Pharm Ch 26 Notes [10-2
advertisement

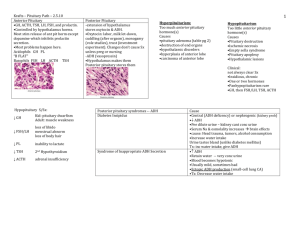
Pharm Ch. 26: Pharm of the Hypothalamus and Pituitary Gland Hypothalamic and Pituitary Physiology Relationship Between the Hypothalamus and Pituitary Gland Anterior pituitary – ectodermal tissue Posterior pituitary (aka neurohypophysis) – ventral surface of diencephalon Hypothalamus controls activity of both lobes o Acts as neuroendocrine transducer, integrates neural signals from brain and converts them into chemical messages (peptides) that regulate pituitary hormone secretion Control of anterior pituitary: hypothalamic-pituitary portal vascular system (indirect vascular connection) o Superior hypophyseal artery fans around axon terminals of hypothalamic neurons – forms initial capillary bed o Fenestrations allows hypothalamic factors to be released into blood stream (hypothalamic pituitary portal system) o Second capillary bed bathes neuroendocrine cells at the AP with hormones secreted by hypothalamus Control of posterior pituitary (direct vascular connection) o Neurons synthesized hormones in cell bodies of the hypothalamic supraoptic and paraventricular nuclei o Hormones transported down axons to the posterior pituitary gland, stored until released; PP – acts as an extension of hypothalamus o Fenestrated endothelial cells also facilitate release Anterior pituitary transcription factors key in development: Pit-1, T-Pit, Prop-1 AP cell types: thyrotrophs, corticotrophs, lactotrophs, somatotrophs, gonadotrophs Relationship btwn hypothalamic releasing factors and pituitary hormones is not always 1:1, and the interaction isn’t always stimulatory o Somatostatin: inhibits release of GH, TSH, prolactin o TH: stimulates TSH release, can also cause prolactin release All known hypothalamic releasing factors are peptides, except dopamine o AP: proteins and glycoproteins 3 groups: Somatotropic hormones: GH, prolactin Glycoprotein hormones: LH, FSH, TSH ACTH Intact peptides and proteins are not absorbed across intestinal lumen, local proteases digest them into their constituent amino acids; this is why therapeutic administration of a peptide hormone or hormone antagonist must be accomplished by a non-oral route (Intro case – octreotide and pegvismant had to be injected) AP gland cell response initiated when hypothalamic factor binds to specific G protein-coupled receptors located in plasma membrane of appropriate anterior pituitary cell o Most receptors alter intracellular cAMP, IP3, and Ca2+ o Ex: GH binds to receptors on somatotrophs, which increases intracellular cAMP and Ca2+ levels; Somatostatin binding to its receptors on somatotrophs decreases intracellular cAMP and Ca 2+ Timing and pattern of hypothalamic release factors important for determining AP cell response o Most hypothalamic RFs are secreted in a cyclical or pulsatile manner (rather than a continuous) Ex: hypothalamus releases pulses of GnRH every few hours, frequency and magnitude of GnRH release determines the extent of pituitary gonadotropin release AND the ratio of LH:FSH secretion Continuous administration of GnRH suppresses rather than stimulates pituitary gonadotroph activity Feedback Inhibition Endocrine axis: each pathway, including a hypothalamic factor, its pituitary gland target cell type, and the ultimate target gland Simplified model, 5 endocrine axes: Generally: systemic hormones produced by target organs negatively regulate the pituitary and hypothalamus to maintain an equilibrium level of hormone release Endocrine diseases are described based on etiology o Primary endocrine disorder – target organ pathology o Secondary endocrine disorder – pituitary disease o Tertiary endocrine disorder – hypothalamic pathology Physio, Pathophysio, Pharm of Individual Axes Anterior Pituitary Gland Hypothalamic-Pituitary GH Axis Regulates general processes that promote growth Somatotrophs of the anterior pituitary gland produce and secrete GH; first expressed at high concentrations at puberty; pulsatile manner, largest pulses at night during sleep Anabolic effects of GH mediated by insulin-like GFs, esp. IGF-1, a hormone release into circulation by hepatocytes in response to stimulation by GH; lots of cell types capable of producing IGF-1, liver contributes majority of detectable IGF-1 IGF-1 is protein bound and stable in the circulation for longer periods of time at steady concentrations, unlike GH; IGF-1 measurements represent an integrated surrogate for GH activity that is stable throughout the day; IGF-1 also better for screening acromegaly Environmental (hypoglycemia, sleep, exercise, adequate nutrition all increase GH secretion) and biological (hypothalamic GHRH, sex steroids [puberty], dopamine, and ghrelin) stimuli regulate GH secretion o Ghrelin acts synergistically with GHRH to promote GH release, acting in a receptor different than the GHRH receptor o Majority of ghrelin secreted by gastric fundal cells during fasting state, linking growth with nutritional status and energy balance Environmental factors that inhibit GH release: hyperglycemia, sleep deprivation, and poor nutritional status Biological factors that inhibit GH secretion are somatostatin, IGF-1, and GH Pathophysio and Pharmacology of Growth Hormone Deficiency Failure to secrete GH or enhance IGF-1 during puberty growth retardation (26-3A-D) GH deficiency usually from defective hypothalamic release of GHRH (tertiary deficiency 26-3D) or from pituitary insufficiency (secondary deficiency 26-3C) However, failure of IGF-1 secretion in response to GH (Laron dwarfism or primary deficiency 26-3B) not amenable to treatment with GH Semorelin: administered to help determine disease etiology; no longer available in U.S. as of 2009 o Alternative exogenous agents to stimulate GH release: glucagon, arginine, clonidine, insulininduced hypoglycemia Tesamorelin: GHRH analogue, augments base and pulsatile GH secretion If a pt. has defective hypothalamic release of GHRH but a normally functioning AP gland somatotrophs, administration of exogenous of exogenous GHRH increases GH release Most cases of GH-dependent growth retardation treated with recombinant human growth hormone (aka somatotropin, generic name); daily subQ/IM injections, $$$, specific use only o Adults: either confirmed GH deficiency or panhypopituitarism (at least 3 hormonal axes affected) Unapproved use in competitive sports o Pediatric: idiopathic short stature, chronic kidney disease, Tuner’s, Prader-Willi Recombinant IGF-1 (mecasermin) effective for pts with GH insensitivity (Laron dwarfism) o Also for pts with w/GH deficiency and antibodies against GH o Adverse effects: hypoglycemia, intracranial HTN Pathophysio and Pharm of GH Excess somatotroph adenoma; rarer: ectopic production of GH or GHRH 2 different disease presentations, depending on whether GH excess occurs before or after closure of bone epiphyses o Gigantism: abnormally high GH secretion before closure of epiphyses be increased IGF-1 levels promote excessive longitudinal bone growth o acromegaly: abnormally high levels of GH after epiphyses close; IGF-1 can still promote growth of deep organs and cartilaginous tissue Somatrotroph adenoma: surgical resection, medical therapy, radiation therapy o Trans-sphenoidal surgical approach is the current SOC; variable success, esp, when adenoma > 1cm, adjuvant medical therapy is frequently required Somatostatin receptor ligands (SRLs) mainstay; somatostatin physiologically inhibits GH secretion, somatostatin itself is not used, half life too short Octreotide and lanreotide – synthetic, longer-acting peptide analogues of somatostatin Somatostatin receptors distributed widely – octreotide can be used for esophageal varices and some hormone-secreting tumors Systemic administration of SRLs adverse effects: Nausea, diarrhea, gallstones, lightheadedness Efficacy of SRLs: they can normalize GH and IGF-1 levels in 60-80% acromegliac patients, and can decrease pituitary adenoma size in 40-40% pts Dopamine – acts mainly on lactrophs to physiologically inhibit prolactin release; also stimulates somatotrophs to release GH under physiologic conditions, pts with acromegaly can have paradoxical decrease in GH secretion in response to dopamine o Maybe bc lactotrophs and somatotrophs have shared embryonic lineage; 20-30% somatotroph adenomas also secrete excess prolactin Bc of this, dopamine analogues bromocriptine and cabergoline sometimes used as adjunctive treatment in acromegaly (dopamine receptor agonists generally much less effective than SRLs, 2nd line agents) GH molecule has 2 binding sites – each of which can bind one GH receptor monomer o GH action requires dimerization of the receptor by GH in order to initiate receptor activation and intracellular signaling o Pegvisomant – GH analogue, binds to GH receptor with higher affinity than native molecule, but the other binding site is inactive; prevents receptor dimerization and intracellular signaling; acts as a competitive antagonist of GH activity; multiple PEG residues which prolong half life and allow once daily dosing; most potent IGF-1 reducing potential, also decreases GH levels by decreasing IGF-1 mediated feedback inhibition of GH secretion Hypothalamic-Pituitary-Prolactin Axis Lactotrophs (AP) produce and secrete prolactin o Inhibited dopamine secretion TRH can enhance prolactin release, also stimulates other thyrotrophs Estrogen and breast feeding also enhance prolactin release Lactotrophs – tonic inhibition by the hypothalamus; disease condition that interrupts the hypothalamic-pituitary portal system decreased secretion of most AP hormones, BUT increased prolactin release o Elevations of prolactin seen in pts taking dopamine receptor antagonists Prolactin secretion not regulated by any (-) feedback Physio actions of prolactin: o Mammary gland development and milk protein biosynthesis and secretion o Normally low in men and non-pregnant women o During pregnancy, increased estrogen stimulates lactotrophs to secrete increasing quantities of prolactin Estrogen antagonizes prolactin action in the breast; prevents lactation until after parturition Suckling – powerful neural stimulus for prolactin release; prolactin levels increase 100x w/in 30 min of breastfeeding; (+) feedback ensures continued replenishment of milk reserves; if mom not breast feeding, prolactin levels decrease over several weeks o Increased prolactin levels suppress estrogen synthesis; antagonize hypothalamic release of GnRH AND decreasing gonadotroph sensitivity to GnRH Decrease in LH and FSH release decreases end-organ stimulation of the hypothalamicpituitary gonadal axis Suppression of estrogen synthesis by prolactin – mechanism to suppress ovulation while a woman is still breast feeding Chronically high secretions of prolactin (prolactinoma) also suppress hypothalamicpituitary-gonadal axis; bc of this, prolactinomas frequently cause infertility, esp. in women who present with oligomenorrhea or amenorrhea o Bromocriptine – synthetic dopamine receptor agonist that inhibits lactotroph cell growth, used for prolactinomas; orally bioavailable Adverse effects: N/V – area postrema in medulla, which stimulates nausea, has dopamine receptors o Cabergoline (U.S.) and quinagolide (Europe) – dopamine receptor agonists, also used to treat prolactinomas; both Category B – bromocriptine still prescribed more frequently Cabergoline: weekly/biweekly dosing, less frequent GI adverse effects; link with valvular heart disease (higher dose therapy used in Parkinson’s, smaller dose for prolactinomas no significant tie to heart disease Hypothalamic-Pituitary-Thyroid Axis Hypothalamus secretes TRH, which stimulates thyrotrophs in the AP to produce and secrete TSH; TSH promotes biosynthesis and secretion of TH by thyroid TH regulates overall body energy and homeostasis; negatively controls hypothalamic and pituitary release of TRH and TSH Thyroid hormone replacement effective treatment for hypothyroidism, TRH and TSH are mainly used to Dx disease etiology o Hypothyroidism bc of unresponsive gland (primary deficiency) serum TSH will be high Serum TSH is the main test used in screening for primary thyroid disease o Hypothyroidism bc of defect in pituitary production (secondary deficiency) TSH will not be high despite low TH levels; if TRH given in this scenario, TSH wouldn’t increase, or it would be significantly reduced Recombinant TSH (thyrotropin) commonly used during radioactive iodine treatment of thyroid cancer; given before radioactive iodine therapy to maximize uptake of radiolabeled 131I isotope into cancerous thyroid Hypothalamic-Pituitary-Adrenal Axis Neurons from paraventricular nucleus of hypothalamus synthesize and secrete CRH, binds to cell-surface receptors on corticotrophs of the AP, stimulates corticotrophs to synthesize and secrete ACTH o ACTH synthesized as part of POMC; along with ACTH, cleavage of POMC MSH, lipotropin, and β-endorphin MSH – skin pigmentation, structurally similar to ACTH, high [ACTH] can bind and activate MSH receptors, important in primary hypoadrenalism – increased ACTH skin pigmentation ACTH stimulates synthesis and secretion of adrenocortical steroid hormones (glucocorticoids, androgens, mineralocorticoids) 26-5A ACTH required for secretion of glucocorticoids and adrenal androgens Mineralocorticoid production also regulated by K+ balance and volume status - ACTH has minor role ACTH trophic affect in zona fasciculata and zona reticularis of the adrenal cortex Excessive ACTH secretion adrenal hyperplasia Deficiency of ACTH adrenal atrophy Cortisol is the most crucial product of steroid biosynthesis Main feedback inhibitor of pituitary ACTH release , “stress hormone”, vascular tone, electrolyte balance, glucose homeostasis Deficiency crucial illness/death; excess Cushing’s Synthetic cortisol, cosyntropin, used to Dx adrenal insufficiency, specifically to determine whether primary of secondary o If primary: administration of cosyntropin will fail to increase plasma [cortisol] bc of inherent dysfunction of adrenal biosynthesis o If new-onset secondary adrenal insufficiency : administration of cosyntropin robust increase in plasma cortisol o Long standing secondary: blunted cortisol response to cosyntropin, mainly due to adrenal cortical atrophy in the absence of trophic effects from ACTH Conditions requiring physiological replacement of glucocorticoids usually treated with synthetic analogues of cortisol, instead of ACTH, bc of more precise control o CRH used as Dx tool in petrosal sinus sampling for ACTH Used to distinguish whether excessive cortisol secretion results from an ACTH-secreting pituitary adenoma or from an ectopic ACTH-secreting tumor Pituitary corticotroph adenoma (Cushing’s Disease) administration of CRH usually increase blood ACTH levels; this response is NOT seen in pts with ACTH-secreting ectopic tumor, which secretes ACTH at an autonomous rate Cushing’s syndrome (primary adrenal tumor) treated with surgical resection Medical therapies: metyrapone, ketoconazole, mitotane – potent inhibitory effects on steroidogenesis, can be used to reduce cortisol production Mifepristone antagonizes peripheral cortisol receptor Hypothalamic-Pituitary-Gonadal Axis Gonadotrophs – secrete LH and FSH (glycoprotein hormones); referred to as gonadotropins Gonadotrophs regulate secretion of LH and FSH independently Gonadotropins control hormone production by gonads; synthesis of androgens and estrogens o Males: gonadotropins inhibited via (-) FB by testosterone o Females: depending on rate of change, absolute [estrogen], stage of menstrual cycle; estrogen can exert both inhibitory and excitatory effects on gonadotropins Inhibin – hormone produced in gonads that has inhibitory effect on FSH secretion, some on LH secretion Activin – paracrine factor produced and acts locally both in the pituitary and in the gonads, function: stimulate FSH production (pituitary gland) Native GnRH (short half life) can be administered in a pulsatile fashion to stimulate patterned gonadotropin release, GnRH analogues with longer half lives are used to suppress production of sex hormones by desensitizing pituitary gland to the stimulating activity of the releasing factor o Leuprolide – most commonly used GnRH agonist, can be administered daily as a subQ injection or as a monthly depot injection, osmotic pump implants available that deliver leuprolide acetate at a controlled rate for up to 12 months o Long acting agonists used to suppress gonadotropins in: endometriosis, uterine fibroids, precocious puberty, androgen dependent prostate cancer o Main drawback: gonadotroph suppression does not occur immediately, transient (several days) increased in sex hormone levels, followed by lasting suppression of hormone synthesis and secretion FSH – clinically used to stimulate ovulation for in vitro o Urofollitropin: purified FSH isolated from urine of postmenopausal women o Follitropin: recombinant from of FSH o Both agents effectively stimulate ovulation by may cause ovarian hyperstimulation syndrome Familial gestational ovarian hyperstimulation syndrome – caused by inherited mutation in the FSH receptor, allows hCG to activate FSH receptor follicular enlargement GnRH antagonists cetrorelix and ganirelix also sometimes used in assisted reproduction o They suppress premature surges in LH in the early to mid-follicular phase of menstrual cycle -> improved rates of implantation and pregnancy o Also have palliative applications for metastatic prostate cancer – avoids initial surge in testosterone caused by treatment with GnRH agonists Posterior Pituitary Gland – secretes ONLY ADH and oxytocin ADH Peptide hormone, produced by magnocellular cells of hypothalamus o Cells in this region have osmoreceptors – sense changes in osmolality Increased osmolality ADH secretion ADH binds to V1 and V2 located in systemic arterioles, mediates vasoconstriction (why its also called vasopressin) V2 receptors located in nephrons stimulate cell surface expression of water channels in order to increase water reabsorption in the collecting duct 2 actions of ADH combine to maintain vascular tone by: 1. Increasing BP 2. Increasing water reabsorption o Disruption of ADH homeostasis: Excessive ADH SIADH ADH secretion occurs irrespective of plasma volume status or osmolality Most common cause: ectopic secretion of ADH by small cell lung carcinoma Persistent stimulation of V1 and V2 receptors HTN and excessive water retention Conivaptan and tolvaptan are vasopressin receptor antagonists approved for SIADH hyponatremia (due to excess water retention) – both available as oral agents o Tolvaptan: specific V2 receptor antagonist approved for heart failure o Conivaptan: mixed V1a and V2 receptor antagonist approved for use in euvolemic and hypervolemic hyponatremia Demeclocycline and lithium also used to treat SIADH Deficient ADH/decreased response to ADH diabetes insipidus Disorder of vasopressin deficiency or resistance Polyuria and polydipsia, secondary to inability to concentrate urine and retain free water at the level of the renal collecting duct o Neurogenic diabetes insipidus: inability of hypothalamic neurons to synthesize or secrete ADH Desmopressin (ADH analogue) stimulated V2 receptors, allows urine to be concentrated and thirst to decrease o Nephrogenic diabetes insipidus: inability of renal collecting duct cells to respond to ADH (aka ADH resistance); Caused by mutation in the V2 receptor or medication-induced (ex: lithium) Treat with diuretics: amiloride or hydrochlorothiazide induce a volume-contracted state, which promotes enhanced absorption of water in proximal tubule and thereby decreased delivery of water to the side of ADH resistance (i.e. collecting ducts) Oxytocin Peptide hormone, produced by paraventricular cells of the hypothalamus Muscular contraction: mile release and uterine contraction Used pharmacologically to induce labor artificially