Role of a neonatal nurse. - Mary Catherine Pilkington
advertisement

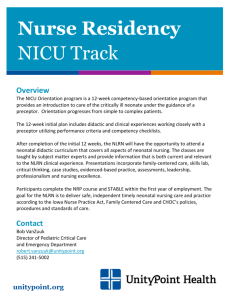
Running head: ROLE OF A NEONATAL NURSE 1 The Role of a Neonatal Nurse Mary Catherine Pilkington Introduction to Nursing (NUR 300) Professor Connelly September 28, 2012 ROLE OF A NEONATAL NURSE 2 A neonatal nurse works in the Neonatal Intensive Care Unit, called NICU for short. The NICU is just like an intensive care unit but it is designed with special equipment to care for very sick or premature babies. Not all hospitals have the level of nursery to be considered a NICU, so if a sick baby is born somewhere with just a regular, level one nursery, they could potentially be transported to a hospital more equipped to help them. The role of being a neonatal nurse is exciting and ever changing with every shift. Their job can be as simple as changing diapers and bathing babies or as complex as caring for critically ill or premature infants (Grimes, 2012). On the simpler, but still very important, side of NICU nursing, nurses help babies that are essentially healthy but just need to gain weight before they can be discharged to go home learn to eat. These babies would be considered feeder-grower babies (Grimes, 2012). A few specific duties of a neonatal nurse include “lots of IV therapy with maintenance of IV fluids, administration of medications based on an infant’s diagnosis, starting IVs and drawing blood, and assisting in procedures such as lumbar punctures, umbilical line and picc line insertions” (Grimes, 2012). There was a study conducted to determine the influence of work environments on actual outcomes in the NICU and they found that, “Professional work environment characteristics, such as nurse staffing and resource adequacy, nurse-physician relationships and nurse-management relationships, are related to better outcomes for nurses and higher nurse-related quality of care in NICUs” (Rochefort & Clarke, 2010 p.2220 para. 3). Just like most every nurse, neonatal nurses working with sick children serve as a patient and family advocate that teach and support parents as they deal with having a sick or premature infant that has to stay in the NICU, possibly even after the mother is discharged from the hospital after delivery (Grimes, 2012). As Karl and Keefer stated in their research, nurses help parents to establish a bond or relationship with their child that may otherwise be stressful or difficult ROLE OF A NEONATAL NURSE 3 because of their situation of being in an intensive care setting. Karl and Keefer said, “Nurses can use their knowledge of newborn behavior to facilitate connections that parents will use throughout their parenting lives…they can sensitive parents to what their infant is “saying” and help parents to accurately interpret these cues and respond appropriately” (Karl & Keefer, 2011 pp. 75-76 para. 5). So it is important that nurses working in the NICU are trained to know what certain behaviors of newborns could mean and how to teach their parents how to interpret and connect with their child that way. All nurses must learn to juggle their assignments and to decide what duty is most important and do those things first, and all of that just comes with experience and a good education (Grimes, 2012). Once a nurse has graduated from an accredited nursing program, if they desire to become a nurse specialized to work in the neonatal intensive care unit, they must have a little more education. There are always mandatory classes and continuing educational offerings specific to a neonatal nurses’ job, as are in most areas of nursing. Grimes stated that “to be a NICU nurse, one certification is Neonatal Resuscitation Program which is like CPR for babies. Of course, there is Basic Life Support that I have to keep up on as well as S.T.A.B.L.E. that my institution requires me to have” (Grimes, 2012). Of course the required continuing education will differ with each institution. It is acknowledged that there is a need for experienced and qualified nurses that can care for sick newborns (Redshaw & Harris, 1994). A study by Redshaw and Harris showed that there was a degree of overlap in qualifications of nurses working in the NICU. They concluded that “three-quarters of individual nurses had qualified as registered nurses and 45% as registered midwives. Fewer staff were registered sick childrens’ nurses, enrolled nurses or nursery nurses (Redshaw & Harris, 1994). Nurses that work with neonates need to meet many service demands. It has been studied and concluded that “Increasing the ROLE OF A NEONATAL NURSE 4 ration of nurse specialists in level 2 and 3 units increases the survival rates for very premature infants” (Pinfield, Pengelly, Rouse, & Passant, 2011). The easiest way to become a neonatal nurse would be to graduate from an accredited nursing school as a Registered Nurse, then complete any classes necessary to specialize in that area, and then proceed to take continuing education courses, as well as stay up to date on evidence based practice that will help the nurse grow into a more experienced and better qualified nurse. As with most professions and specialties, there are some organizations that are specific to neonatal nursing. There are also certain ethical guidelines and standards that a NICU nurse needs to live up to. They need to be an advocate for the patient, but they have to find a way to do it ethically and in a positive, helping manner. There are some specific attributes of a person who displays advocacy in a good way. A few of these attributes would be strong leadership skills, strong communication skills, sound knowledge base, and an ability to read signals and assess timing (Spence, 2007). One organization that is specific to the profession of neonatal nursing is the National Association of Neonatal Nurses. The mission statement of the Association is “NANN is the professional voice that shapes neonatal nursing through excellence in practice, education, research and professional development” ("National association of," 2010). Joining an organization like this one would be very beneficial and a nurse could learn a lot from it. Working with premature babies, one disease process that is very prevalent is Respiratory Distress Syndrome. This is usually in babies whose lungs have not fully developed so they do not have an adequate amount of surfactant so the lungs cannot inflate with air effectively (Lee, 2011). A nurse who is caring for a neonate with RDS has to have astute assessment skills that usually come from years of experience. Some specific skills they must do while taking care of ROLE OF A NEONATAL NURSE 5 the patient would be to “monitor chest rise, breath sounds, activity level, O2 stats, and blood gases” (Grimes, 2012). The earlier the baby is born, the more likely they are to develop this disease. It is important that if a baby does acquire this illness that they have few disturbances, and being handled gently, and that they maintain ideal body temperature in order for them to recover and become a strong, healthy child (Lee, 2011). It is also important that the nurses caring for the baby collaborate with the doctors and other health care professionals for the baby to be able to heal to their full potential. In conclusion, a neonatal nurse is one who works with critically ill or premature babies in the Neonatal Intensive Care Unit. Their job is one that is ever changing and can be very exciting and rewarding. They have the privilege to work with parents and to teach them how to communicate with their new baby as well as nurse the baby to good health. It is a very rewarding job when the patient is able to grow bigger and go home with their parents and live a full life. ROLE OF A NEONATAL NURSE 6 Grimes, G. (2012, September 02). Interview by M.C.Pilkington [Personal Interview]. Role of a neonatal nurse. Karl, D., & Keefer, C. (2011). Use of the behavioral observation of the newborn educational trainer for teaching newborn behavior. JOGNN: Journal Of Obstetric, Gynecologic & Neonatal Nursing, 40(1), 75-83. doi:10.1111/j.1552-6909.2010.01202.x. Lee, K. (2011, November 07). Medline Plus. Retrieved from http://www.nlm.nih.gov/medline Plus/ency/article/001563.htm. National association of neonatal nurses. (2010). Retrieved from http://www.nann.org/about/ content/our mission.html. Pinfield, J., Pengelly, T., Rouse, J., & Passant, M. (2011). Developing careers in neonatal nursing to meet service demands. Nursing Standard, 25(23), 35-40. Redshaw, M. & Harris, A. (1994). Training and education for nurses working in neonatal care. Journal of Advanced Nursing, 20(6), 1023-1029. doi: 10.1046/j.1365-2648.1994.2006102 3.x. Rochefort, C., & Clarke, S. (2010). Nurses’ work environments, care rationing, job outcomes, and quality of care on neonatal units. Journal Of Advanced Nursing, 66(10), 22132224. doi:10.1111/j.1365-2648.2010.05376.x. Spence, K. (2011). Ethical advocacy based on caring: A model for neonatal and paediatric nurses. Journal Of Paediatrics & Child Health, 47(9), 642-645. doi:10.1111/j.14401754.2011.02178.x. ROLE OF A NEONATAL NURSE 7