Importance of the inhaler device
advertisement

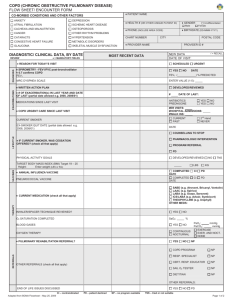
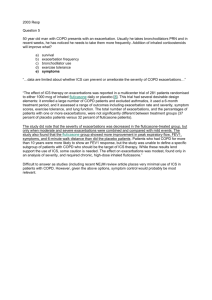
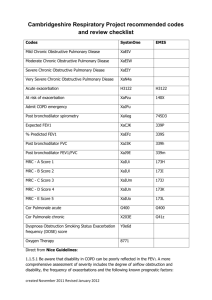
COPD GUIDELINES Sarah Cowdell WHY GUIDELINES MATTER Predicted to be the third leading cause of death by 2030 Cause of over 30,000 deaths in the UK yearly Chronically underdiagnosed – ( by up to 1/3 ) The cause of massive spend in healthcare resources (drugs, bed-days, primary care consultations, workdays lost, comorbidities, mortality. Impact on sufferers and their carers WHATS GOING ON • • • • 2010 NICE update ( Gold Guidance) COPD STRATEGY NICE QUALITY INDICATORS • Oxygen suppliers reprocurement New HOOF /HOCF • New Drugs • Community COPD service • Community referral pulmonary rehabilitation. • ESD • Decomissioned OP secondary care work Wakefield and Kirklees COPD Guidance • • • • Diagnosis of COPD Management of Stable Disease Treatment of Acute Exacerbations Taken from the NICE (2004)2010 update Definition Disease classified by airways obstruction which is not reversible, is usually progressive and does not vary from day today. It will usually occur in smokers or ex smokers over the age of 50. Main symptoms include dyspnoea, cough and sputum production. • Airflow obstruction is defined as a reduction in FEV1/FVC ratio <0.7 • No longer necessary to have FEV1 <80% predicted for definition of airflow obstruction* • If FEV1 is ≥ 80% a diagnosis of COPD should only be made in the presence of respiratory symptoms and/or reduced ratio. • *post bronchodilator Severity Mild Reduced FEV1/FVC, Normal FEV1 Moderate FEV1 50-80% Severe FEV1 30-49% Very severe FEV1 <30% Inhaled therapy Breathless and/or exercise limitation SABA or SAMA as required* FEV1 ≥ 50% FEV1 < 50% Exacerbations or persistent breathlessness LABA LAMA** Offer LAMA in preference to regular SAMA four times a day LABA + ICS in a combination inhaler Consider LABA + LAMA if ICS declined or not tolerated LAMA** Offer LAMA in preference to regular SAMA four times a day LABA + ICS in a combination inhaler Consider LABA + LAMA if ICS declined or not tolerated LAMA + LABA + ICS Persistent exacerbations or breathlessness Offer therapy Consider therapy Thorax February 2011; 66:93-96 Cost implications Fometerol Turbohaler Salmeterol MDI Salmeterol Accuhaler Symbicort Turbohaler Seretide Accuhaler Seretide MDI Tiotropium Handihaler Tiotropium Respimat £23.75 £27.80 £29.26 £38.00 £40.92 £59.58 £34.87 £36.26 Other therapies • Carbocisteine – Reduce exacerbations if chronic sputum production- £16.03 • Theophylline – May improve breathless, may enhance action of ICS- Approx £5.00 • Montelukast – Not recommended for COPD Summary • Bronchodilators improve symptoms • No clear benefit of 1 agent over another • “Adding on” bronchodilators improves symptoms further • Adding on inhaled corticosteroids has a small additional benefit • Importance of the inhaler device Other stuff n.b presence of haemoptysis in a newly diagnosed or otherwise stable pt require urgent fast track referral • • • • Chest x-ray FBC/U&E BMI MRC score/Ex tolerance • Smoking status • Infection frequency • Vaccination • • • • • • • PLAN Treatment level Disease Info SMOKING CESSATION Review frequency Self-management Pulmonary rehabilitation CAT COPD assessment test • • • • • • The CAT provides a reliable measure of the impact of COPD on a patients health status Score 5 – (upper limit of normal in healthy non-smokers) Score <10 (low) » » » » Smoking cessation Annual flu vaccination Reduce exposure to exacerbation risk factors Therapy as warranted by further clinical assessment » » » » Review maintenance therapy Referral for pulmonary rehabilitation Best approaches to minimizing and managing exacerbations Review aggravating factors – is the patient still smoking? » » » Additional pharmacological treatments Referral to pulmonary rehabilitation Ensuring best approaches to minimising and managing exacerbations » In addition to the guidance for patients with low and medium impact CAT scores consider: Referral to specialist care Score 10-20 (medium) Score >20 (high) Score >30 (very high) » Pulmonary Rehabilitation • Offer to all patients who consider themselves functionally disabled by COPD • Make available to all appropriate people, including those recently hospitalised from an acute exacerbation [2010] • Hold at times that suit patients and in buildings with good access Pulmonary rehabilitation • • • • • • Paddock Jubilee Centre Twice weekly for 8 weeks Structured exercise programme Education component MRC score of ≥ 3 Transport cannot be provided 12 months before PR 12 months after PR Change Admissions 9 7 -22% Length of stay (days) 8.5 5.1 -40% Bed days 76.5 35.7 -53% Managing exacerbations • The frequency of exacerbations should be reduced by appropriate use of inhaled corticosteroids and bronchodilators • Give self management advice on responding promptly to symptoms of exacerbation. • Start appropriate treatment with oral steroids and antibiotics • Use of hospital-at-home or assisted-discharge schemes • Use of NIV as indicated EXACERBATIONS • A SUSTAINED WORSENING (+ 24 hours) OF SYMPTOMS REQUIRING A CHANGE IN TREATMENT • • • • CHANGE IN SPUTUM COLOUR INCREASE IN COUGH CHANGE IN VOLUME OF SPUTUM ( LESS OR MORE) INCREASED BREATHLESSNESS OR TAKING LONGER THAN USUAL TO RECOVER FROM USUAL ACTIVITY Amoxicillin 500mg TDS 7 days Prednisolone 30mg OD 7 days Reducing mortality Exacerbations and mortality GLOW3: Seebri significantly improved exercise tolerance on Days 1 and 21 against placebo 600 Exercise endurance time (s) Δ (95% CI): 88.9 (44.7,133.2) seconds, p<0.001 Δ (95% CI): 43.1 (10.9,75.4) seconds, p<0.001 500 400 300 0 Seebri 44 µg o.d. Placebo Day 1 SBH12-C038 Date of Prep October 2012 Seebri 44 µg o.d. Placebo Day 21 Beeh KM et al. International Journal of COPD, 2012;7 5013-513 What’s New? • INDERCATEROL = ONBREZ • GLYCOPYRRONIUM BROMIDE = SEEBREE • ACLIDINIUM = Indercaterol - once daily long acting beta2 agonist Dry powder device GLYCOPYRRONIUM BROMIDE Once daily long acting anti muscarinic MUSCARINIC Aclidinium • Twice daily long acting antimuscarinic • Novel inhaler device Roflumilast • Anti-inflammatory, reduces exacerbations • Not approved by NICE • £37.71 Moderate/severe exacerbations Use of systemic steroids and/or antibiotics Placebo 1.37 Roflumilast 1.14 (ARR -17%) 1.35 1.13 (ARR -16%) The future? • Anti-inflammatories? – Exacerbation reduction – Disease progression? • More combinations of current molecules – Once daily triple therapy in 1 inhaler? http://ckw.wdpct.nhs.uk/documents/long-termconditions/