Learning Guide for Chemical Dependency
advertisement

STUDENT LEARNING GUIDE FOR CHEMICAL DEPENDENCY 1. 2. Does alcohol abuse have a genetic component? Differentiate among intoxication, withdrawal, detoxification, substance abuse and dependency. 3. Describe how tolerance occurs. The body requires larger and larger amounts of the drug to achieve the same effect. 4. Describe the symptoms of substance abuse. 5. From the above list, identify the three defense mechanisms are associated with chemical dependency? Give examples of each. How is minimalization a form of denial? 6. Describe the warning signs of chemical dependency. 7. Describe the personality characteristics associated with chemical dependency. 8. When does alcohol withdrawal begin, peak, and last. When do DT’s usually begin? Begins 4-12 hours after last drink, peaks 2nd day, and lasts for 5 days. DTs usually begin 24 to 72 hours after the last drink. 9. Complete the following table. Drugs Common Manifestations During Use Alcohol, Sedatives, Hypnotics, & Anxiolytics Stimulants (Amphetamines, Cocaine) Cannabis (Marijuana, Hash) Relaxation, mild euphoria, loss of inhibition, decreased motivation, red eyes, dry mouth Opiods Hallucinogens (LSD, Peyote, PCP) 10. Distorted perception, heightened sense of awareness, grandiosity, hallucinations, illusions, distortions of time & space, depersonalization, mystical experiences, dilated pupils, increased blood pressure, increased salivation Describe the effects of alcohol on the major body organs and tissues. Respiratory: Reproductive: Hematologic: Nervous System: Cardiac: Tissue damage due to effects of alcohol on excitability and contractility of heart muscle. Intoxicating amounts of alcohol affect cardiac rate and output and increase both systolic and pulse pressures. Toxicity a causative factor in hypertension. Alcohol contributes to a weakened heart muscle and heart failure. Alcoholic cardiornyopathy, a severe condition with heart failure, shortness of breath, and enlargement of the heart, frequently seen in long-term chronic alcoholics. GI: 11. Complete the following table: Drugs Overdose Manifestations Alcohol Withdrawal Manifestations Treatments for Overdose Tremors, sweating, increased pulse & B/P, nausea, vomiting, and anxiety, seizures. Sedatives, hypnotics, & anxiolytics Stimulants (Amphetamines, Cocaine) Euphoria, hyperactivity, hypervigilance, grandiosity, anger, ↑ B/P tachycardia, chills, chest pain, anorexia, insomnia, fever, nausea, vomiting, diarrhea. dilated pupils Cannabis (Marijuana, Hash Opioids Hallucinogens (LSD, Peyote, PCP) LSD: Talk down. PCP: Do not talk down, Do not use phenothiazine, acidify urine 12. Describe how 12 step programs encourage sobriety. 13. What medications and what vitamin are used in the treatment of ETOH withdrawal and why? 14. What are the effects of alcohol intake, if the client is taking Antabuse? Identify drugs and other preparations that a client may not take if on Antabuse. 15. Why is acamprosate (Compral) used in for ETOH treatment? 16. What medication is used for opiate withdrawal? 17. Why is naltrexone hydrochloride (ReVia, Trexan) used for ETOH treatment? This drug blocks the effects of opiates and reduces alcohol craving. 18. What is a dual diagnosis? The co-occurance of a substance abuse disorder with another psychiatric disorder. 19. Identify three physical and four psychosocial nursing diagnoses for the addicted client. 20. Prioritize the nursing diagnoses and describe the rationale for prioritization. 21. What method did you use to determine priorities? 22. Describe how the nurse intervenes with denial and uses confrontation. Use non-judgmental, supportive approach 23. In order to promote coping skills, the nurse should focus on: 24. Describe how the nurse intervenes with loneliness. 25. Describe how the nurse intervenes with negative self-concept and guilt. 26. Describe the purposes of group and family therapy with the chemically dependent client. 27. Describe the concepts of codependency and enabling as well as the underlying concepts of dysfunctional family theory. Codependency is a maladaptive coping pattern that results in role change. Enabling is a behavior that seems helpful but actually perpetuates substance use. In codependency the codependent takes care of the dependent person and perpetuates the dependency. Family members are not free to be who they are. The family assigns roles to meet the family’s needs. The major problems of the user are never discussed. The elephant in the living room. The roles of the user are abdicated and taken on by the co-dependent. Even with the user no longer abusing the codependent seeks to continue the roles 28. Describe the roles and shifts associated with dysfunctional family theory. Print and bring to class the dysfunctional family diagram. 29. What is the Texas Peer Assistance Program in Nursing? 30. What is your legal obligation to report suspected drug abuse by licensed or non licensed personnel?
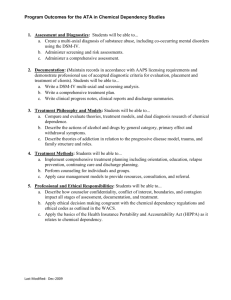




![[#KULRICE-8616] Wrong slf4j-log4j12 version resolved](http://s3.studylib.net/store/data/007509464_1-ab9bda0784a3e51fb3e38df882af1877-300x300.png)