Alport`s/thin basement membrane disease, pregnancy and proteinuria
advertisement

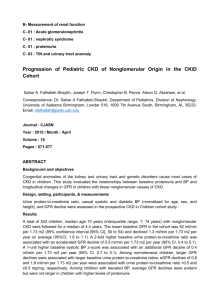
O36 Alport’s/thin basement membrane disease, pregnancy and proteinuria Hall M1, Kapoor D2, Ferraro A1, Wallace S2 Nottingham Renal and Transplant Unit1 and Department of Maternal Medicine2, Nottingham University Hospitals INTRODUCTION: Physiological changes of pregnancy include increased proteinuria to approximately twice baseline levels. Increased renal blood flow can only account for a proportion of this increase. Changes in glomerular capillary permeability and trans-capillary hydrostatic pressure are postulated to account for the rest. Women with chronic kidney disease (CKD) may commence pregnancy with increased protein excretion as a result of their underlying disease. For some, pregnancy can induce nephrotic range proteinuria, nephrotic syndrome and associated complications. We observed that some women with glomerular collagen disorders (Alport’s syndrome (AS) or thin basement membrane (TBM) disease) had particularly pronounced increases in proteinuria. Disease-specific pregnancy outcomes for women with AS/TBM are not well reported. The aim of the analysis is to test the hypothesis that these conditions lead to more pronounced increases in proteinuria than other kidney diseases. METHODS: 7 patients with AS/TBM, 7 patients with other glomerular diseases and 7 patients with non-glomerular CKD were identified from the local Obstetric-Renal service. NonAS/TBM patients were matched for age and baseline creatinine. Baseline values were obtained from preconception laboratory reports. Proteinuria was quantified from spot urine samples as protein:creatinine ratios (P:CR). Women without P:CR quantification but urine dipstick analysis negative for proteinuria were arbitrarily assigned a P:CR of 10mg/mmol. The increase in proteinuria was calculated as the ratio between peak pregnancy proteinuria and baseline proteinuria. Differences between the three groups were compared with one way ANOVA and Bonferroni post-hoc analysis. Values are presented as mean±standard deviation. RESULTS: AS/TBM, other glomerular and non-glomerular CKD patients were well matched for age (27.4±6.3, 27.8±2.2, 23.9±2.6 years respectively, p=0.19), baseline creatinine (75±24, 91±32, 74±14µmol/l respectively, p=0.41) and estimated glomerular filtration rate (CKD-EPI 98±30, 82±27, 102±20 ml/min/1.73m2 respectively, p=0.4). Baseline proteinuria was similar in women with AS/TBM and other glomerular diseases (238±161 vs 103±109 mg/mmol, p=0.14) and higher than in those with non-glomerular diseases (9.6±0.8 mg/mmol, p=0.005). The increase in proteinuria during pregnancy was greater for women with AS/TBM than for women with other glomerular diseases (4.9±3.6 vs 1.3±0.8, p=0.04) and non-glomerular diseases (1.6±1.6, p=0.05). Nephrotic range proteinuria (P:CR>300mg/mmol) during pregnancy was found in 6 (86%) women with AS/TBM, 2 (29%) women with other glomerular diseases and no women with non-glomerular diseases. CONCLUSION: Women with AS/TBM are at high relative and absolute risk of pronounced increases in proteinuria during pregnancy. They should be counselled that this may occur and that prophylactic low molecular weight heparin may be indicated to minimise venous thromboembolic events. Further follow-up data of this cohort will be used to identify the impact of these changes on renal disease progression, and maternal and fetal pregnancy outcomes. Marked changes in circulating angiogenic and antiangiogenic factors have been identified during pregnancy and these are implicated in the pathogenesis of proteinuria in pre-eclampsia. We postulate that changes in these factors particularly affect women with AS/TBM and warrants future study.