histology of Epididymis: pseudostratified columnar epithelium stereocilia (long microvilli) – increase surface for secretion and absorption smooth muscle – peristalsis moves sperm forward DUCTUS (VAS) DEFERENS – 18 inch tubule, conducts sperm from epididymis through inguinal canal and pelvic cavity to prostate ampulla – dilated distal end stores sperm – up to several months 4 Histology of Ductus Deferens pseudostratified columnar epithelium 3 layers of smooth muscle – peristalsis moves sperm into urethra EJACULATORY DUCT – 1 inch duct union of ductus deferens and duct from seminal vesicle lies within prostate conducts sperm and seminal secretions to urethra URETHRA – 8 inch duct; carries semen and urine to exterior prostatic urethra membranous urethra spongy (penile) urethra external urethral orifice MALE ACCESSORY GLANDS – secrete seminal fluid (liquid portion of semen) Seminal Vesicles posterior to bladder secretion – alkaline, viscous fluid (60% of semen) neutralizes acidity that is harmful to sperm fructose – ATP source for sperm motility prostaglandins – stimulate sperm motility and smooth muscle contractions in male & female repro. tracts clotting proteins – semen clots after ejaculation Prostate round gland; surrounds superior urethra secretion – milky (30% of semen) seminalplasmin – antibiotic enzyme citric acid – ATP source for sperm proteolytic agents – break down clotting agents Bulbourethral Glands 2 small, round glands in urogenital diaphragm inferior to prostate secretion – alkaline mucus (5% of semen) neutralizes acid in urethra lubricates urethra and end of penis SEMEN sperm + seminal fluid 2-5 ml / ejaculation 50-100 million sperm (<20 mil = likely infertile) slightly alkaline – pH 7.2-7.7; buffers acidity in female repro. tract coagulates within 5 minutes reliquifies after 15-30 minutes 5 PENIS – organ of sexual intercourse transmits sperm to female for fertilization External Anatomy of Penis root – proximal attachment body – main, central portion glans – expanded distal end prepuce (foreskin) – protective skin flap covering glans smegma – waxy secretion from glands of prepuce circumcision – removal of prepuce Cross-Sectional Anatomy of Penis (body) integument - superficial fascia and fibrous connective tissue – middle erectile tissues – deep; contain extensive blood sinuses erection – sexual stimulation dilates arteries to penis blood sinuses of erectile tissues fill expansion of erectile tissues compresses veins penis enlarges and stiffens (vasocongestion) corpora cavernosa – 2 large, dorsolateral columns of erectile tissue; cause erection crura of penis – extensions of cavernosa into root of penis corpus spongiosum – ventral tube of erectile tissue surrounds and prevents collapse of spongy urethra glans – distal enlargement of spongiosum Male Sexual Function arousal – physical and psychological stimuli parasympathetic reflex – vasodilation in penis leads to erection continued stimulation: stimulates glandular secretions and peristalsis in ductus deferens emission – sympathetic reflex triggers contraction of glands discharge of small amount of semen before ejaculation peak stimulation (orgasm) – somatic reflex rhythmic contractions of bulbospongiosus and ischiocavernosus muscles of penis ejaculation – semen propelled from ductus deferens and urethra into vagina FEMALE REPRODUCTIVE SYSTEM OVARIES – female gonads site of oogenesis produce female hormones (estrogens, progestins) lateral to uterus; superior to pelvic brim suspended by ligaments derived from peritoneum 6 ANATOMY OF OVARIES almond-shaped hilus – blood vessels and nerves enter and exit suspensory ligament anchors to pelvic wall germinal epithelium – visceral peritoneum lining surface usually appears cuboidal tunica albuginea – dense irregular CT layer deep to germinal epithelium Ovarian Cortex – outer region ovarian follicles developing oocytes in center of follicle surrounding cells – nourish oocytes and secrete hormones follicular cells – single layer of squamous cells around undeveloped primary oocytes granulosa cells – 1 or more layers of cuboidal cells around developing oocytes; produce secretions dense irregular CT and smooth muscle Ovarian Medulla – inner region loose CT, vessels and nerves OOGENESIS AND FOLLICULAR DEVELOPMENT oogonia (stem cells) – diploid before birth – undergo mitosis; form millions of primary oocytes atresia – most degenerate (about 400 reach maturity) 1) primary oocytes (diploid) – begin meiosis I before birth arrested development – don’t complete meiosis I primordial follicles – single layer of follicular cells around a primary oocyte; found near tunica albuginea OVARIAN CYCLE – begins at puberty hormones activate a group of primordial follicles each month primary follicles follicular cells divide, forming multiple layers of granulosa cells zona pellucida – clear, glycoprotein layer around oocyte thecal cells – CT surrounding follicle; nourishes follicle and helps it produce hormones secondary follicles – a few primary follicles mature to this stage pockets of secretions from granulosa cells surround primary oocyte tertiary follicle – normally only 1 secondary follicle matures to this stage antrum – fluid-filled pocket in center of follicle 2) secondary oocyte – as tertiary follicle develops, the primary oocyte it contains completes meiosis I, forming haploid cells secondary oocyte – 1large cell; receives most of cytoplasm during division first polar body – 1 small, discarded cell with no cytoplasm 7 secondary oocyte begins meiosis II arrested at metaphase II (not completed unless fertilized) corona radiata – crown of granulosa cells around oocyte ovulation – mature follicle ruptures and releases secondary oocyte and its corona radiata into the pelvic cavity normally release 1 oocyte/cycle FATE OF SECONDARY OOCYTE 1) sperm in uterine tube (within 24 hr of ovulation) fertilization – sperm penetrates secondary oocyte oocyte resumes meiosis II – unequal cytokinesis ovum (haploid) – mature egg; large cell second polar body – small, discarded cell nuclei of sperm and ovum unite zygote (diploid) – divides and differentiates to form fetus 2) no sperm in uterine tube degeneration of secondary oocyte and all related structures UTERINE TUBES (oviducts, Fallopian tubes) site of fertilization 4 inch tubes; conduct sperm to secondary oocyte and zygote to uterus Anatomy of Uterine Tubes infundibulum – superior, funnel-shaped portion fimbriae – fringe on border; sweep oocyte into infundibulum ampulla – wide, lateral portion of tube isthmus – narrow, medial portion of tube; connected to uterus Histology of Uterine Tubes mucosa ciliated columnar epithelium – sweeps oocyte through tube secretory cells – nourish oocyte, sperm, and zygote muscularis smooth muscle – peristalsis helps move oocyte serosa – peritoneum UTERUS (womb) – supports the zygote during prenatal development between urinary bladder and rectum size and shape of an inverted pear size depends on sex hormone levels supported by broad ligaments and round ligaments 8 Anatomy of Uterus fundus – broad, superior portion body – central portion cervix – narrow, inferior portion; opens into vagina uterine cavity – interior of uterus Histology of Uterus 1) perimetrium (outer layer) – visceral peritoneum 2) myometrium (middle layer) 3 layers of smooth muscle contracts during childbirth and menstruation 3) endometrium (inner layer) - highly vascular; supports developing fetus simple columnar e. w/ cilia and secretory cells thick lamina propria (endometrial stroma) – areolar CT endometrial glands 2 functional layers: functional zone – lines uterine space develops to support fetus; sloughs during menstruation basal zone – deep layer permanent stem cell layer VAGINA 3-4 inch canal from cervix to exterior of body site of sexual intercourse birth canal outlet for menstrual flow fornix – recessed area surrounding cervical os vaginal orifice – opening to exterior hymen – fold of mucous membrane that partially or completely closes the vaginal orifice in childhood Histology of Vagina 1) mucosa – stratified squamous e./lamina propria rugae – transverse folds normal bacterial flora – create an acidic environment inhibits other microbes (eg. yeast) harmful to sperm – semen buffers acid 2) muscularis – smooth muscle 3) adventitia – loose, fibrous CT VULVA (pudendum) – external genitals mons pubis – bulge due to adipose tissue cushioning pubic symphysis covered by integument and pubic hair 9 labia majora – outer skin folds around vaginal orifice homologous to scrotum labia minora – inner skin folds w/hair around vaginal orifice homologous to spongy urethra – contains erectile tissue clitorus – erectile tissue anterior to vaginal orifice homologous to corpus cavernosum – erectile tissue prepuce covers most of clitorus glans – exposed portion vestibule – region between labia minora vaginal orifice external urethral orifice – between vaginal orifice and clitorus openings of glands – lubricate vestibule and vagina PERINEUM – diamond-shaped area between thighs and buttocks of male or female region of pelvic outlet contains external genitalia and anus boundaries – pubic symphysis, ischial tuberosities, coccyx FEMALE REPRODUCTIVE CYCLE HORMONAL REGULATION Hypothalamus Gonadotropin Releasing Hormone (GnRH) stimulates anterior pituitary Anterior Pituitary Follicle Stimulating Hormone (FSH) stimulates follicle growth stimulates estrogen secretion by follicle cells Luteinizing Hormone (LH) – secreted as estrogens increase stimulates follicle maturation (synergistic with FSH) LH peak triggers ovulation promotes differentiation of follicle after ovulation corpus luteum – granulosa cells differentiate secrete progesterone, estrogens, inhibin Estrogens – synthesized by ovarian follicles from cholesterol functions: development of female reproductive organs in fetus secondary sexual characteristics after puberty fat distribution, breast development, wide pelvis anabolic – promote bone and muscle growth stimulate development of the endometrium 10 Progesterone – secreted by corpus luteum after ovulation acts synergistically with estrogens to build and maintain endometrium supports pregnancy (implantation and nourishment of fetus) prepares mammary glands for milk production feedback inhibition of GnRH = less FSH secretion prevents further follicle development during pregnancy Inhibin – from developing follicles and corpus luteum inhibits FSH secretion delays development of more follicles during ovulation and pregnancy PHASES OF REPRODUCTIVE CYCLE 24-35 days (average 28) 4 phases: 1) Menstrual Phase (day 1-5) no fertilization of oocyte corpus luteum degenerates – becomes corpus albicans (scar) progesterone level declines uterus sloughs functional zone of endometrium menstruation – blood, epithelial cells, mucus low progesterone stimulates GnRH and FSH secretion FSH > LH = follicular development in ovaries 2) Proliferative (Preovulatory) Phase (day 6-13 / variable length) developing follicles secrete estrogens dominant follicle matures others inhibited by inhibin and < FSH (fraternal twins – development of 2 mature follicles) estrogen stimulates growth of functional zone of endometrium maturing follicle produces increasing estrogen level 3) Ovulation (day 14) estrogen peak stimulates GnRH and LH secretion LH peak causes ovulation primary oocyte resumes meiosis – forms secondary oocyte mature follicle ruptures secondary oocyte released (LH level can be used to predict ovulation) 4) Secretory (Postovulatory) Phase (day 15-28) LH stimulates formation of corpus luteum corpus luteum secretes progesterone and estrogen progesterone and estrogens promote secretions of endometrium endometrial glands grow – secrete glycogen (ATP source) endometrial vasculature increases LH > FSH, and inhibin from corpus luteum inhibit follicle development No Fertilization – corpus luteum degenerates to corpus albicans after 2 weeks progesterone, and inhibin levels decline new cycle begins 11 Fertilization human chorionic gonadotropin (hCG) – produced by embryo maintains corpus luteum maintains progesterone and estrogens maintains endometrium to nourish embryo (hCG is detected by early pregnancy tests) Oral Contraceptives synthetic estrogens and progestins feedback inhibition of GnRH and FSH inhibit follicle development MAMMARY GLANDS modified sweat glands within subcutaneous tissue overlying pectoral muscles lactation – secretion of milk following parturition (giving birth) Anatomy of Mammary Gland irregular connective tissue containing adipose suspensory ligaments within CT support breast 15-20 lobes – grape-like clusters of glands lactiferous glands – glands that produce milk stimulated by prolactin + correct levels of progesterone, estrogens, growth hormone, thyroid hormone, etc. regular nursing required to maintain hormone levels lobes drain into lactiferous ducts ----> lactiferous sinuses (expansions that store some milk) ----> lactiferous ducts -----> open in nipple areola – pigmented area around nipple myoepithelial cells – contractile cells in ducts and sinuses contraction expels milk stimulated by oxytocin in response to suckling SEXUALLY TRANSMITTED DISEASES Bacterial Chlamydia – inflammation, pain, sterility Gonorrhea (clap) – inflammation, pus, sterility, blindness in newborn Syphilis primary stage – open sore (chancre) secondary stage – systemic; rash, fever, joint and muscle pain tertiary stage – organ degeneration; may affect nervous system Viral AIDS – immune suppression Genital Herpes – genital blisters and sores; no cure Genital Warts – warts on genitals; may predispose to cancer 12