detection and pathogenetic role of mmr missense mutations
advertisement

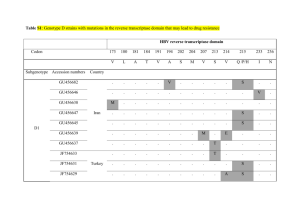
Dottorato di Ricerca in Oncologia – V ciclo Nuova Serie Abstract della tesi di dottorato della dott. Daniela Gagliardini DETECTION AND PATHOGENETIC ROLE OF MMR MISSENSE MUTATIONS Hereditary Nonpolyposis Colorectal Cancer Syndrome (HNPCC Syndrome, or Lynch Syndrome), is an autosomal dominant hereditary cancer syndrome, which accounts for 5% of all colorectal cancers. HNPCC is associated with an increased (90% for men, 70% for women) lifetime risk of endometrial, ovarian and other extra colonic cancers. HNPCC syndrome is defined in clinical terms by the revised Bethesda guidelines and by more stringent Amsterdam criteria. Germline mutations in the MisMatch Repair Genes (MMR) are associated with HNPCC. MMR is a multi-enzymatic system with a main role in genomic stability maintenance, which corrects mismatches generated during DNA replication. Mutations affect mostly the MMR genes MLH1 (50%) and MSH2 (39%). About 50% of these mutations are nonsense variants, which leads to Approximately 32% of MLH1 mutations and 18% of MSH2 mutations are nontruncating missense variants, which lead to a single amino acid substitution, often with an uncertain genetic significance. These alterations may change the shape of the protein or its ability to interact with other MMR components, leading to cancer predisposition, as a consequence of the loss of MMR functionality. The aim of this study was to assess the pathogenicity of MLH1 and MSH2 missense mutations. Ascertainment the causal relationship with the pathology could represent a useful tool in clinical practice and in genetic counselling. Several criteria have been used to address pathogenic significance to these variants; unfortunately, these criteria are frequently insufficient, so several functional assays have been developed. Direct sequencing of the genomic DNA of 118 patients with suspected HNPCC Syndrome was performed. 8 missense mutations in MMR genes were found: 5 alterations of MLH1 (P496R, L559R, K618A, Y646C, P648S), found in 6 patients of unrelated families, and 3 mutations of MSH2 (G162R, D167H, R359S), found in 6 patients, 3 of which belong to the same family. No one of these mutations was listed in the InSiGHT mutation database. Immunoistochemical staining and microsatellite instability (MSI) analysis were performed. The lack of the mutated protein in vivo and a high MSI are the typical hallmarks of HNPCC. To address pathogenic significance to these mutations, functional studies were developed and performed. We tried to set up an in vitro complementation assay, to analyze the ability of MLH1 and MSH2 variants to restore MMR functionality of two MMR- human cell lines, HCT116 and LoVo, respectively MLH1 and MSH2 defective. This functional assay, based on a previous report, showed some design limits, so we tried to improve the test and develop a best one, unsuccessfully. However, test results confirmed HCT116 and LoVo cells as a good model for expression studies. Thus, the expression levels of cloned MLH1 and MSH2 missense mutations, constructed by site-directed mutagenesis and transfected in HCT116 and LoVo cells, were investigated. An in vitro interaction assay was developed, to investigate if MLH1 or MSH2 missense mutations disrupt the protein interaction with the MMR proteins PMS2 or MSH6, respectively. The lack of the formation of functional heterodimers leads to the loss of MMR functionality, suggesting the correlation between the variant and the pathology. The MSH2-MSH6 interaction test showed to be unable to perform MSH2 missense mutations analysis, but the MLH1-PMS2 interaction test showed to be a good tool for analysis of MLH1 variants. Finally, comparative sequence analysis by software SIFT was performed, to assess the value of sequence homology as a tool for predicting functional results. Clinical, genetic, in silico and biochemical data were correlated. All those data permitted to assess a probably pathogenic role to P648S and L559R MLH1 variants, and to exclude the pathogenicity of P496R MLH1 variant. Pathogenicity of K618A and Y646C MLH1 mutations was questionable, as their correlation with HNPCC features was low and results of functional analysis were ambiguous. These results suggests that the MLH1-PMS2 interaction assay developed, together with clinical, genetic and expression analyses, could represent a useful tool to evaluate pathogenicity of MLH1 missense variants.