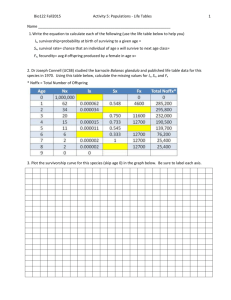
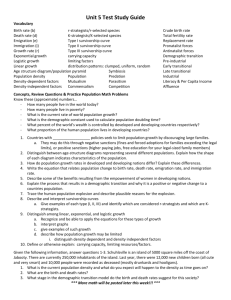
Transcript
advertisement

MODULE 3 TOOLBOX FOR PROVIDING CANCER SURVIVORSHIP CARE Introduction This module will provide an overview of the key elements and evidence based tools and resource to support survivorship care. The specific elements reviewed in this module do not provide an exhaustive list and they are not mutually exclusive. They have been selected to provide exemplars of strategies that you may find useful in providing survivorship care. In this module This module covers Therapeutic Communication- good communication skills and goals they address; Framework for Supportive Care- the tiered Supportive Care model; Multidisciplinary Care- skills required and who’s involved; Survivorship Care Plans- what goes in them and who writes them; Shared Care- how to effectively follow up with the GP Shared Care model; and Promoting Quality in Survivorship Care- implementing and evaluating quality programs. Therapeutic communication Good communication skills are criteria to all aspects of healthcare. Effective communication can reduce stress, feelings of anxiety and uncertainty in individuals. In the context of cancer survivorship, communication serves to address particular goals that are essential to good outcomes. These goals include: identification of individual needs; development of a therapeutic relationship; meeting information needs in regarding diagnosis and treatment plans; reducing distress; and development of the individual’s selfmanagement skills. There are a number of strategies integral to effective communication. Take some time to complete the following activities, to review these strategies and reflect on your skills in these areas. While you’re watching, see how many of the following exemplars of effective communication you can notice. Communication training Communicating with people affected by cancer has been identified as a significant source of stress for cancer specialists. Breaking bad news and feeling inadequately trained to communicate effectively contributes to practitioner stress. There stressors can also extend to communication about survivorship, especially when communicating about the challenges and uncertainty that the cancer survivor may experience. Good communication skills do not necessarily improve over time or with clinical experience, but they can be learned. Approaches which improve communication skills include: communication skills training, organisational changes to improve processes and efficiency, and professional clinical supervision. When you have time, watch the International Psycho-Oncology Society’s Online Curriculum: Communication and Interpersonal Skills in Cancer Care webinar. The webinar takes approximately 45 minutes. Upon completion of the webinar, list 5 changes you could make to your practice to improve communication with cancer survivors. Framework for supportive care Supportive Care interventions can prevent or minimise adverse effects in survivors. Supportive Care embraces the full range of issues that emerge for an individual as the impact of cancer and treatment is felt, and the person tries to deal with the situation. In the context of cancer, Supportive Care includes self-help and support, information, psychological support, symptom control, social support, rehabilitation, spiritual support, palliative care and bereavement care. Fitch defines 5 standards of Supportive Care that provide a useful framework for Survivorship Care, which have been adapted for this module as follows: all individuals receive ongoing Supportive Care needs screening according to need; where necessary individuals receive ongoing supportive care screening; all individuals have the opportunity to be referred to an appropriate Supportive Care resource; all individuals have the opportunity for self referral to Supportive Care resources, all individuals have access to understandable relevant information regarding the medical, practical and emotional aspects of their cancer and its treatment; and all individuals receive Supportive Care that is relevant to their needs and sensitive to their age, gender, language, culture, sexual preferences, religion and economic status. The tiered model of Supportive Care can be useful when developing a plan of care. This model is consistent with the Risk Stratification Approach, recommended for Survivorship Care. More information about the Risk Stratification Approach can be found in Module 2. Framework for supportive care activity Describe specific examples of strategies to meet the following standards for supportive care provision in Survivorship Care: All individuals receive ongoing supportive care screening according to need; and all individuals have the opportunity to be referred to an appropriate Supportive Care resource relevant to their need or preference. In your response, consider screening and assessment tools, clinical resources, support services, multidisciplinary teams, referral pathways and networks. The Supportive Cancer Care Victoria Project developed a suite of resources to guide supportive needs screening and assessment. You can see these 3 links on the screen. The National Cancer Survivorship Initiative in England has a suite of resources including the 2 listed. The Supportive Cancer Care Victoria Project developed a suite of resources to guide supportive needs referral. Multidisciplinary care The importance of the multidisciplinary team during a person’s treatment phase is well recognised. While there has been less attention given to the role of multidisciplinary approaches in cancer survivorship, a multidisciplinary approach is necessary to meet the Supportive Care needs of cancer survivors, and to develop and implement a cancer Survivorship Care plan. Skills that assist healthcare professionals to confidently introduce a multidisciplinary team discussion and approach to Survivorship Care include understanding the purpose and need for a multidisciplinary approach to cancer Survivorship Care, and knowledge of the role of team members. A Cochrane review of interventions to enhance return to work for cancer patients, reported on the significant role of the multidisciplinary team. 3 multidisciplinary interventions involving physical training, in combination with patient education, vocational counseling, training of coping skills regarding return to work, or behavioural biofeedback, suggested that multidisciplinary interventions lead to higher return to work rates than carers usual. Rehabilitative approaches play a role in improving functional outcomes for cancer survivors. Such approaches require a multidisciplinary team. The following diagram illustrates the various contributions of members of the multidisciplinary team to cancer rehabilitation. Faces of cancer rehabilitation Different patients will have different rehabilitation needs depending on the type, location and stage of their cancer. Click on the boxes to see what specialist interventions each team member might deliver. Faces of cancer activity 1 Access the Supportive Cancer Care Victoria resource Scenario 4: Multidisciplinary Team Communication. Louise, a 55 year old, presents after finding a lump in her breast. She has a past history of Hodgkin’s Lymphoma 20 years ago and breast cancer 12 months ago. She’s attending the late effects clinic and requires review by the MDT. Review the interaction demonstrated in the video, and identify strategies which facilitated effective interactions amongst the team. The video goes for about 5 minutes. When you’re finished watching the video, click the button to view a list of elements of effective communication that have been identified. Faces of cancer activity 2 Consider how you would support Louise to meet her Supportive Care needs in your health service. Identify members of the multidisciplinary team in your health service who would be involved in Louise’s care. When you’re finished, click the MDT text to see a list of team members you should consider involving. Faces of cancer activity 3 Describe strategies used in your health service to ensure continuity of care and effective communication between members of the MDT and the cancer survivor. In developing your response, consider the Livestrong Essential Elements recommendations regarding the need for a Care Coordination Strategy. The Care Coordination Strategy provides guidance for what services or activities should be included as part of Survivorship Care and who is responsible for overseeing this care. When you’re finished click anywhere on the screen to see what elements should be included in a Care Coordination Strategy. At a basic level, a care coordination strategy should include: asking or prompting a survivor during a clinic visit to identify other members of the team, maintaining updated contact information for this team in the medical record, providing specific guidance to the survivor on who they should include on their healthcare team, and developing a treatment summary and survivorship care plan which should be shared with all providers of their healthcare. At an enriched level, this strategy is further integrated into an electronic health records system with the ability to document and correspond with all members of the survivor care team. Survivorship care plans Survivorship Care Plans are recommended to achieve an individualised and coordinated approach to survivorship care. Survivorship Care Plans are formal, written documents that provide details of a person’s cancer diagnosis and treatment, potential late and long term effects arising from the cancer and its treatment, recommended follow up and strategies to remain well. Survivorship Care Plans are also a tool to delineate which provider is responsible for which aspect of care. The Institute of Medicine recommends that each person who completes primary treatment for cancer, receive a comprehensive care summary and follow up plan. This needs to be clearly and effectively explained to the survivor. Review the Survivorship Care Plan currently used in your healthcare service. Does it meet the current recommendations identified on the rest of this slide? If your health service does not have a Survivorship Care Plan, access the example from the Australian Cancer Survivorship Centre at the Peter MacCallum Cancer Centre. It is acknowledged that there is variation in opinion regarding ideal content of the Survivorship Care Plan, who might prepare it and how it might be discussed and utilised. Development of the Survivorship Care Plan. The Institute of Medicine recommends that the plan be written by the principle specialists who provided the cancer treatment. The survivor needs to be involved in the development of the Survivorship Care Plan, as care should be responsive to the individual’s goals and needs. The following is some recommendations for content included in Survivorship Care Plans: the cancer for which the survivor receive treatment, short term and long term effects of treatment, screening guidelines and symptoms of cancer recurrence, how the survivor’s follow up care plan will be coordinated, lifestyle changes needed to reduce the risk and severity of treatment side effects, useful community resources should the survivor encounter employment and insurance issues, information about fertility planning for patients of reproductive age, and survivor’s values and preferences regarding their care. Integration of Survivorship Care Plans into electronic health records through automated, programmable applications is an important future goal. Associate Professor Michael Geofford, director of the ACFC cautions that “While the use of care plans might make intuitive sense, or have good face validity, their impact has not been formally evaluated. There are a number of challenges to their routine use, most obviously who will produce the document, how can it easily be tailored to an individual person, who will discuss the document and how should it be used to enhance outcomes for survivors.” We await further evaluation and publication. Shared care Ideally, a shared care model using a Risk Stratified approach can take advantage of the expertise of the cancer team and the primary care provider in coordinating survivor follow up. In a shared care model, cancer survivors continue to have face-to-face, phone or email contact with professionals, as part of continuing follow up. An increasing proportion of follow up care is likely to be performed by primary care teams. Several studies of follow up in primary care, versus secondary care settings, found no statistically significant difference in patient wellbeing and satisfaction, and disease related outcomes, including survival. Improved communication between primary and secondary care has been identified as key to greater general practitioner involvement in Survivorship Care. Click on the link to see the Cancer Council Victoria’s resource- Cancer in General Practice: A Practical Guide for Primary Healthcare Nurses. Shared care activity Watch the video mentioned on the previous slide “Cancer In General Practice: A Practical Guide for Primary Healthcare Nurses- A Focus on Survivorship”, and reflect upon the following issues when watching the experts speak: how can survivors be assured a smooth transition between acute care and general practice, what existing tools and practices can assist the patient’s transition to the survivorship phase, how can primary healthcare nurses best assist patients to ensure that their needs are met, and what are some of the challenges for primary healthcare nurses in providing appropriate care for cancer survivors. You can click the buttons on the screen to see some examples of how these issues may be resolved. Promoting quality in survivorship care Effective translation of guidelines and recommendations to implementation of programs for Survivorship Care requires active planning, systematic prioritisation and system changes to ensure sustainability. This figure outlines one example of the process by which organisations can implement and evaluate survivorship programs. The process is an ongoing and continuous one of evaluation and input. Click on each circle to find out more about each item. Survivorship research Further research is required to develop evidence to support the delivery of effective Survivorship Care to meet survivor needs. In the latest National Comprehensive Cancer Network Survivorship Guidelines, opportunities for research have been identified and these are: linking specific cancer types or treatments with specific late effects; developing increased understanding of the prevalence of, mechanisms of, and risk factors for late and long term effects of cancer and its treatment; defining interventions that relieve symptoms, restore function and improve the quality of life of survivors; and defining optimal follow up and surveillance schedules for cancer survivors after treatment. In Australia, it has also been recommended that progress is needed in the areas of: survivorship issues in the specific populations, the influence of lifestyle factors and behaviors on the health and wellbeing of survivors, and flexible and cost effective models for providing Survivorship Care. Survivorship research activity Identify a program or intervention used to support cancer survivors in your health service. Outline key outcomes which should be assessed in evaluating its impact. In developing your response, you may consider the recommendations outlined in the linked document “Moving Beyond Patient Satisfaction: Tips to Measure Program Impact”. To ensure a comprehensive evaluation of program impact, questions that explore the expected short, intermediate and long term outcomes should be considered. You can click the button to see some of these. In assessing models of care, there are also a number of important elements that have been identified. You can click the button to see these. References 1 These 2 slides contain the list of references used to create this module. Thanks for listening.