Designing a Hybrid Simulation
advertisement
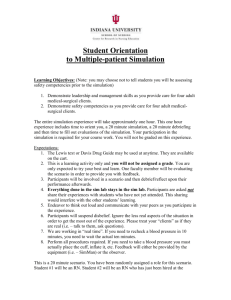
Designing a Hybrid Simulation Ralitsa Akins, MD, PhD ATACS Center, Paul L. Foster SOM, TTUHSC, El Paso, Texas In healthcare teaching and training exercises, the simultaneous utilization of both human and mechanical simulators in the same scenario is known as “hybrid simulation.” Advantages of hybrid simulation: Potential to increase the immersive nature of the experience, taking the best of both worlds: standardized patient role play and use of partial task simulators and/or high-fidelity manikins Opportunity for optimal use of limited number of simulators in large classes of students, increasing return on investment Ability to display heart and lung sounds, and vital signs that might not be available in healthy standardized patients Cautions of hybrid simulation: Depending on the fidelity and technical complexity of the manikins, cost of manikins might be restrictive The human and mechanical portions of the scenario must be well integrated to maintain the ability of the learner to suspend disbelief The human and mechanical locations of the scenario must be in relative proximity to avoid time lost Many scenarios in healthcare training are well-suited for hybrid simulation: Practically, every scenario involving the history-taking of a person with abnormal vital signs or bodily sounds is perfect for hybridization with examination of a manikin module. Scenarios involving healthy or sick patients with necessity of pelvic or rectal examination are great substitute for using gynecological or prostate human teaching assistants. Scenarios involving rapid decline of patient’s condition and emergency/anesthesia treatment would benefit from starting the encounter with a standardized human patient and moving to working with a manikin for intubation, placement of chest tube or completing a code. Scenarios involving death and dying are excellent examples of including both the opportunity to manage a terminal patient (manikin) and counsel the family (human standardized patients). Scenarios involving pediatric/neonatology patient (manikin) and working with the parent(s) (human standardized patients) are appropriate substitutes for pediatric human patient simulators. Example of Anaphylaxis Hybrid Scenario Disclaimer: This scenario was initially developed by Hoi Ho, MD for first year medical students at the Paul L. Foster SOM, session on immune hyper-reactivity. Objectives: 1. Recognize signs and symptoms of anaphylactic reaction 2. Apply first aid to a patient with anaphylaxis 3. Monitor vital signs and progress of a patient with anaphylaxis Scenario Title: Anaphylactic reaction to latex Necessary preparation: Recruit a student from the class to participate, to increase the immersive experience Train a staff member or a standardized patient for the role of the technician Have a wheelchair readily available Have the session faculty or a staff member clearly take responsibility for “calling 911” to prevent calls from classmates High-fidelity simulator (iSTAN or other) Other equipment needed: bag-valve mask, BP apparatus, thermometer, pulse oximeter, suction pump, large monitor for vital signs, syringe(s) with labeled medication(s), telephone Case description: A 26-year-old male first year medical student suddenly develops acute respiratory distress with stridor and wheezing during a medical skills session. Prior to the event, the student is in his usual status of health. A service technician wearing latex gloves and cleaning the white board in the beginning of the session, accidentally falls and grips the student’s forearm (student is in short sleeve shirt). Five minutes after this incident, the student starts feeling itchy around the forearm; the itch spreads to the face and whole body, and sneezing starts. Few minutes later, the student develops difficulty breathing, with rapid and shallow breaths, starts having stridor and tries to loosen his shirt around the neck. Student keeps pointing to the neck (laryngeal spasm and edema). Student is quickly moved to the clinical simulation room, where the high fidelity simulator is located, and the scenario continues managing a simulator with anaphylaxis. Manikin settings: BP 80/56 mm Hg; RR 30/min; HR 130/min; T 96.2F; Pulse Oxi 92%. It is very convenient to use the anaphylaxis stages pre-set on the manikin. Optional: Patient safety issue with use of look-alike/sound-alike medication (e.g. a student on the team calls Pharmacy for epinephrine; another medication is brought, and the faculty needs to prevent the application of the wrong medication by asking the student to verify patient and medication). NOTE: The play of this scenario yielded high-believability among the student group, with strong emotional response (a colleague student was involved), and excellent opportunities for immersive hybrid simulation use in teaching.