13 Apr 2010 - Benzodiazepine Dependence
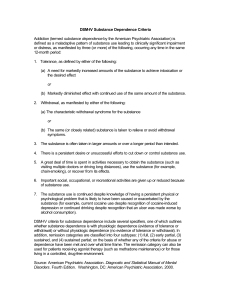
advertisement
Benzodiazepine dependence in primary care Aisha Bhaiyat 13 April 2010 Patient X • • • • 25 yr old male. Previous hx of opiate misuse. Now working as a manager. Needs to fly to attend a meeting in Dublin, for one day. • Is afraid of flying. • Requesting diazepam for the flight there and back. Patient Y • • • • 71 yr old female. Taking diazepam for “nerves”, for decades. Diazapam on repeats. Attended for medication review. Uses • Act on inhibitory GABA receptors to depress CNS • Anxiolytic, sedative, anticonvulsant, muscle relaxant, EtOH/stimulant drug withdrawal, premed anaesthesia Adverse effects • Inevitable tolerance, reduces effectiveness. Results in dosage escalation • Little tolerance to cognitive impairment/amnesia. Risks accidence/falls. • Dependence-continuing treatment then only serves to prevent withdrawal of symptoms which resemble initial complaint • Drug interactions- synergism with EtOH and drugs. Risk of overdose. Tolerance and dependence • Hypnotic effect-within a few days-weeks (after 2/52 of regular use, B become ineffective as sleeping tabs) • Anxiolytic-within 4-6 months (half of those taking for 1 yr or more do so due to dependence rather than B being medically effective) • Anticonvulsant-few weeks • Cognitive impairment/amnesia –very little (so despite effect of BZ decreasing CI/A continue) DSM IV criteria for dependence 3 or more of following • Tolerance –Increasing amount required for desired effect/reduced effect with same amount • Withdrawal • Taken in larger amounts or longer periods than was intended • Persistant desire/unsuccessful effort to cut down • A great deal of time is spent to obtain/use/recover from a substances effect • Social/occupation/recreational effects due to substance use • Substance use is continued despite persistent/recurrent physical/psychological problems due to substance use Withdrawal syndrome • Time lag corresponds to half life • Severity correlates with time used, dose and with short acting and potency of drug • Symptoms of withdrawal resemble the original complaint resulting in a temptation to continuing usage. Patients wanting to stop taking Considerations • Is the patient ready? • Where? By GP or specialist centre? • Advice patients information about undergoing withdrawal and that they will be in control Management of expected withdrawal symptoms • Anxiety-consider slowing withdrawal, nondrug treatment, adjunct treatments (not established practice but may help) • Insomnia-not likely to occur if withdrawal is slow • Psychological interventions Psychological intervention • Counselling to CBT • Key worker through drug and EtOH rehab services • Self help-battle against tranquillizers (www.bataid.org), benzodiazipines cooperation not confrontation (www.bcnc.org.uk), www.nonbenzodiazepines.org.uk Those not wanting to stop taking benzodiazepines • Listen and address their concerns • Discuss tolerance and adverse effects • Encourage dose reduction, even if not stopping Benzodiazipine misusers • Often associated with polysubstance abuse • Medical prescriptions is primary source of supply • Multiple false identities/temporary residents with a story of forgotten or lost medication • GP may worry re confrontation but best not to prescribe • If requesting detox, refer to specialist drug and EtOH service. Possible Effect on children of misusers • • • • • Neglect, physical and emotional abuse Accidents Poverty Frequent changes in residence Presence and availability of toxic substance to the child Tips if prescribing benzodiazipine 1 • Avoid in those with hx of drug misuse/dependence • Prescribe lowest dose and maximum 2 wks • Do not add to repeats • Consider alternatives eg relaxation techniques • Advise patients re adverse effects Tips if prescribing benzodiazipine 2 Advice patients of the following • Advise of risk cognitive impairment eg accidents, effect on driving • Advise of risk of tolerance • Advise of risk of dependence and withdrawal Legal stuff • Class C • Driving- non-prescribed/supratherapuetic dose constitutes dependency/misuse, must inform DVLA • Travel - if more than 3/12 supply then personal import/export licence from UK and letter from prescribing doctor. Patient to contact consulate of country being visited re rules Summary • Distinguish between BZ symptom treatment and chronic dependence • Holistic care • Withdraw gradually • Non drug strategies-patient education, CBT • Adjunct drug therapy-not firmly established (but may be helpful) • Regular follow up of symptoms and dose • Remember legal stuff –driving and travel.