CPR Checklist v12Apr2013
advertisement
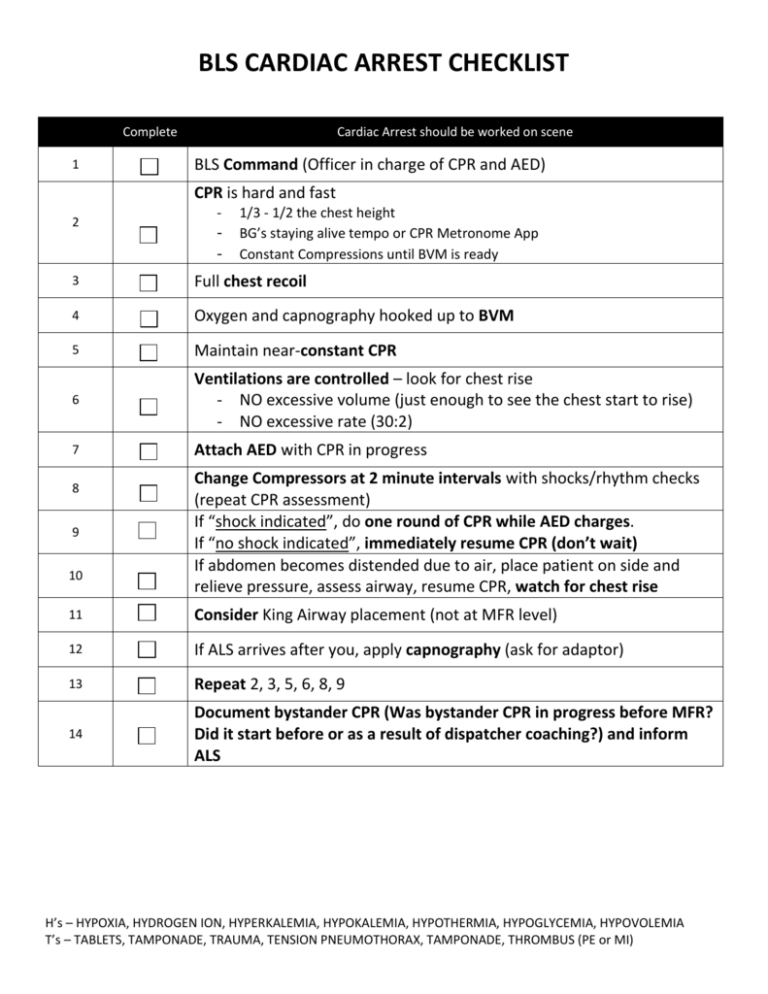
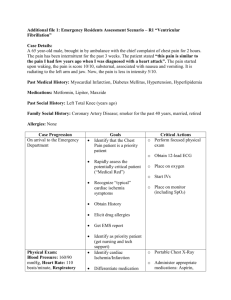
BLS CARDIAC ARREST CHECKLIST Complete 1 Cardiac Arrest should be worked on scene BLS Command (Officer in charge of CPR and AED) CPR is hard and fast 2 - - 1/3 - 1/2 the chest height BG’s staying alive tempo or CPR Metronome App Constant Compressions until BVM is ready 3 Full chest recoil 4 Oxygen and capnography hooked up to BVM 5 Maintain near-constant CPR 6 Ventilations are controlled – look for chest rise - NO excessive volume (just enough to see the chest start to rise) - NO excessive rate (30:2) 7 Attach AED with CPR in progress 8 9 10 Change Compressors at 2 minute intervals with shocks/rhythm checks (repeat CPR assessment) If “shock indicated”, do one round of CPR while AED charges. If “no shock indicated”, immediately resume CPR (don’t wait) If abdomen becomes distended due to air, place patient on side and relieve pressure, assess airway, resume CPR, watch for chest rise 11 Consider King Airway placement (not at MFR level) 12 If ALS arrives after you, apply capnography (ask for adaptor) 13 Repeat 2, 3, 5, 6, 8, 9 14 Document bystander CPR (Was bystander CPR in progress before MFR? Did it start before or as a result of dispatcher coaching?) and inform ALS H’s – HYPOXIA, HYDROGEN ION, HYPERKALEMIA, HYPOKALEMIA, HYPOTHERMIA, HYPOGLYCEMIA, HYPOVOLEMIA T’s – TABLETS, TAMPONADE, TRAUMA, TENSION PNEUMOTHORAX, TAMPONADE, THROMBUS (PE or MI) ALS CARDIAC ARREST CHECKLIST Complete Cardiac Arrest should be worked on scene 1 BLS Command (Officer in charge of CPR and AED) 2 Get report of care and downtime while continuing with list Verify CPR is hard and fast 3 4 5 6 7 8 9 10 11 12 13 14 15 16 - 1/3 - 1/2 the chest height BG’s staying alive tempo or CPR Metronome App Constant Compressions until BVM is ready Verify Full chest recoil Verify Oxygen and capnography hooked up to BVM Maintain near-constant CPR Ventilations are controlled – look for chest rise - NO excessive volume - NO excessive rate (30:2) If AED is attached: allow the AED to complete the 2 minute cycle and shock if needed before transitioning to the EKG monitor If NO AED attached: attach pads for monitor during compressions - If only ALS on scene, push analyze for AED mode - IF BLS is doing CPR, use lead or paddles setting for manual If there is adequate chest rise with ventilation and no obvious risk of airway loss (burns or trauma to the airway), DO NOT PLACE AN ADVANCED AIRWAY YET. Continue with basic airway-Consider King Tube If abdomen becomes distended due to air, place patient on side and relieve pressure, assess airway, resume CPR, watch for chest rise Change Compressors at 2 minute intervals with shocks/rhythm checks (repeat CPR assessment) – Eliminate peri-shock pauses (see BLS). Prepare IV – establish access If the patient is in a shockable rhythm or a narrow complex PEA, establish IO access in the proximal humerus. If the patient is in a wide complex PEA or asystole, look for peripheral access sites above the level of the diaphragm. Administer Epinephrine (adults 1mg – peds 0.01mg/kg) Evaluate/Correct H’s and T’s Ask about and document bystander CPR (Was bystander CPR in progress before MFR? Did it start before or as a result of dispatcher coaching?) H’s – HYPOXIA, HYDROGEN ION, HYPERKALEMIA, HYPOKALEMIA, HYPOTHERMIA, HYPOGLYCEMIA, HYPOVOLEMIA T’s – TABLETS, TAMPONADE, TRAUMA, TENSION PNEUMOTHORAX, TAMPONADE, THROMBUS (PE or MI)