Global Breast Cancer Facts (interactive map):
advertisement

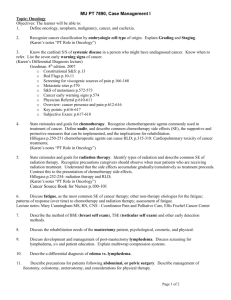
November 3, 2009 at Dana Farber Cancer Institute Offices, 14.15-17.00 THEMATIC WORKING GROUP SESSIONS (pre-registration required) OPTIMIZING HUMAN RESOURCES FOR EARLY DETECTION AND TREATMENT IN DEVELOPING COUNTRIES Co-leaders: Corey Casper, Assistant Professor, Fred Hutchinson Cancer Research Center Gustavo Nigenda, Director, Innovation Services and Health, Center for Health Systems Research, National Institute of Public Health in Mexico Rapporteur: Vinona Bhatia, Medical Oncologist, MPH 2010 Harvard School of Public Health DISCUSSION QUESTIONS 1) What are the necessary human resources for optimizing early detection and treatment for breast cancer in developing countries? a) Primary care physicians and trained nurses in the community i) Examine patients—breast and careful full body clinical examinations ii) Take over the role of the Oncologist in smaller towns/villages b) Midwives and Traditional healers, who can be trained to do clinical breast exams c) Radiologists (screening mammography) d) Pathologists (perform and read biopsies) e) Surgeons (lumpectomy and mastectomy, lymph node dissection) f) Medical and Radiation Oncologists (chemotherapy, hormone therapy, radiation) g) Pharmacists h) Technicians i) Pathology ii) Laboratory iii) Surgical iv) Radiation Therapy i) Community health workers (PIH model) and Traditional Healers i) Finding women in the community with large, neglected tumors ii) Counseling and support after diagnosis iii) Support and follow up during/after treatment iv) Issues of Stigma 1 2) Why are there inadequate human resources for combating cancer in most resourcepoor regions? a) Barriers to specialty training in oncology at all levels – physician, nurses, pharmacists and technicians i) Where could people be trained? (1) Establish centers of excellence locally (2) Send physicians to US and Europe for training (3) Where would resources come from and how much would this cost? b) Inadequate support for human resources by government i) Ugandan Oncologist makes $818 / year ii) Radiation Oncologists in Tanzania but no Medical Oncologist c) Brain drain i) Physicians drawn to more lucrative positions with NGOs and overseas ii) Nurses drawn to developed countries due to nursing shortage d) Lack of Continuing Medical Education e) Poor job satisfaction in Oncology i) Poor conditions ii) Near universal mortality of cancer inpatients iii) Local physicians have not seen the successes of outpatient Oncologic care (1) There are several breast cancer survivors in Kampala 3) How can existing health care systems / financing be harnessed to increase human resources? a) PEPFAR funds, since many cancer patients are HIV+ i) $250 million spent annually in Uganda vs. zero government spending last year on cancer.) b) Partnerships with International NGOs and academic partnerships i) eg, Lance Armstrong Foundation, Clinton Foundation, Gates ii) eg, Harvard, UW, UCSF c) Learn from examples of successful centers i) Uganda Cancer Institute ii) Ocean Road Cancer Institute 4) What capacity needs to be built for ancillary services? a) Laboratories i) Pathology ii) Hematology b) Radiology i) Mammography ii) Ultrasound iii) X-rays iv) CT scanning c) Surgical Oncology i) Clean water d) Radiation Oncology 2 i) Old cobalt machines in Uganda and Tanzania ii) Cost of Linear Accelerators? iii) Radiation induced burns e) Medical Oncology i) Outpatient centers for chemotherapy ii) Chemotherapy education for patients iii) Chemotherapy storage and proper disposal of toxic material iv) Monitoring for hydration/anti-emetic use/other side effects f) Hospital / clinic administration 5) How does a lack of a comprehensive cancer center affect capacity building for human resources? a) Poor metrics lead to unknowns about cancer burden and survival b) Unable to accurately estimate ideal amount human resources needed c) Lack of cancer registry i) Incidence and prevalence of each cancer ii) Age distributions iii) Equity issues d) No death records i) Mortality rates e) Unrealistic to think all cancers can be treated in resource-limited areas…some “rationing” may occur 6) What are the human rights issues with developing human resources? a) What obligation do health care workers in oncology have to be community educators and leaders? i) Will people in resource-poor areas embrace cancer as a significant health care problem? and unlikely to commit resources)? ii) Can a “train the trainer” model be adopted to allow health care workers in Oncology to train others and members of the community? iii) Is it ethical for doctors outside of a cancer center to treat cancer patients? (1) Remote access to experts 3 READING MATERIALS AND RESOURCES Economist Intelligence Unit. Breakaway: The global burden of cancer—challenges and opportunities. 2009 Aug. Available at: http://graphics.eiu.com/marketing/pdf/EIU_LIVESTRONG_Global_Cancer_Burden.pdf Lanata CF. Human Resources in Developing Countries. The Lancet. 14 April 2007;369(9569): 1238-1239. Commentary on Barnighausen article. Available at http://linkinghub.elsevier.com/retrieve/pii/S014067360760573X. (log in required) Anand S, Bärnighausen T. Health workers and vaccination coverage in developing countries: an econometric analysis. The Lancet. 14 April 2007;369(9569):1277-1285. Available at http://www.lancet.com/journals/lancet/article/PIIS0140-6736(07)605996/abstract. Fred Hutchinson Cancer Research Center, Breast Health Global Health Initiative Guidelines for International Breast Health and Cancer Control-Implementation, 2008 Published in: Cancer, Volume 113 Issue S8 , Pages 2215 - 2371 (15 October 2008) Available at http://www3.interscience.wiley.com/journal/121429470/issue. 4