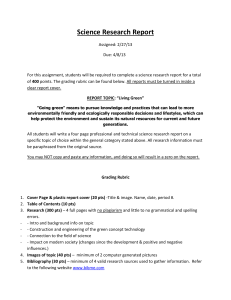
Table 2 Review of the literature for key questions 3 and 4 1st author
advertisement

Table 2 Review of the literature for key questions 3 and 4 1st author / year / Intention-to- Control for Inclusion criteria Surgical intervention Comparison group Randomization FU Participants Precise description of Symptom Quantification of Co– (baseline) symptoms(baseline) duration SL treatment Target variables Relevant results Indication of study type / Period treat analysis bias / con- performed? founding (++, sources / +, –) conflicts of LoE Our conclusion 2b – Instrumented fusion + Authors’ conclusion funding interest Key question 3: Is instrumented fusion with decompression more successful in relation to pain and function than decompression alone in adult patients with degenerative SL and spinal canal stenosis? Bridwell et al. / – No – 1993 / 2b cohort – Surgery for degen. SL with – Group I: decomp., n = 9 NC due to SPS – Group II: decomp. – Intended to be – Min. Group I: 7 fe- – NC with leg pain and + posterolateral randomized 2 y., male, 2 male inability to walk distances study / 1985–1990 fusion (autologous [30] iliac bone graft) without instr., n = 10 – Group III: decomp.+ posterolateral fusion – In fact, not all pts – No data – Unclear – No data, – Ability to walk – Ability to walk distances except: distances significantly: average 3 y 2 mo randomized Group II: 6 Group 1: – Progression of Group I: 3/9 pts improved; 3/9 female, 4 male no ortho- SL pts unchanged; 3/9 pts reduced Yes “For this specific class of pts, pedicle fixation and fusion is indicated along with decomp.”; decomp. better than de- “Significantly more SL progression in groups I comp alone and II than in group III” – Methodological short- sis – Preop. pathologic Group III: 20 motion led to inclu- female, 4 male comings (no clear Group II: 3/10 pts improved; sion in group III Mean age: Group II + 5/10 pts unchanged; 2/10 pts III: ortho- reduced randomization, different baseline data, small cohorts) sis (autologous iliac Group III: 20/24 pts improved; bone graft) + pedicle Group I: 72 yr screw instr., n = 24 4 mo – Poor study for answering 4/24 pts unchanged key question – Increase in SL: Group II: 65 y 7 mo Group I: 4/9 pts Group III: 64 y Group II: 7/10 pts 2 mo Group III: 1/24 pts – Of 12 pts whose SL progressed, one felt that surgery was of benefit – Of the other 31 pts, 28 felt that surgery improved their ability to walk distances Ghogawala et al. / – No – – Surgery for degen. SL1° + – Decomp. alone, n = 20 – Decomp.+ poster- 2004 / 2b cohort symptomatic lumbar SPS olateral instr. fusion study / 2000–2002 without gross instability with pedicle screws, [32] iliac crest autograft, – No previous spine surgery n = 14 – No 1y – Mean age 68.8 y – Type of surgery chosen by surgeon at his discretion at index level – No data – No data – SL slip in mm – No data – ODI, SF-36 – Decomp. alone vs decomp. + Yes “Fusion was associated with greater functional 2b improvement” fusion at 1-y FU: – Instrumented fusion + decomp. better than de- – No differentiation leg vs – Preoperative – Female 68% back pain extent of SL: ODI: 27.4 (P=0.003) vs 14 – “No significant – Symptomatic lumbar 8.5 mm (P<0.001) – Small cohorts intergroup dif- SPS SF-36 PCS: 37.4 (P=0.005) vs – Methodological short- 45.7 (P<0.001) comings Decomp. + fusion improved – Type of surgery at the better than decomp. alone in surgeon’s discretion ferences in the preoperative variables” comp. alone – Decomp. alone vs decomp. + fusion: ODI: 41.0 vs 41.5 ODI (P=0.02) and SF-36 PCS (P=0.003) SF-36 PCS: 30.9 vs 29.8 – Older age: strong independent predictor of poorer outcomes in both groups (multivariate analyses; decomp. alone: ODI P=0.028; SF-36 PCS P=0.008; decomp. + fusion: ODI not sign.; SF-36 PCS P=0.05) Park et al. / 2012 / case–control study 3b / 2005–2007 [33] – No – – Degen. single level SL 1° – Surgical candidates – Radiculopathy – Unilateral laminectomy – Decomp. + instr. and bilateral decomp., fusion with pedicle n = 20 screws, local bone graft and cage, n = 25 – unresponsive to cons. treatment > 3 mo – No – Retrospective Median – Decomp. only 63 mo vs decomp. + instr. fusion: study – Radicular pain – Decomp. only vs decomp. + instr. Fusion: Age: 67.7 vs 61.9 y 3 mo – Yes Female: 75% vs 8.0±0.87 ODI: 29.8±4.40 vs 24.6±5.38 SF-36 PCS: 29.2±3.67 vs 26.1±5.33 SF-36 MCS: 28.0±3.37 vs – NRS leg, NRS – Decomp. only vs decomp. + back, ODI, SF-36, instr. fusion at FU: Yes “Unilateral laminectomy and bilateral decomp. is the recommendable procedure for the treatment 3b – Methodologically poor – Fusion vs decomp. + pts: ortho- NRS back pain: 1.2±2.20 vs instr. fusion: sis 3 mo 2.4±1.88 (diff. between groups especially for NRS back P=0.001) pain NRS leg pain: 2.4±2.53 vs – Key question cannot be 2.5±1.80 (diff. between groups answered Odom’s criteria of pts with grade I deg. SL who have mainly radicular pain” – Retrospective study with different baseline data, Preop. slip 14.1% vs 14.7% NRS leg pain: 7.8±0.91 vs – No data – Decomp. only NRS back pain: 2.8±3.10 vs 6.6±2.47 88% – Min. P=0.99) ODI: 15.45±7.06 vs 11.0±7.09 (diff. between groups P=0.96) SF-36 PCS: 47.2±9.42 vs 46.3±7.41 (diff. between groups P=0.26) 29.3±3.84 SF-36 MCS: 46.7±8.54 vs 44.5±6.63 (diff. between groups P=0.25) Excellent 3 vs 4; Good 10 vs 10; Fair 2 vs 5; Poor 5 vs 6 (diff. between groups P=0.50) – Surgery of 1 or 2 levels for – Decomp. alone, n = 655 – Decomp. + fusion, tional Swedish lumbar SPS with degen. SL (including only pts with n = 651 (including Register for Spine (n = 1306) and without de- degen. SL) only pts with deg. Surgery) / 2013 / gen. SL Försth et al. (Na- – No – case–control study SL) – Age > 50 y 3 b / 1998–2008 – No 2y – Retrospective – Mean age 69 y – Female73% – All pts with degen. SL: – No data – Yes – No data – SL defined as VAS back pain: 58±26 ≥ 3 mm slip on register study VAS leg pain: 62±25 – No differentiation – ODI, EQ5D, – No sign. difference in patient VAS back pain, satisfaction between the 2 decomp. was not associated with an improved VAS leg pain groups outcome” 3b – Retrospective registry study – Methodological shortcomings (no baseline data EQ5D: 0.36±0.31 non–instr. fusions “In this large cohort the addition of fusion to radiographs on complaints differentiat- – Decomp. alone vs decomp. + between instr. and [31] Yes ODI: 45±15 fusion at FU: – No differentiation be- VAS back pain: 35 (95% CI 32- tween pts with degen. SL 37) vs 32 (95% CI 30-34) receiving decomp. only vs (P=0.12) ed for both groups) – No data on type of fusion (instr. vs. non–instr.) – Key question cannot be answered; at best, trend can decomp. + fusion VAS leg pain: 35 (95% CI 32- be seen that fusion pts do 37) vs 32 (95% CI 30-35) not perform better at FU, (P=0.17) but without having baseline data EQ5D: 0.63 (95% CI 0.61-0.66) vs 0.62 (95% CI 0.59-0.64) – Most likely, baseline data (P=0.34) for both groups were not similar ODI: 27 (95% CI 26-29) vs 27 (95% CI 26-29) (P=0.93) Key question 4: Is instrumented fusion with reduction more successful in relation to pain and function than instrumented fusion without reduction in adult patients with isthmic or degenerative SL? – Dysplastic low- or high- – Posterolateral fusion with – Same as groups A – “Were random- RCT 1b / no data grade SL with pars articularis local autologous grafts + and B + reduction, ized” [34] defect + facet joint dysplasia allografts, decomp., sagittal n = 20 Benli et al./ 2006 / – Yes + – Pain unresponsive to cons. plane correction, instr. with pedicle screws, n = 20 treatment – Presence of neurological – Group A: low dysplastic, n = 10 – Group A vs B – No details on relation of vs C vs D: back to leg pain – No details on Age: 29.2 vs randomization 34.9 vs 32.6 vs dysplastic, n = 10 deficits or NC – Displacement > 25% + – Group C: low 37.9 mo 32.4 y – Group D: high Female: 2 vs 2 dysplastic, n = 10 vs 2 vs 2 – No data – Slippage – Slippage at FU: No “Anterior slippage reduction did not have any 1b additional favorable effect on clinical results” change; P>0.05) Group A: 6.7 – Slippage before Group B: 29.5% (no sign. surgery: change; P>0.05) Group A: Group C: 5.5% (83.4±32.6% 30.5±5.5% correction; P<0.01) Group B: Group D: 5.3% (87.1±16.1% 30.0±5.8% correction; P<0.01) Group C: – JOA at FU (diff. between 32.3±8.1% groups P>0.05): Group D: Group A: 17.1 (P<0.05) study (deficiency: type of randomization not specified, small groups) – Conclusion: reduction Group B: 6.8 Group C: 6.9 Groups A and C – All pts had NC in addi- had similar tion to neurogenic pain baseline data – Methodologically well designed and performed Group A: 30.5% (no sign. erding 2° Group D: 6.7 – No previous spinal surgery – JOA, SRS22 – JOA: vertebral instability – No trauma – No data – All pts: Mey- – Group B: high dysplastic, n = 10 – Yes not necessary Groups B and D – No degen. changes had similar 40.6±5.9% baseline data Group B: 17.2 (P<0.05) Group C: 16.6 (P<0.05) Group D: 16.1 (P<0.05) – Improvements in SRS22 were independent of surgical technique and type of SL (diff. between groups P>0.05) Lian et al. / 2013 – 82 pts en- Spine J / RCT 1b / rolled, 9 pts 2006–2009 [37] lost, 73 pts finally analyzed + – 1 level degen. SL + SPS – PLIF + complete bilateral – Same as group A requiring surgery removal of the laminae and without reduction – Age > 70 y decomp. of nerve roots + pedicle screw instr. with 2 – No previous lumbar spine PEEK cages (filled with surgery bone from the posterior elements) + reduction simultaneous surgery – Randomized by – Group A, n = 36 – Min. – Group A vs – Severe disabling LBP + 2 y; group B: lower extremity pain + NC, refractory to conserv. serial number ac- – Mean Mean age 74.3 y cording to the 33.2 mo vs 73.8 y quence of Female 61% vs. 62% L3/4: n = 2 vs likelihood of developing n = 32 post–decomp. instability L5/S1: n = 3 vs compression secondary to – Group A vs group B: – Yes – No data – VAS, ODI, JOA – Group A vs group B: –Standing radio- – Radiographic Mean operating time: graphs data (vertebral 126.5±23.3 min. vs 118.6±17.5 slip, focal lordosis, min. (P=0.107) disc height) Yes “In conclusion, for aged pts with degen. lumbar designed and performed RCT to reduce the slipped vertebra and restore sagittal balance. PLIF with pedicle screw fixation, with or without reduction, provides good outcomes in Meyerding grade 436.4±137.1 mL vs the surgical treatment of aged pts with degen. 450.5±147.3 mL (P=0.672) SL. Better radiological outcomes do not necessarily indicate better clinical outcomes” – Group A vs 60.8±22.1 group B: JOA: 13.1±3.3 vs 1° slip: n = 29 vs 12.7±3.7 n = 30 n=2 VAS at FU: 1.3±0.9 (P<0.001) vs 1.1±0.8 (P<0.001) (diff. between groups P=0.322) ODI at FU: 22.4±11.7 (P<0.001) vs 23.9±11.3 2° slip: n = 7 vs (P<0.001) (diff. between groups n=7 P=0.578) – Methodologically well screws seems to be an effective surgical method Mean blood loss: ODI: 62.2±20.8 vs 1b SL, a drawing-back technique with pedicle nique and VAS: 4.2±1.9 vs 4.0±1.7 n=3 L4/5: n = 31 vs decomp. to relieve nerve root ≥ 3 mo Taillard tech- – Preoperative instability or – Requirement of foraminal treatment for ≥ 3 mo consecutive se- hospitalization – No degen. disease in adjacent segments requiring – Group B, n = 37 – Yes – Reposition does not provide better clinical results compared to in situ fusion in degen. SL foraminal SPS Average preop. JOA at FU: 22.1±3.6 (P<0.001) slip: 18.3±5.8% vs 23.2±4.3 (P<0.001) (diff. vs 19.6±7.1% between groups P>0.05) Slip at FU: 3.1±4.4% vs 14.3±4.4% (diff. between groups P<0.001) No radiographic sign of nonunion at FU Surgical complications: 22.2% vs 21.6% Lian et al. / 2013 – 94 pts en- Eur Spine J / RCT rolled, 6 pts 1b / 2006–2008 lost, 88 pts [36] finally ana- + – 1 level isthmic SL without – PLIF + complete bilateral – Same as group 1 – Randomized by – Min. – Group 1 vs – LBP, lower extremity degen. removal of the laminae and without reduction serial number ac- 2 y; group 2: pain or NC that were cording to the – Mean consecutive se- FU: 32.5 quence of mo decomp. of nerve roots + disease in adjacent level lyzed pedicle screw instr. with 2 – No previous lumbar spine PEEK cages (filled with surgery bone taken from the poste- – Group 2, n = 43 hospitalization ≥ 3 mo refractory to conserv. Mean age 45.5 y treatment for ≥ 3 mo – Yes – No data – Radiographic Mean operating time: 119 min. graphs data (vertebral (range 100-160 min.) vs 125 slip, focal lordosis, min. (range 100-180 min.) Taillard tech- Female 62% vs rior elements) + reduction 63% – Group 1, n = 45 L4/5: n = 32 vs Meyerding grade 44.1±18.9 n = 29 group 2: 1b – Methodologically well degen. disease in adjacent level, single segment designed and performed of PLIF with pedicle screw fixation is an effec- RCT tive and safe surgical procedure regardless of – Repositioning does not whether reduction has been conducted or not. Mean blood loss: 475 mL Better radiological outcome does not mean better (range 180-1030 mL) vs clinical outcome” provide better clinical results compared to in situ fusion in isthmic SL VAS at FU: 11.7±7.6 vs 51.1±13.8 11.9±7.8 (diff. between groups L5/S1: n = 13 vs n = 14 “In conclusion, for the adult isthmic SL without 490 mL (range 250-840) – Group 1 vs ODI: 50.2±16.1 vs Yes disc height) nique and VAS: 42.5±17.5 vs – Group 1 vs group 2: – Standing radio- vs. 44.9 y – Group 1 vs group 2: – VAS, ODI, JOA 1° slip: n = 15 vs JOA: 15.4±3.0 vs P>0.05) n = 16 15.3±3.0 ODI at FU: 16.2±10.2 vs 2° slip: n = 25 vs 15.9±9.6 (diff. between groups n = 23 P>0.05) 3° slip: n = 5 vs JOA at FU: 24.1±2.6 vs n=4 23.9±2.8 (diff. between groups P>0.05) Average preop. slip: 28.1±11.4% Slip at FU: 6.3±6.0% vs vs 27.9±12.0% 17.7±9.3% (diff. between groups P<0.001) No radiographic sign of nonunion at FU Surgical complications: 11% vs 9% – Pts from 2 databases of 2 – 1-level posterolateral – No separate control 2013 / 2c study / no ongoing prospective studies lumbar fusion + laminec- group data [35] on the biological process of tomy + medial facetectomy fusion in instr. posterolateral + pedicle screw instr., lumbar 1-level fusion in pts n = 72 Hagenmaier et al. / – No + with low-grade degen. or isthmic SL (Meyerding I° + – No 1y Mean age 51 y VAS leg pain: 69.0 (range 2.0-98.0) – No data Meyerding grade I: n = 36 – VAS leg pain, VAS leg pain at FU: 5.5 (range ODI 0.0-93.0) (P<0.001) Female 54% – Correlation analysis of effect of amount of reduction Isthmic SL 71% Degen. SL 29% on clinical outcome L3/4 9% II°) Meyerding grade – Radiographic ODI at FU: 11.1% (range 0.0- 73.3%) II: n = 36 data (vertebral 77.8%) (P<0.001) slip, foraminal Listhesis preop: 10.6±4.3 mm (25.2±10.3%) – Complete radiographic + L5/S1 49% diameter, disc height, fusion status) Slips at FU: 8.1±5.0 mm (P<0.001) Foraminal diameter at FU: ter preop.: 19.0±4.3 mm (P<0.001) 21.1±3.3 mm Anterior disc height at FU: 7.6±3.8 mm (P>0.05) 18.7 mm) Posterior disc height at FU: 4.3 mm (range 0-10.9 mm) (P>0.05) Posterior disc height preop.: 4.8±2.5 mm radiographic reduction of the slipped vertebra. no evidence that it positively affects clinical outcome” 2c – Methodologically limited design – Not a controlled trial – Simple 1-cohort study with data from 2 databases – Only little data on pts included – No correlation between slip reduction and clinical outcome height preop.: 7.7 mm (range 9- “Clinical outcome was not related to the obtained (17.4%; range 0-59.7%) Foraminal diame- Anterior disc Yes Although reduction remains appealing, there is ODI: 44.4% (range 8.9- L4/5 42% clinical FU – No data Fusion rate on CT at FU: 64% “No correlation could be established between slip reduction and clinical outcome” (Pearson’s correlation VAS -0.204; ODI 0.066) Fusion vs nonfusion: no sign. clinical diff. Isthmic vs degen. SL: higher preop. VAS for degen. SL (P<0.01), at FU no sign. clinical diff. in improvements in VAS and ODI Abbreviations: +/–, with or without; CD, Cotrel–Dubousset; CI, confidence interval; conserv., conservative; CT, computed tomography; decomp., decompression; degen., degenerative; diff., difference; DRI, Disability Rating Index; DS, degenerative spondylolisthesis; EQ5D, EuroQoL 5D; FU, follow-up; instr., instrumentation/instrumented; JOA, Japanese Orthopedic Association (score); LBP, low back pain; LBPBI, Low Back Pain Bothersomeness Index; LoE, level of evidence; LPBI, Leg Pain Bothersomeness Index; MCS, mental component summary (score); min., minute(s) or minimum; mo, month(s); NC, neurogenic claudication; NRS, Numeric Rating Scale; NSAID, nonsteroidal anti-inflammatory drug; ODI, Oswestry Disability Index; PCS, physical component summary (score); PEEK, polyetheretherketone; PLF, posterolateral lumbar fusion; PLIF, posterior lumbar interbody fusion; pts, patients; RCT, randomized controlled trial; SBI, Stenosis Bothersomeness Index; SF-36, Short Form-36 (questionnaire); sign., significant; SL, spondylolisthesis; SPORT, Spine Patient Outcome Research Trial; SPS, spinal stenosis; TE, treatment effect; VAS, visual analogue score; vs, versus; wk, week; y, year(s); ZCQ, Zurich Claudication Questionnaire.