High_quality_CICU-356-17-08-2010
advertisement
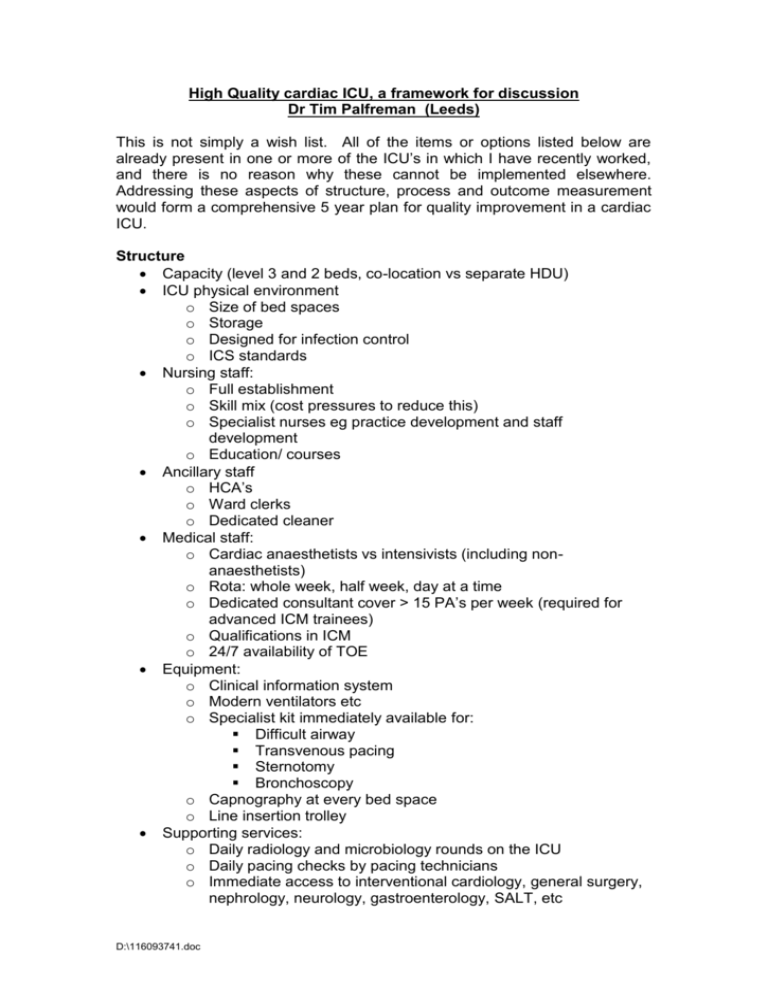
High Quality cardiac ICU, a framework for discussion Dr Tim Palfreman (Leeds) This is not simply a wish list. All of the items or options listed below are already present in one or more of the ICU’s in which I have recently worked, and there is no reason why these cannot be implemented elsewhere. Addressing these aspects of structure, process and outcome measurement would form a comprehensive 5 year plan for quality improvement in a cardiac ICU. Structure Capacity (level 3 and 2 beds, co-location vs separate HDU) ICU physical environment o Size of bed spaces o Storage o Designed for infection control o ICS standards Nursing staff: o Full establishment o Skill mix (cost pressures to reduce this) o Specialist nurses eg practice development and staff development o Education/ courses Ancillary staff o HCA’s o Ward clerks o Dedicated cleaner Medical staff: o Cardiac anaesthetists vs intensivists (including nonanaesthetists) o Rota: whole week, half week, day at a time o Dedicated consultant cover > 15 PA’s per week (required for advanced ICM trainees) o Qualifications in ICM o 24/7 availability of TOE Equipment: o Clinical information system o Modern ventilators etc o Specialist kit immediately available for: Difficult airway Transvenous pacing Sternotomy Bronchoscopy o Capnography at every bed space o Line insertion trolley Supporting services: o Daily radiology and microbiology rounds on the ICU o Daily pacing checks by pacing technicians o Immediate access to interventional cardiology, general surgery, nephrology, neurology, gastroenterology, SALT, etc D:\116093741.doc o Ability to provide short-term VAD support Management structure: o Formal links with ICU users: surgeons, cardiologists, etc o Formal links with other ICU’s in the Trust o Unit clinical governance and operational meetings Involvement of all intensivists Scorecards with key quality and operational indicators Process Closed vs shared model of care Multi-disciplinary ward rounds: o Intensivist o Surgeon o Nurse o Physiotherapist o Pharmacist Documentation: o Admission o Daily assessment o Discharge o Consent o Integrated pathways Clinical guidelines and protocols o Insulin infusion o PAC management o IABP management o Management of pacing wires o Routine post-operative care o etc Routine audit o Hand hygiene o CVC management o Urinary catheter management o Ventilator care bundle o Matching Michigan o Prescribing standards o Antimicrobial use o C. Diff o MRSA bacteraemias o Surgical site infections o Glycaemic control o etc Safety culture o List of triggers for incident reporting o Root cause analysis of significant incidents o Mortality review (modified Birmingham death reporting form) Education: o Induction for every new trainee o Mandatory training Hand hygiene D:\116093741.doc Scrub technique Blood products MRSA, C. diff o Weekly educational meeting (as per syllabus) o Journal club o Formal educational supervision o Accreditation for training advanced ICM trainees Appraisal and revalidation o Covers ICM as well as cardiac anaesthesia Potential Outcome Measures Mortality Surgical site infections Catheter related blood stream infections Drug resistant organism infections (including MRSA) C. difficile infections Chest reopening rate on ICU Unplanned extubation Reintubation rate Readmission within 48 hrs of discharge Serious untoward incidents Length of stay Cancellations Economic indicators Patient satisfaction Family satisfaction Research output Role of ICNARC and cardiac surgical databases Role of the ACTA ICU group o Setting standards o Sharing data for benchmarking o Sharing clinical guidelines and best practice o Sharing innovation o Involvement in guidelines produced by others eg ICS, SCTS D:\116093741.doc