Proteinuria and nephrotic syndrome Hamid Moradi M.D. Division of Nephrology and Hypertension
advertisement

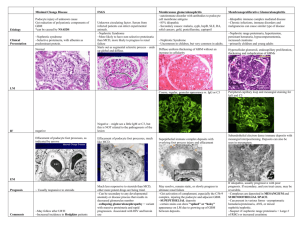
Proteinuria and nephrotic syndrome Hamid Moradi M.D. Division of Nephrology and Hypertension Case- Isolated Proteinuria 22 yo white male without past medical history was noted to have 1+ protein on dipstick on routine UA (health screening for a job) Denies any history of HTN or DM No family history of kidney disease No new medications or over the counter meds No edema on exam Assessing Proteinuria Urinary protein excretion in the normal adult should be less than 150 mg/day. Can increase up to 300 mg with exercise. Higher rates of protein excretion that persist beyond a single measurement should be evaluated?increase in glomerular permeability that allows the filtration of normally nonfiltered macromolecules such as albumin. Isolated proteinuria is defined as proteinuria without hematuria or an elevated serum creatinine concentration. Isolated proteinuria, the patient is asymptomatic and the presence of proteinuria is discovered incidentally by use of a dipstick during routine urinalysis in which the urine sediment is unremarkable. Assessing Proteinuria This is different from renal disease : heavy proteinuria (>3 g/day), edema, active urine sediment with dysmorphic red cells/red cell casts. Annual screening for proteinuria is not cost-effective in the general population of healthy individuals under age 60 routine urinalysis is recommended for high risk patients, including those with diabetes or hypertension. Early detection of proteinuria in high risk patients is important because the administration of an ACEI or ARB has been shown to slow the progression of proteinuric chronic kidney disease. Assessing Proteinuria Types of proteinuria — Glomerular proteinuria — Glomerular proteinuria is due to increased filtration of macromolecules (such as albumin) across the glomerular capillary wall. Only glomerular proteinuria (albuminuria) is identified on dipstick. Most cases of persistent proteinuria are due to glomerular proteinuria. The proteinuria associated with diabetic nephropathy and other glomerular diseases, as well as more benign causes such as orthostatic or exerciseinduced proteinuria fall into this category. Assessing Proteinuria Tubular proteinuria — Low molecular weight proteins — such as ß2-microglobulin, immunoglobulin light chains, retinol-binding protein, and amino acids — have a molecular weight that is generally under 25,000 D in comparison to the 69,000 molecular weight of albumin. These smaller proteins can be filtered across the glomerulus and are then almost completely reabsorbed in the proximal tubule. Interference with proximal tubular reabsorption, due to a variety of tubulointerstitial diseases or even some primary glomerular diseases, can lead to increased excretion of these smaller proteins Assessing Proteinuria Tubular proteinuria is often not diagnosed clinically since the dipstick for protein does not detect proteins other than albumin and the quantity excreted is relatively small. The increased excretion of immunoglobulin light chains (MGUS) in tubular proteinuria is mild, polyclonal (both kappa and lambda), and not injurious to the kidney. This is in contrast to the monoclonal and potentially nephrotoxic nature of the light chains in the overflow proteinuria seen in multiple myeloma. Assessing Proteinuria Overflow proteinuria — Increased excretion of LMW proteins due to marked overproduction of a particular protein, leading to increased glomerular filtration and excretion. Almost always due to immunoglobulin light chains MM, but may also be due to lysozyme (in acute myelomonocytic leukemia), myoglobin (in rhabdomyolysis), or hemoglobin (in intravascular hemolysis) In these settings, the filtered load exceeds the normal proximal reabsorptive capacity. Patients with myeloma kidney also may develop a component of tubular proteinuria, since the excreted light chains may be toxic to the tubules, leading to diminished reabsorption. Assessing Proteinuria Some patients have mixed forms of proteinuria. As an example, glomerular diseases such as focal segmental glomerulosclerosis can be associated with proximal tubular injury, leading to tubular proteinuria. In addition, patients with multiple myeloma and Bence Jones proteinuria can also develop nephrotic syndrome due to AL (primary) amyloidosis. Case Repeat UA on the 22 yo man revealed 1+ proteinuria on dipstick, How should we quantify the proteinuria? Assessing Proteinuria The standard urine dipstick primarily detects albumin via a colorimetric reaction between albumin and tetrabromophenol blue producing different shades of green The dipstick is insensitive to the presence of non-albumin proteins. Thus a positive dipstick usually reflects glomerular proteinuria. Pure tubular or overflow proteinuria will not be diagnosed unless a 24hour urine is collected for some other reason, or the urine is tested with sulfosalicylic acid which detects all proteins. Assessing Proteinuria Proteinuria on the urine dipstick is graded from 1+ to 4+, which reflects the urine albumin concentration: Negative Trace — between 15 and 30 mg/dL 1+ — between 30 and 100 mg/dL 2+ — between 100 and 300 mg/dL 3+ — between 300 and 1000 mg/dL 4+ — >1000 mg/dL Assessing Proteinuria Dipstick is semiquantitative and is strongly influenced by the urine volume A high urine flow rate will lower the urine protein concentration by dilution but will not affect total protein excretion. The urine dipstick is highly specific, but not very sensitive for mild proteinuriapositive only when protein excretion exceeds 300- 500 mg/day. Thus, the standard urine dipstick is an insensitive method to detect initial increases > 150 mg/day as occurs in patients with microalbuminuria False-positive urine dipstick results are common with many iodinated radiocontrast agents the urine should not be tested for protein with the standard dipstick for at least 24 hours after a contrast study. Assessing Proteinuria Sulfosalicylic acid test — In contrast to the urine dipstick, which primarily detects albumin, sulfosalicylic acid (SSA) detects all proteins in the urine Use of sulfosalicylic acid is primarily indicated in patients who present with acute renal failure, a benign urinalysis, and a negative or trace dipstick, a setting in which myeloma kidney should be excluded. A significantly positive sulfosalicylic acid test (SSA) in conjunction with a negative dipstick usually indicates the presence of nonalbumin proteins in the urine, most often immunoglobulin light chains. Assessing Proteinuria The sulfosalicylic acid (SSA) test is performed by mixing one part urine supernatant (eg, 2.5 mL) with three parts 3% sulfosalicylic acid, and grading the resultant turbidity 0 = no turbidity (0 mg/dL) trace = slight turbidity (1 to 10 mg/dL) 1+ = turbidity through which print can be read (15 to 30 mg/dL) 2+ = white cloud without precipitate through which heavy black lines on a white background can be seen (40 to 100 mg/dL) 3+ = white cloud with fine precipitate through which heavy black lines cannot be seen (150 to 350 mg/dL) 4+ = flocculent precipitate (>500 mg/dL Assessing Proteinuria Similar to the standard urine dipstick, the SSA test will also record false positive results in the presence of many of the commonly used iodinated radiocontrast agents. Protein excretion may be overestimated by as much as 1.5 to 2 g/L the urine should not be tested for protein for at least 24 hours aftercontrast Both the dipstick and sulfosalicylic acid test will detect urinary lysozyme, the production and excretion of which may be increased in patients with acute leukemia. Assessing Proteinuria Thus, lysozyme excretion should be measured in this setting, particularly if other signs of the nephrotic syndrome (such as edema and hyperlipidemia) are absent. The results with the dipstick and SSA serve as only a rough guide of the degree of protein excretion since urine concentration will affect the measurement. A dilute urine, for example, will underestimate the degree of proteinuria. Assessing Proteinuria Measurement of quantitative protein excretion — The quantity of protein excretion is important clinically for several reasons: Most patients with benign forms of isolated proteinuria excrete <1-2 g/day. The degree of proteinuria is prognostically important in patients with a primary glomerular dz, ie membranous nephropathy or FSGS Progression to renal failure most often occurs in patients with nephrotic range proteinuria, The degree of proteinuria is used to monitor the response to therapy, as with immunosuppressive drugs for primary glomerular diseases Assessing Proteinuria Most patients with persistent proteinuria should undergo a 24-hour urine measurement This can be cumbersome in ambulatory care settings specially if serial monitoring of protein excretion is used as a guide to the efficacy of therapy. An alternative method requires only a random urine specimen to estimate the degree of proteinuria This test calculates the total protein-to-creatinine ratio (mg/mg). This ratio correlates with daily protein excretion expressed in g per 1.73m2 of BSA Thus, a ratio of 4.9 represents a daily protein excretion of approximately 4.9 g per 1.73 m2 Assessing Proteinuria Calculating the spot urine protein-to-creatinine ratio is much easier for the patient and closely correlates with a wide range of levels of proteinuria It is particularly valuable for serial monitoring of protein excretion. Assessing Proteinuria Microalbuminuria — The urine dipstick is highly specific, becomes positive only when protein excretion exceeds 300 to 500 mg/day but not very sensitive for the detection of initial increases in protein excretion above the upper limit of normal of 150 mg/day. Thus, the standard urine dipstick is an insensitive method to detect microalbuminuria, which is the earliest clinical manifestation of diabetic nephropathy and, in patients without diabetes, is a marker of increased cardiovascular risk. Assessing Proteinuria The normal rate of albumin excretion is less than 30 mg/day; microalbuminuria = persistent albumin excretion between 30-300 mg/day Dipsticks are available that detect the urine albumin concentration in this range, but the preferred test for diagnosis and monitoring is the urine albumin-to-creatinine ratio, which is the similar in concept to the urine protein-to-creatinine ratio Case 22 yo with 1+ proteinuria on dipstick twice Protein to creatinine ratio showed 1 gm of proteinuria/1.73 m2 BSA 24 hour urine protein to creatinine ratio was the same Assessing Proteinuria Approach to proteinuria — History and exam looking for a systemic or renal disease, such as diabetes mellitus or autoimmune disease, that could account for the proteinuria In these cases, management of the proteinuria is part of the management of the underlying condition. A careful medical history may reveal a cause for proteinuria, such as diabetes mellitus or a prior history of renal disease. Poststreptococcal glomerulonephritis, for example, may be associated with persistent proteinuria years after recovery from the acute episode, a possible reflection of some irreversible glomerular damage Assessing Proteinuria Examination of the urine — The urine sediment should be examined for other signs of glomerular disease such as hematuria, red cell casts, Red cell casts, are virtually pathognomonic for glomerulonephritis. If the sediment is unremarkable, the differential diagnosis includes transient proteinuria, orthostatic proteinuria, and persistent proteinuria. The urine dipstick should be repeated on at least one other visit. If these subsequent tests are negative for protein, the likely diagnosis is transient proteinuria. Assessing Proteinuria Rule out transient proteinuria — Transient proteinuria is common, occurring in 4% of men and 7% of women on a single examination, with resolution on subsequent examinations in almost all patients A transient increase in protein excretion may be seen with fever and exercise, as well as with symptomatic urinary tract infection. With marked exercise, protein excretion can exceed 2 g/day and excretion of both albumin and LMW proteins is increased, suggesting both an increase in glomerular permeability and a reduction in proximal reabsorption These patients need no further evaluation and should be reassured that they do not have kidney disease. Assessing Proteinuria Rule out orthostatic proteinuria — A split urine collection should be obtained if the patient is younger than age 30 and has documented proteinuria on more than one occasion. This test detects orthostatic proteinuria, a relatively common finding in adolescents (occurring in 2- 5%), but uncommon in those over the age of 30 Orthostatic proteinuria is characterized by increased protein excretion in the upright position, but normal protein excretion when the patient is supine. ? neurohumoral activation and altered glomerular hemodynamics Total protein excretion is generally less than 1 g/day in orthostatic proteinuria, but may exceed 3 g/day in selected patients Assessing Proteinuria Orthostatic proteinuria is a benign condition requiring no further evaluation or specific therapy In many patients, the condition resolves over time. Split urines are collected : The first morning void is discarded. A 16-hour upright collection is obtained between 7 AM and 11 PM, with the patient performing normal activities and finishing the collection by voiding just before 11 PM. A separate overnight 8 hour collection is obtained between 11 PM and 7 AM. Assessing Proteinuria You can also do the protein-to-creatinine (Pr/Cr) ratio on a first morning spot urine specimen and on a specimen collected while upright. For this, the patient is instructed to void before going to bed and to remain recumbent until the first morning sample is obtained. A normal Pr/Cr ratio on the first morning void and dipstick-positive proteinuria with an elevated Pr/Cr ratio on a second specimen collected while the patient is upright indicates orthostatic proteinuria. The diagnosis of orthostatic proteinuria requires that protein excretion be normal when supine (less than 50 mg per 8 hours), not merely less than when in the upright position. Case- Follow up 22 yo patient with 1+ proteinuria on dipstick Urinary sediment negative Patient admitted to heavy exercise, intermittent use of steroids and significant intake of protein supplements Proteinuria persisted on several other exams Split urine samples revealed normal urine protein while supine Orthostatic proteinuria suspected although heavy exercise can also be contributing Patient warned regarding hyperfiltration proteinuria and advised against use of anabolic steroids Case 50 year old Asian gentleman with history of persistent proteinuria for past 7 years referred to UCI Renal Clinic. Creatinine stable, no hematuria, no change in degree of proteinuria (600mg/day) U/S normal, serologies all negative Assessing Proteinuria Persistent isolated proteinuria — thorough evaluation is warranted when isolated proteinuria persists. Usually reflects an underlying renal or systemic disorder. Underlying glomerular disease that may be primary (focal segmental glomerulosclerosis or membranous nephropathy) or secondary (diabetic nephropathy or hypertensive nephrosclerosis due to systemic hypertension). Renal function tests including BUN and creatinine should be obtained, as well as a quantitative measurement of urine protein excretion. In addition, the patients should undergo an ultrasound examination to rule out structural causes, such as reflux nephropathy or PCKD Assessing Proteinuria All patients with persistent proteinuria should be referred to a nephrologist for decisions regarding further management (eg, renal biopsy). A renal biopsy is performed if there is some sign of severe or progressive disease, such as nephrotic syndrome, increasing protein excretion, or an elevation in the plasma creatinine concentration. By contrast, biopsies are often not performed among patients with stable non-nephrotic proteinuria, providing renal function is stable and hematuria is not present, since knowledge of histology obtained by the biopsy is unlikely to alter therapy. Assessing Proteinuria The level of non-nephrotic proteinuria that should be evaluated by biopsy is not clear. ? perform a biopsy in patients with non-nephrotic proteinuria of 2 to 3 g/day but not for proteinuria that is less than one g/day If a patient with proteinuria greater than one g/day is reluctant to undergo biopsy, absolute indications include increasing proteinuria or plasma creatinine concentration, or a significant elevation in blood pressure over baseline values. PROGNOSIS — The prognosis of patients with glomerular proteinuria is related to the quantity of protein excreted. Non-nephrotic proteinuria (less than 3 g/day) is associated with a much lower risk of progressive chronic kidney disease than nephrotic range proteinuria. Assessing Proteinuria Most patients with persistent isolated proteinuria in the absence of decreased renal function or a systemic disease will have an indolent course. In one study, only 10% of such patients developed an elevation in plasma creatinine during a mean follow-up of six years. These observations indicate the need for persistent monitoring of patients with apparently benign, nonorthostatic, and persistent isolated proteinuria. Those with evidence of progressive disease (either increasing proteinuria or rising plasma creatinine concentration) may benefit from therapy with an angiotensin converting enzyme inhibitor or angiotensin II receptor blocker. Case Patient insisted on a biopsy Biopsy showed some foot processes effacement on EM otherwise negative Clinical and histopathology not consistent with MCD Biopsy nondiagnostic Glomerular disease Three different urinary and clinical patterns: Nephritic and nephroticfocal nephritic, diffuse nephritic (RPGN) Focal nephritic — Disorders resulting in a focal nephritic sediment are generally associated with inflammatory lesions in less than one-half of glomeruli on light microscopy. The urinalysis reveals red cells (which often have a dysmorphic appearance), occasionally red cell casts, and mild proteinuria (usually less than 1.5 g/day). The findings of more advanced disease are usually absent, such as heavy proteinuria, edema, hypertension, and renal insufficiency. Often present with asymptomatic hematuria and proteinuria discovered on routine examination or, occasionally, with episodes of gross hematuria. Glomerular disease Diffuse nephritic — The urinalysis in diffuse glomerulonephritis is similar to focal disease, but heavy proteinuria (which may be in the nephrotic range), edema, hypertension, and/or renal insufficiency may be observed. Diffuse glomerulonephritis affects most or all of the glomeruli. Glomerular disease Nephrotic — The nephrotic sediment is associated with heavy proteinuria and lipiduria, but few cells or casts. The term nephrotic syndrome refers to a distinct constellation of clinical and laboratory features of renal disease. It is specifically defined by the presence of heavy proteinuria (protein excretion greater than 3.5 g/24 hours), hypoalbuminemia (less than 3.0 g/dL), and peripheral edema. Hyperlipidemia, hypertension and thrombotic disease are also frequently observed. Glomerular disease Isolated heavy proteinuria without edema is an important clinical distinction heavy proteinuria in patients without edema or hypoalbuminemia is more likely to be due to secondary FSGS Edema secondary to decreased oncotic pressure as well as albumin in tubular lumen increasing activity of Na/H+ exchanger Therefore need salt restriction and diuretic for treatment Hypercholestrolemia correlates with hypoalbuminemia Factor V, VIII and fibrinogen increased while X, XI and ATIII are decreased, platelete aggregation increased Risk of infection with encapsulated bacteria increased due to loss of complement factor B and gamma globulin pneumococcal vaccine Nephrotic syndrome Heavy proteinuria and the nephrotic syndrome associated with variety of primary and systemic diseases. Minimal change disease is the predominant cause in children. In adults, approximately 30% have a systemic disease such as diabetes mellitus, amyloidosis, or systemic lupus erythematosus; the remaining cases are usually due to primary renal disorders such as minimal change disease, focal segmental glomerulosclerosis, and membranous nephropathy European study patients 15-65 years of age, membranous nephropathy (24%), minimal change disease (16%), lupus (14%), FSGS (12%), MPGN (7%), amyloidosis (6%), and IgA nephropathy (6%). Age greater than 65 years an increased incidence of amyloidosis (17%) and a decreased incidence of lupus (1%). Nephrotic syndrome A study of 233 renal biopsies performed 1995-1997 at the University of Chicago in adults (in the absence of an obvious underlying disease such as diabetes mellitus or lupus) found the major causes to be membranous nephropathy and FSGS (33% each), minimal change disease (15%), and amyloidosis (4% overall, but 10% in patients over age 44) The main change over time (compared to 1976-1979) was a marked increase in frequency of FSGS (35 versus 15%), particularly in black patients in whom it accounted for more than 50% of cases. Similar findings were noted in a report from Springfield, Massachusetts Over time, the relative frequency of membranous nephropathy fell from 38 to 15%, while the frequency of FSGS increased from 14 to 25% overall; this increase was primarily seen in black and Hispanic patients. Nephrotic syndrome Nephrotic syndrome can also develop in patients with postinfectious glomerulonephritis, MPGN, and IgA nephropathy. However, these individuals typically have a "nephritic" type of urinalysis with hematuria and cellular (including red cell) casts as a prominent feature. Nephrotic syndrone Case 9 yo boy presenting with edema and significant proteinuria (around 9 gms per day) No family history of kidney disease Biopsy is completely normal on light microscopy and IF is not very specific Nephrotic Syndrome Minimal change disease — Minimal change disease (also called nil disease or lipoid nephrosis) accounts for 90% of cases of the nephrotic syndrome in children under the age of 10 (peak age 2-3), and more than 50% of cases in older children, 10-15% in adults. It also may occur in adults as an idiopathic condition, in association with the use of NSAIDS, or as a paraneoplastic effect of malignancy, most often Hodgkin lymphoma. Also seen after treatment of melanoma with IFN beta ? Related to defect in cell mediated immunity Tcells from MCD patients release a vascular permeability factor Lymphokine that reduces negative charge of BM and is toxic to the podocytes Nephrotic syndrome The terms minimal change and nil disease reflect the observation that light microscopy in this disorder is either normal or reveals only mild mesangial cell proliferation. Immunofluorescence and light microscopy typically show no evidence of immune complex deposition. The characteristic histologic finding in minimal change disease is diffuse effacement of the epithelial cell foot processes on electron microscopy. IF with some IgM and C3 deposit, heavy IgM deposit associated with mesangial hypercellularity has a worse prognosis. Nephrotic syndrome Hematuria may be seen although it is not common Trearment usually involves steroids, relapses are common may be provoked by a URI Steroid resistant disease or frequent relapsers can be treated with cytoxan or CNI. Nephrotic syndrome 45 yo female with history of morbid obesity, hypertension admitted for CHF and diastolic dysfunction. On cardiac echo had infiltrative pattern. Urine with 2.5 grams of proteinuria, creatinine normal. Renal bx to rule out amyloidosis Nephrotic syndrome Focal segmental glomerulosclerosis — Focal segmental glomerulosclerosis (FSGS) accounts for 35% of all cases of nephrotic syndrome in the U.S. and over 50% of cases among blacks FSGS is characterized on light microscopy by the presence in some but not all glomeruli (hence the name focal) of segmental areas of mesangial collapse and sclerosis FSGS can present as an idiopathic syndrome (primary FSGS) or may be associated with HIV infection, reflux nephropathy, healed previous glomerular injury, an idiosyncratic reaction to NSAIDs, or morbid obesity, chronic transplant rejection, Heroin nephropathy. 50-60% of patients reach ESRD withing ten years although depending on type this is variable (HIVAN withing 2 years) Nephrotic syndrome There are three important diagnostic concerns in FSGS: Sampling error Distinguishing primary and secondary FSGS Identifying FSGS associated with collapsing glomerulopathy. Sampling error can easily lead to misclassification of a patient with FSGS as having minimal change disease. Clinical features that are seen in FSGS are hematuria, hypertension, and decreased renal function. There is, however, substantial overlap in these features. 30% only have proteinuria. In addition to careful review of the renal biopsy, steroid-resistance in a patient considered to have minimal change disease should raise suspicion about FSGS. Nephrotic syndrome Primary FSGS is an epithelial cell disorder that may be related etiologically to minimal change disease. Mutation in genes encoding podocyte proteins nephrin, podocin In addition, as noted above, FSGS can occur as a secondary response to nephron loss (as in reflux nephropathy) or previous glomerular injury. Differentiating primary and secondary FSGS has important therapeutic implications. The former may respond to immunosuppressive agents such as corticosteroids, while secondary disease is best treated with modalities aimed at lowering the intraglomerular pressure, such as angiotensin converting enzyme inhibitors. Nephrotic syndrome The distinction between primary and secondary FSGS can usually be made from the history (such as one of the disorders associated with secondary disease) and the rate of onset and degree of proteinuria. Patients with primary FSGS typically present with the acute onset of the nephrotic syndrome, whereas slowly increasing proteinuria and renal insufficiency over time are characteristic of the secondary disorders. The proteinuria in secondary FSGS is often nonnephrotic; even when protein excretion exceeds 3 to 4 g/day, both hypoalbuminemia and edema are unusual Nephrotic syndrome Collapsing FSGS is a histologic variant that is usually but not always associated with HIV infection. Two major features distinguish it : a tendency to collapse and sclerosis of the entire glomerular tuft, rather than segmental injury; and often severe tubular injury with proliferative microcyst formation and tubular degeneration These patients often have rapidly progressive renal failure and optimal therapy is uncertain. Nephrotic Syndrome Primary FSGS will need to be treated with 6-9 mos of steroids Steroid resistant cases are treated with MMF, CSA or cytoxan Factors associated with poor prognosis are persistent high grade proteinuria, extent of TIN, degree of glomerulosclerosis, higher creatinine, AA race, lack of response to steroids 30% recurrence rate in transplanted kidney rapid progression and higher degree proteinuria Nephrotic Syndrome Mesangial proliferative GN Microscopic hematuria or proteinuria, occasional nephrotic syndrome ACEI/ARB Steroids then CSA if no response IgM deposition and lack of response to steroid are a bad sign Nephrotic Syndrome 57 yo Caucasian male with history of hypertension and COPD presented with elevated creatinine 4-5 mg/dL for the past year or so Significant proteinuria at 6 gms/day Serologies are all negative Renal biopsy performed Membranous nephropathy Nephrotic syndrome Membranous nephropathy — Membranous nephropathy most common cause of primary nephrotic syndrome in Caucasians. It is characterized by basement membrane thickening with little or no cellular proliferation or infiltration, and the presence of electron dense deposits across the glomerular basement membrane Membranous nephropathy is most often idiopathic in adults and secondary in children, although it can be associated with hepatitis B antigenemia, autoimmune diseases, thyroiditis, carcinoma, and the use of certain drugs such as gold, penicillamine, captopril, and NSAIDs. In patients over age of 50 there is 20% association with malignancy therefore colon CA, lung CA, breast CA etc need to be ruled out Nephrotic Syndrome Patient with primary membranous 1/3 spontaneously go into remission (so follow for 6 months before treating), 1/3 remain stable (creat and proteinuria) and 1/3 progress Treat the 1/3 that progress with Ponticelli protocol (6 months of steroid/cytoxan alternating) Relapsers are treated with Rituxan and CNI Nephrotic Syndrome 46 yo hispanic male referred to LBVA for proteinruia, has significant edema and pleural effusions Albumin 2.2, urine with 10 gms protein per day Serologies negative Patient progressed to hemodialysis, also found to have CHF with EF 15% (nonischemic) Renal biopsy showed congo red positive stain Nephrotic syndrome Amyloidosis — amyloidosis accounts for 4 to 17% of cases of seemingly idiopathic nephrotic syndrome, with the increased infrequency observed among older individuals There are two major types of renal amyloidosis: AL or primary amyloid, which is a light chain dyscrasia in which fragments of monoclonal light chains form the amyloid fibrils; and AA or secondary amyloidosis, in which the acute phase reactant serum amyloid A forms the amyloid fibrils. AA amyloid is associated with a chronic inflammatory disease such as rheumatoid arthritis or osteomyelitis. The diagnosis is suspected by a history of a chronic inflammatory disease or, with primary disease, detection of a monoclonal paraprotein in the serum or urine. Nephrotic syndrome AL amyloid- cardiac disease, renal dysfunction and interstitial fibrosis are associated with a poor outcome Treatment consists of chemotherpay to reduce light chain production Melphelan and prednisone are the commonly used combination Best results in patients treated with melphelan and bone marrow transplantation AA amyloid- treat the underlying cause of inflammation. Colchicine in patients with FMF. Nephrotic syndrome AA amyloid- treat the underlying cause of inflammation. Colchicine in patients with FMF. Eprodisate is a member of a new class of compounds designed to interfere with interactions between amyloidogenic proteins and glycosaminoglycans and thereby inhibit polymerization of amyloid fibrils and deposition of the fibrils in tissues. Nephrotic syndrome randomized, double-blind, placebo-controlled trial AA amyloidosis and kidney involvement. Assigned 183 patients to receive eprodisate or placebo for 24 months. At 24 months, disease was worsened in 24 of 89 patients on eprodisate (27%) and 38 of 94 patients on placebo (40%, P=0.06); the hazard ratio for worsening disease with eprodisate was 0.58 (P=0.02). The mean rates of decline in creatinine clearance were 10.9 and 15.6 ml per minute per 1.73 m(2) of body-surface area per year in the eprodisate and the placebo groups, respectively (P=0.02). The drug had no significant effect on progression to end-stage renal disease (hazard ratio, 0.54; P=0.20) or risk of death (hazard ratio, 0.95; P=0.94). Eprodisate slows the decline of renal function in AA amyloidosis. N Engl J Med. 2007 Jun 7;356(23):2349-60 Nephrotic syndrome Monoclonal immunoglobulin deposition disease Deposition of light chain, heavy chains or both in a variety of organs including the kidney LCDD- immunoglobulin light chains deposit in the glomerulus and do not form fibrils Most deposits are derived from the constant region of kappa light chains Paraprotein detected in plasma and urine by immunofixation in 85% cases Nephrotic syndrome Most common presentation is nephrotic syndrome, HTN and decreased GFR Light microscopy with mesangial nodules, may have dense deposits IF positive for light chains in the glomerulus and basement membrane Subset of patients have cast nephropathy Overall prognosis is poor if renal failure present Some patients respond to melphalan and prednisone Heavy chain deposition disease has a similar presentation except has heavy chain deposition in glomerulus and basement membrane Nephrotic syndrome Lupus nephritis- six WHO classes Class V is membranous nephropathy and is associated with nephrotic syndrome Very similar to other forms of membranous with similar treatment and prognosis There is a class IV + class V variety which has the worst prognosis and poorly responds to treatment Nephrotic syndrome 45yo hispanic female with history of hypertension and diabetes for 10 years, both poorly controlled, ? history of DR, proteinuria and elevated creatinine Protein to creatinine ratio is 10 gms per day, also has significant edema, low albumin at 2 gm/L and severe hypertension Serologies are all negative Renal biopsy done Nephrotic syndrome Diabetic nephropathy Most common cause of nephrotic syndrome and ESRD in the U.S. Patients with type I diabetes and nephropathy have 50X increased risk of mortality Risk of nephropathy peaks after 20years of living with disease and then decreases Nodular glomeruosclerosis known as kimmelstiel-Wilson’s disease Time of initial diagnosis first decade marked by glomerular hyepertrophy and hyperfiltration glomerulopathy in the absence of clinical disease (microalbuminuria clinically evident disease with dipstick + proteinuria, HTN and decreased GFR ESRD Nephrotic syndrome Five stages of DN are well characterized in typeI They are similar in patients with type II except with one difficulty time of onset of type II is usually not as distinct In type I diabetes, presence of retinopathy correlates with nephropathy almost 100% of patients of the time In type II diabetes 2/3 of patients with retinopathy have nephropathy, therefore absence of retinopathy does not rule out nephropathy Presents with proteinuria, occasional hematuria will need full work up. However most common cause of microscopic hematuria is DN. Nephrotic syndrome Treatment is mainly aimed at controlling blood sugar and HgA1c less than 7 Controlling BP with goal BP <130/80 ACEI or ARB to decrease intraglomerular pressure Decreasing cardiovascular risk factors Aggressive BP and BS management is aimed at decreasing proteinuria and hence slowing down/cessation of progression of disease
![Detection of proteinuria[1]](http://s3.studylib.net/store/data/007549979_2-02bd2c299a632d6a55125f2f2a73449c-300x300.png)