Burns Surgery - Wellington Intensive Care Unit
advertisement
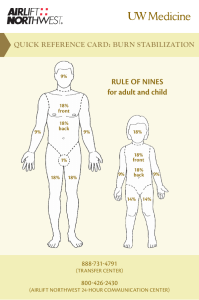
Burns 14/12/10 FANZCA Part II Notes OHOA Data Interpretation - Venkatesh - adults = fire children = scalding maybe associated with ET-OH, abuse, epilepsy or psychiatric problem mortality is related to age (>50yrs), TBSA (40%) burnt and burn depth CLASSIFICATION Superficial – epidermis only Partial – superficial (epidermis and upper layer of dermis), deep (extends to deeper layer of dermis) Full – all layers of dermis and may involve underlying tissue METHODS OF ASSESSING EXTENT Rules of 9’s Palm of patient = 1% TBSA burn Lund-Browder Chart OTHER IMPORTANT ASPECTS Resuscitation – airway patency, breathing, circulation, LOC Adequacy of resuscitation to date – HR, BP, urine output, fluid received Associated trauma Airway burn or inhalational injury – stridor, burns to face, nose and mouth, carbonaceous sputum Facial and/or corneal burns, perineal burns Circumferential burns – extremities -> compartment syndrome, ventilator inadequacy -> escharotomy Rhabdomyolysis Inhalation of toxic gases – CO Temperature Adequacy of analgesia Problems with vascular access Evidence of drug/alcohol ingestion Co-morbid conditions MANAGEMENT EMST/ATLS protocol – primary and secondary survey Burn assessment and management – debridement by 48 hours Transfer to definitive care facility Jeremy Fernando (2011) Primary Survey Airway with C-spine control - may need ETT quickly (use an uncut tube + wire to maxilla) - warning signs include = singed nasal hairs, horse voice, productive brassy cough, soot in sputum, stridor, facial burns, breathed fire, voice change. - maximum wound oedema takes place @ 12-36hrs after injury - FOB or nasoendoscopy - Bronchoscopy - soot, charring, mucosal erythema, necrosis, airway oedema - RSI - sux ok for 24-48hrs then none for 2 days -> 2 yrs - may need AFOI or surgical airway Breathing with O2 - 15L/min + resevior bag - may require ETT + IPPV because of other injuries, major resusication, sedation, ARDS & analgesia, decreased pulmonary compliance - protective lung injury - NAC & heparin nebs - suction Circulation with haemorrhage control - >25% -> SIRS with oedema IV access through intact skin where possible IVF for >15% in adults & >10% in children Hartmans is preferred x-match units may have to stop surgery to catch up aim for PCV 0.3 Disability with assessment of neurological function - CHI CO poisoning ET-OH poisioning analgesia Exposure with temperature control - remove all clothes - if stuck to patient, cut around adherent areas - keep warm - assess %TBSA - 1% = patients palm and fingers - assess burn depth -> superficial = red and painful deep = no capillary refill and not painful - warm theatre (32 C) - humidify (70-80%) Jeremy Fernando (2011) Secondary Survey - cool with running cold water (20min) bronchoscopy for evidence of an inhalational injury (nebulized heparin and NAC) watch for hypothermia cover with clingfilm (limits evaporation, heats loss & pain) IV morphine escharotomy - limbs & chest wall have lots of blood ready watch for COHb -> will need 100% O2 or hyperbaric O2 ICU MANAGEMENT Fluid replacement - required in adult > 15%, children >10% - Modified Parklands Formulae -> Adults - 4mL/kg/% -> Children - 3-4mL/kg/% - give 1/2 in first 8hrs since injury - give 1/2 in next 16hrs + normal maintenance!!! - aim for urine output of 0.5mL/kg/hr and normal cardiovascular parameters - then albumin after first 24 hours (keep albumin > 20) - test for myoglobinuria -> if +ve then (1) aim 1-2mL/kg/hr (2) alkalinise urine with 25mmol of HCO3- for each litre of Hartmans (3) promote diuresis with 12.5g mannitol to each litre of Hartmans Dressings - biobrane: superficial - acticoat: partial - subcut infusions: hypertonic saline + acetic acid (anti-pseudomonal) Other issues - N\J tube -> feed - strict asepsis - vigilance for nosocomial infections: line changes every 7 days - tetanus - antibiotics in initial period if dirty (frequently cooled at scene with dirty water) - family discussion - prognosis: age + TBSA burn should be less than 100. - monitor for post burn leukopenia (cease silver sulfadiazine and use mafenide acetate, stop cimetidine, consider G-CSF if doesn’t improve in 3 days) Jeremy Fernando (2011) Chemical Burns - protect self with gloves, apron & facemask - remove contaminated clothing - neutralize or dilute with H2O (1hr) Hyrdroflouric acid - topical calcuim gluconate burn gel + Biers block with 10-15mL of 10% calcium gluconate + 5000U of heparin in 40mL 5 % dextrose Phosphorus - copper sulphate solution Bitumen - cool with H2O, remove with vegetable or parafil oil Electrical Burns - low voltage (<1000V) -> local contact burn - high voltage (>1000V) -> entrance & exit wound -> may require fasciotomy -> side flash = nearby lightening strike -> superficial burns, entry & exit burns +/respiratory arrest - direct lightening strike -> often fatal Jeremy Fernando (2011)