Overview on Understanding ICD 10-CM Codes
advertisement
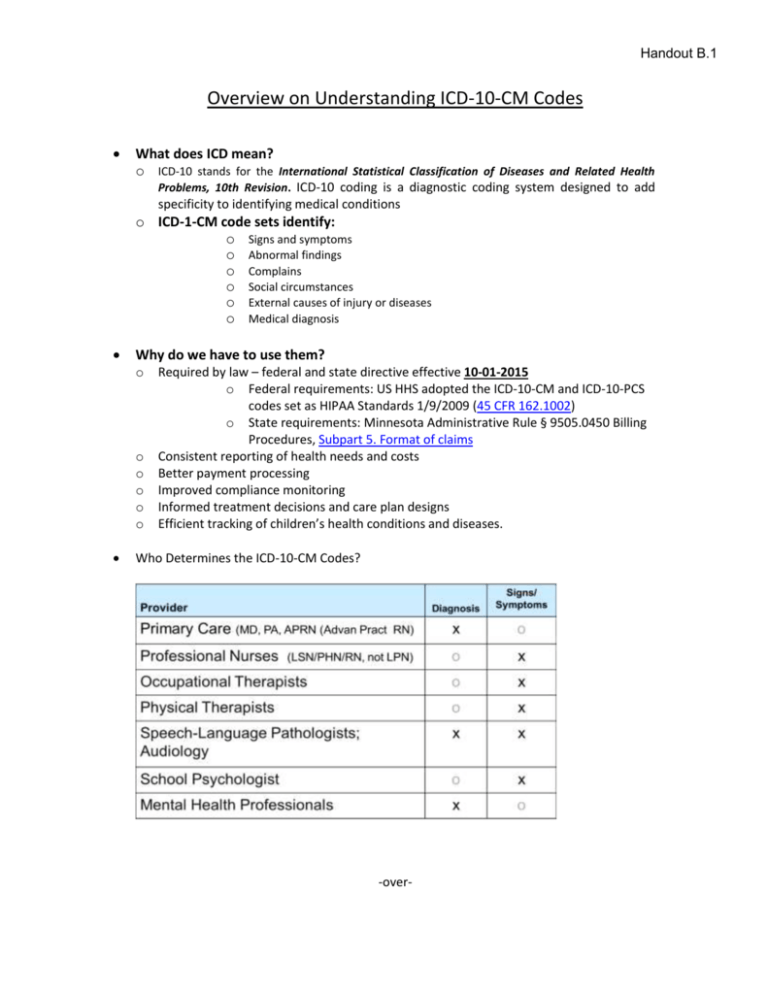
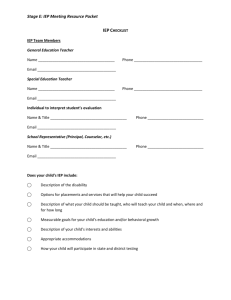
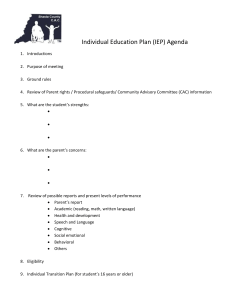
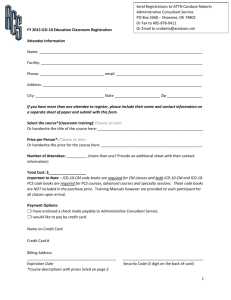
Handout B.1 Overview on Understanding ICD-10-CM Codes What does ICD mean? o ICD-10 stands for the International Statistical Classification of Diseases and Related Health Problems, 10th Revision. ICD-10 coding is a diagnostic coding system designed to add specificity to identifying medical conditions o ICD-1-CM code sets identify: o Signs and symptoms o Abnormal findings o Complains o Social circumstances o External causes of injury or diseases o Medical diagnosis Why do we have to use them? o o o o o o Required by law – federal and state directive effective 10-01-2015 o Federal requirements: US HHS adopted the ICD-10-CM and ICD-10-PCS codes set as HIPAA Standards 1/9/2009 (45 CFR 162.1002) o State requirements: Minnesota Administrative Rule § 9505.0450 Billing Procedures, Subpart 5. Format of claims Consistent reporting of health needs and costs Better payment processing Improved compliance monitoring Informed treatment decisions and care plan designs Efficient tracking of children’s health conditions and diseases. Who Determines the ICD-10-CM Codes? -over- Page 2 Overview of Understanding ICD-10-CM codes Handout B.1 Who determines the ICD-10-CM codes for the other health related services such as: o PCA services o Special transportation o Assistive Technology o Interpreter Services The IEP health related service professional directing, supervising or training selects the ICD-10-CM code(s). Many times it will be the same code used by the professional. EXAMPLE: The IEP Evaluation Report indicates: The child’s primary education disability is Autism Spectrum Disorder. The IEP team also determines the child has significant deficits in expressive language, communication skills and visual contact when speaking and services will be required of the SLP. Because the ICD-10-CM Code for Autism does not describe the SLP services, the SLP locates the code(s) that identifies the services or treatment provided, records the code in the file and uses the code(s) on the activity log (Claim) which is submitted for reimbursement to MDHS. In this example, the SLP may be treating the sign or symptom – not the disability or diagnosis. For IEP health related services to be billable: o IEP Evaluation report: Summarizes medical need States health related services are required during school day o IEP Record: Assessment and Plan describe: Health problem, condition or signs/symptoms: ICD-10-CM Plan of care/treatment plan, why and what services are necessary, when by whom and how often Training o Training will be provided via MDHS webinars MDHS hands-on training – September 24 – Ramada Inn, Marshall MN 3rd Party Billing coordinators to their school district employees Regional 3rd Party Billing Coordinator’s Meetings “Lead” SW/WC IEP Health care providers to SW/WC Service Cooperative employees and as “go to person” for school district.