Individuals (n= 8893) à Rx > Jul 1, 2005 for ICS/LABA or LAMA
advertisement

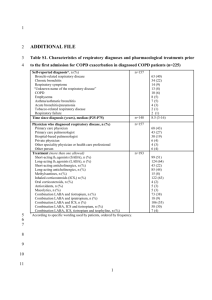
Online Supplement Journal: Drugs Real World Outcomes Title: Severe COPD Exacerbation Risk and Long-Acting Bronchodilator Treatments: Comparison of Three Observational Data Analysis Methods Authors: Melissa H. Roberts, PhDa,b; Douglas W. Mapel, MD, MPHa; Matthew E. Borrego, PhDb; Dennis W. Raisch, PhDb; Larry Georgopoulos, PharmDb; David van der Goes, PhDc a LCF Research, Health Services Research Division, Albuquerque, NM, USA; b University of New Mexico, College of Pharmacy, Albuquerque, NM, USA; c University of New Mexico, Department of Economics, Albuquerque, NM, USA Corresponding Author: Melissa H. Roberts, PhD Email: Melissa.Roberts@LCFResearch.org The COPD and COPD-related International Classification of Disease, 9th Edition (ICD-9) diagnosis codes for this study were: COPD: 491.xx (chronic bronchitis), 492.xx (emphysema), 496 (COPD) COPD-Related: 493.22 (chronic obstructive asthma with acute exacerbation) 493.92 (unspecified asthma with acute exacerbation) 494.1 (bronchiectasis with acute exacerbation) 518.81-518.84 (interstitial emphysema; compensatory emphysema; pulmonary eosinophilia; acute edema of lung, unspecified) Exacerbations The Appendix Table provides the exacerbation definitions. If another exacerbation event occurred within 10 days of the same type of exacerbation event (moderate or severe), it was considered a 1 continuation of the previous exacerbation event. If a severe exacerbation event occurred within 10 days of a moderate exacerbation event, it was counted as a new severe event. Study Population Treatment initiation was indicated by having no outpatient prescription claim for ICS/LABA or LAMA in the 6 months prior to the index date treatment claim. The triple therapy index group consisted of patients with prescription claims for ICS/LABA and LAMA on the same day, or patients with a prescription claim for either ICS/LABA or LAMA and then within 30 days, a prescription claim for the alternate medication. In the latter case, the index date was the date of the first prescription claim. Patients were excluded if in the 12 months pre-index they had an inpatient stay lasting >90 days, were admitted to an inpatient stay within 30 days after the index date, or were enrolled in the health plan for less than 6 months after the index date. Figure 1 provides a summary of the selection process for the study population. Estimated Weights 1 Because the weight is an inverse probability( ), and very low estimated probabilities would result 𝑝 in very large weights, potentially impacting the efficiency of the model, stabilized weights were utilized [13]. Inverse probability for treatment weight (IPTW) values and inverse probability for censoring weight (IPCW) values were estimated using baseline and time-varying covariates and were stabilized by multiplying them by a probability estimated using only baseline factors. The Equation [2, 3] provides the notation for the stabilized weight (SW) for treatment (note that overbars indicate a covariate history), where time periods (k) are measured from time 0 to time t, A(k) represents treatment at time k, and 𝐴(𝑘 − 1) represents the treatment history prior to time k, V represents a vector of time-independent variables (baseline covariates), and 𝐿(𝑘) represents a vector of time-varying covariates through time k (that includes the baseline variables V). 𝑡 𝑆𝑊 = ∏ 𝑘=0 𝑓[A(k)|A(k − 1), V] 𝑓[A(k)|A(k − 1), L(k)] Equation Stabilized Treatment Weight Notation 2 During the follow-up period change of therapy occurred infrequently in the cohort. When both index and prior period treatment were included in regression models, the treatment probability models were overfitted. If analyzed by time period, the c-statistics for logistic regression models were close to 0.90 – with the prior period treatment being the overriding factor for estimating probability of current treatment. Final models therefore only considered the index therapy treatment. The model for probability of treatment actually received for the first period (at index) was constructed separately from the models for the future periods. The IPTW was estimated as the inverse of the probability of receiving the treatment received, adjusted for baseline variables. The stabilizing probability as simply the probability of receiving the treatment received at index; for triple therapy that probability was 0.1139, for the non-triple therapy group, it was 0.8861. Models for treatment at the start of each period after the first period incorporated time-varying covariates which captured post-index events in the prior period. These consisted of moderate exacerbations, inpatient stays that were not deemed severe exacerbations but which had a COPD-related diagnosis code as a secondary diagnosis, and use of SABA medications. Thus, in estimating the inverse probability of treatment weight (IPTW) – the treatment models for periods 2-7 considered baseline characteristics, time-varying covariates prior to the start of the period, index therapy, and a variable for the number of two-week periods that marked the start of the time period since the index date. Models for the stabilizing probability were the same, except without the time-varying covariates. The calculation of the stabilized weight for remaining uncensored is similar to the treatment stabilized weight; however, remaining uncensored, or continuing to utilize a study treatment, is considered on a forward basis, as opposed to looking back as for the IPTW. That is, given use of a study treatment at time t, what is the probability of still using a study treatment at t+1. As was the case for the probability for treatment models, models for remaining uncensored were also different between the first period and later periods. In all censoring models the IPCW weight considered the index therapy, baseline characteristics, and time-varying covariates during the current period.. Censoring models after the first period also considered the number of two-week periods that marked the start of the time period since the index date. The stabilizing probability model was the same as the IPCW model, except without the timevarying covariates. 3 Observation weights were the product of the stabilized treatment and censoring weights. An auto-regressive (AR) correlation matrix was specified for the GEE approach, though estimates were similar between the AR specification and an exchangeable specification. In treatment models that included time-varying covariates, three covariates were included: 1. proportion of the time interval for which the study subject was considered to be having a moderate exacerbation (rounded to .2 – 0.0, 0.2, 0.4, 0.6,0.8, 1.0) 2. number of hospitalizations during the time interval that were not severe exacerbations but for which a COPD-related diagnosis code was listed as a secondary diagnosis 3. any evidence of SABA use during the time interval Censoring models after the first period also incorporated assessments of these time-varying covariates for the prior period. Appendix Figure 2 provides a box plot summary for the range of stabilized weight values, showing minimum and maximum, mean and interquartile range values. When the mean stabilized weights are close to 1.0, the estimated number of study subjects by period should be very close to the actual number, as they are in our study. The mean stabilized weights are close to 1.0, but still include some variation in weights. The distributions showed the most change between the first and second periods, when the greatest numbers of study subjects discontinued therapy. From the second period onward the stabilized weight ranges increased as the time periods progressed. References: [1] Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550-60. [2] Hernan MA, Brumback BA, Robins JM. Estimating the causal effect of zidovudine on CD4 count with a marginal structural model for repeated measures. Statistics in Medicine. 2002;21:1689-709. [3] Faries DE, Kadziola ZA. Analysis of longitudinal observational data using marginal structural models. In: Faries DE, Leon AC, Haro JM, Obenchain RL, editors. Analysis of Observational Health Care Data Using SAS. Cary, North Carolina: SAS Institute; 2010. p. 211-30. 4 Appendix Figure 1 Flowchart of Study Subject Identification Individuals with at least one COPD diagnosis (inpatient or ambulatory [outpatient or ED visit]) Jul 1, 2004 and Sep 30, 2012 (n=48,152) Excluded 1. Individuals with only 1 ambulatory encounter (n= 15,775) 2. Patients without a Rx for ICS/LABA or LAMA >Jul 1, 2005 (n=23,484) Individuals (n= 8,893) Rx > Jul 1, 2005 for ICS/LABA or LAMA Excluded (n= 3,359) 1. Less than 12 months enrollment pre-index 2. Less than 6 months enrollment post-index 3. Prescription for treatment or alternate treatment therapy in 6 months prior 4. Inpatient stay on Index date or within 30 days after index date Individuals (n= 5,534) Potential patients for analysis Excluded (n= 59) 1. Age <40 years at index date (n=49) 2. Inpatient stay >90 days (n=10) Individuals (n= 5,475) Individuals meeting inclusion criteria ICS/LABA = 3,052 (56% of group) LAMA = 1,939 (35% of group) Triple therapy = 484 (9% of group) 5 Appendix Figure 2 Box Plots for Standardized Weights 6 Appendix Table Exacerbation Definitions Prescription claim for an systemic corticosteroid or antibiotic within 3 days of an Moderate ambulatory encounter (outpatient or ED) where there was a COPD or COPDrelated diagnosis associated with the visit Inpatient stay with a primary COPD or COPD-related diagnosis associated with Severe the visit, or a COPD-related DRG (“respiratory infections & inflammations”,” pulmonary edema & respiratory failure”, “chronic obstructive pulmonary disease”) COPD, chronic obstructive pulmonary disease; DRG, diagnosis related group; ED, emergency department