AAWC Venous Ulcer Guideline Checklist 7.13
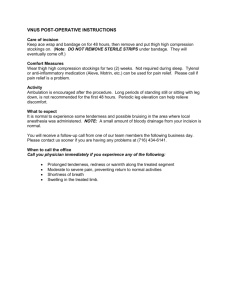
advertisement
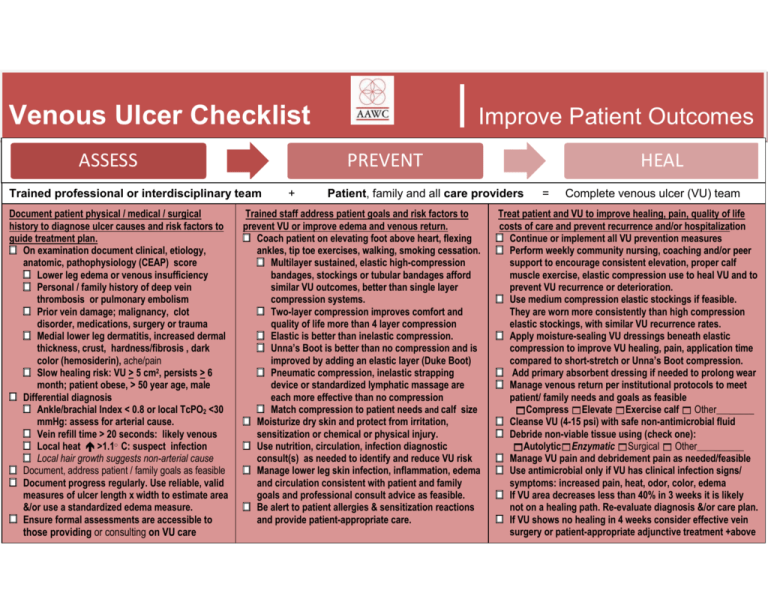
Venous Ulcer Checklist ASSESS PREVENT Trained professional or interdisciplinary team Document patient physical / medical / surgical history to diagnose ulcer causes and risk factors to guide treatment plan. On examination document clinical, etiology, anatomic, pathophysiology (CEAP) score Lower leg edema or venous insufficiency Personal / family history of deep vein thrombosis or pulmonary embolism Prior vein damage; malignancy, clot disorder, medications, surgery or trauma Medial lower leg dermatitis, increased dermal thickness, crust, hardness/fibrosis , dark color (hemosiderin), ache/pain Slow healing risk: VU > 5 cm2, persists > 6 month; patient obese, > 50 year age, male Differential diagnosis Ankle/brachial Index < 0.8 or local TcPO2 <30 mmHg: assess for arterial cause. Vein refill time > 20 seconds: likely venous Local heat >1.1○ C: suspect infection Local hair growth suggests non-arterial cause Document, address patient / family goals as feasible Document progress regularly. Use reliable, valid measures of ulcer length x width to estimate area &/or use a standardized edema measure. Ensure formal assessments are accessible to those providing or consulting on VU care . Improve Patient Outcomes + HEAL Patient, family and all care providers Trained staff address patient goals and risk factors to prevent VU or improve edema and venous return. Coach patient on elevating foot above heart, flexing ankles, tip toe exercises, walking, smoking cessation. Multilayer sustained, elastic high-compression bandages, stockings or tubular bandages afford similar VU outcomes, better than single layer compression systems. Two-layer compression improves comfort and quality of life more than 4 layer compression Elastic is better than inelastic compression. Unna’s Boot is better than no compression and is improved by adding an elastic layer (Duke Boot) Pneumatic compression, inelastic strapping device or standardized lymphatic massage are each more effective than no compression Match compression to patient needs and calf size Moisturize dry skin and protect from irritation, sensitization or chemical or physical injury. Use nutrition, circulation, infection diagnostic consult(s) as needed to identify and reduce VU risk Manage lower leg skin infection, inflammation, edema and circulation consistent with patient and family goals and professional consult advice as feasible. Be alert to patient allergies & sensitization reactions and provide patient-appropriate care. = Complete venous ulcer (VU) team Treat patient and VU to improve healing, pain, quality of life costs of care and prevent recurrence and/or hospitalization Continue or implement all VU prevention measures Perform weekly community nursing, coaching and/or peer support to encourage consistent elevation, proper calf muscle exercise, elastic compression use to heal VU and to prevent VU recurrence or deterioration. Use medium compression elastic stockings if feasible. They are worn more consistently than high compression elastic stockings, with similar VU recurrence rates. Apply moisture-sealing VU dressings beneath elastic compression to improve VU healing, pain, application time compared to short-stretch or Unna’s Boot compression. Add primary absorbent dressing if needed to prolong wear Manage venous return per institutional protocols to meet patient/ family needs and goals as feasible Compress Elevate Exercise calf Other________ Cleanse VU (4-15 psi) with safe non-antimicrobial fluid Debride non-viable tissue using (check one): AutolyticEnzymatic Surgical Other__________ Manage VU pain and debridement pain as needed/feasible Use antimicrobial only if VU has clinical infection signs/ symptoms: increased pain, heat, odor, color, edema If VU area decreases less than 40% in 3 weeks it is likely not on a healing path. Re-evaluate diagnosis &/or care plan. If VU shows no healing in 4 weeks consider effective vein surgery or patient-appropriate adjunctive treatment +above above care.