Oncology
advertisement

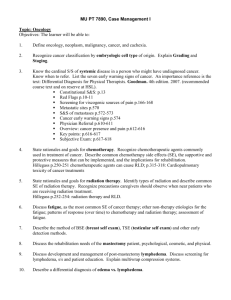
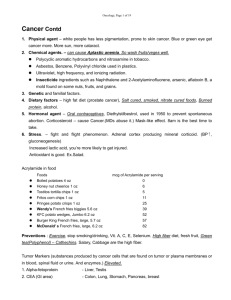
MU PT 7890, Case Management I Topic: Oncology Objectives: The learner will be able to: 1. Define oncology, neoplasm, malignancy, cancer, and cachexia. 2. Recognize cancer classification by embryologic cell type of origin. Explain Grading and Staging. (Karen’s notes “PT Role in Oncology”) 3. Know the cardinal S/S of systemic disease in a person who might have undiagnosed cancer. Know when to refer. List the seven early warning signs of cancer. (Karen’s Differential Diagnosis lecture) Goodman. 4th edition. 2007 o Constitutional S&S: p.13 o Red Flags p.10-11 o Screening for viscogenic sources of pain p.166-168 o Metastatic sites p.570 o S&S of metastases p.572-573 o Cancer early warning signs p.574 o Physician Referral p.610-611 o Overview: cancer presence and pain p.612-616 o Key points: p.616-617 o Subjective Exam: p.617-618 4. State rationales and goals for chemotherapy. Recognize chemotherapeutic agents commonly used in treatment of cancer. Define nadir, and describe common chemotherapy side effects (SE), the supportive and protective measures that can be implemented, and the implications for rehabilitation. Hillegass p.250-251 chemotherapeutic agents can cause RLD; p.315-318: Cardiopulmonary toxicity of cancer treatments; (Karen’s notes “PT Role in Oncology”) 5. State rationales and goals for radiation therapy. Identify types of radiation and describe common SE of radiation therapy. Recognize precautions caregivers should observe when near patients who are receiving radiation treatment. Understand that the side effects accumulate gradually/cumulatively as treatment proceeds. Contrast this to the presentation of chemotherapy side effects. Hillegass p.252-254: radiation therapy and RLD; (Karen’s notes “PT Role in Oncology”) Cancer Source Book for Nurses p.100-101 6. Discuss fatigue, as the most common SE of cancer therapy; other non-therapy etiologies for the fatigue; patterns of response (over time) to chemotherapy and radiation therapy; assessment of fatigue. Lecture notes: Mary Cunningham MS, RN, CNS - Coordinator Pain and Palliative Care, Ellis Fischel Cancer Center 7. Describe the method of BSE (breast self exam), TSE (testicular self exam) and other early detection methods. 8. Discuss the rehabilitation needs of the mastectomy patient, psychological, cosmetic, and physical. 9. Discuss development and management of post-mastectomy lymphedema. Discuss screening for lymphedema, s/s and patient education. Explain multiwrap compression systems. 10. Describe a differential diagnosis of edema vs. lymphedema. 11. Describe precautions for patients following abdominal, or pelvic surgery. Describe management of ileostomy, colostomy, ureterostomy, and considerations for physical therapy. Page 1 of 2 12. Distinguish primary bone cancers from metastatic bone cancers. Name 3 cancers most likely to metastasize to bone. Describe physical therapy in the presence of bone CA (primary or metastatic): pain control vs. safety and mobility. (Cancer Source Book for Nurses p.376-378) 13. Describe the most common brain tumors and medical treatment. Discuss rehabilitation of the patient with primary or metastatic disease affecting brain and / or spinal cord, including appropriate goal setting. Name two cancers that would most likely metastasize to the brain. (Karen’s notes “PT Role in Oncology”) Hill CI, Brain tumors. Phys Ther. 2002;82: 496–502. – posted online) 14. Discuss use of physical therapy modalities in the presence of cancer. (Karen’s notes “PT Role in Oncology”) 15. Demonstrate awareness of Reach to Recovery and other educational programs and support groups for patients and families. 16. Demonstrate recognition of psychosocial, educational and economic implications of cancer for patients, family and friends, health personnel, employers by writing an analysis given a case description. 17. Define palliative care. Discuss pain management for the acute and terminally ill cancer patient. Outline how a patient would qualify for hospice care and the primary purpose of intervention. Understand that palliative care is not exclusive to terminal illness and end of life situations. A person does not have to be no hospice to receive palliative care. The goal of palliative care is to prevent and relieve suffering and to support the best possible quality of life for patients and their families, regardless of the stage of the disease or the need for other therapies. 18. Develop a position on the concepts of "hope" and "coping" relative to the chronically or terminally ill person. Verbalize stages of grief and explain variations in individual grief process. See website resources. 19. Demonstrate understanding of the options within an Advance Directive (AD), and the implication of choices. Appreciate that there is never an option for a person to choose for pain medication to be withheld. Understand the role of the Durable Power of Attorney for Medical Decisions. 20. Describe when an existing Do Not Resuscitate (DNR) order would be applicable or honored. Compare the DNR order and the Advance Directive (AD) in terms of the time frame in which they would be consulted and applied. 21. Differentiate discharge and discontinuation of physical therapy services, as described in The Guide to Physical Therapist Practice. Consider the appropriateness of discontinuation of PT services in the hospice environment. 22. Explain the key questions to ask in order to evaluate pain and pain outcomes. Distinguish between acute and chronic manifestations of pain. Explain the terms: physical dependence, psychological dependence, and tolerance as they relate to the patient with chronic pain. List side effects (SE) of opioids / narcotics. (Mary Cunningham’s lecture notes) 23. Discuss Radical Neck Dissection in Head and Neck Cancer, the risk factors, medical treatment, impairments, acute intervention, rehabilitation for the resulting positional deformity. Which impaired neck and scapulothoracic motions can be compensated, and which cannot? MSH_MUPT_03.06 Page 2 of 2