Patient Centered Care
advertisement
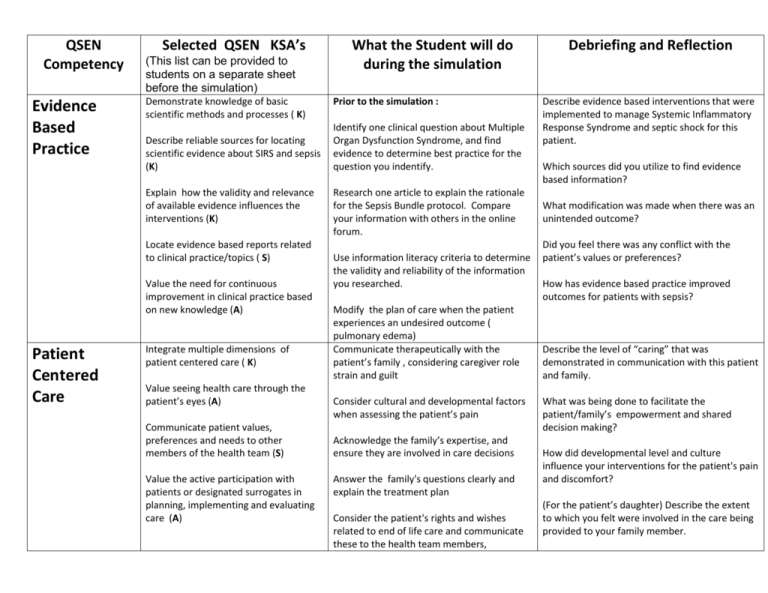
QSEN Competency Evidence Based Practice Selected QSEN KSA’s (This list can be provided to students on a separate sheet before the simulation) Demonstrate knowledge of basic scientific methods and processes ( K) Describe reliable sources for locating scientific evidence about SIRS and sepsis (K) Explain how the validity and relevance of available evidence influences the interventions (K) Locate evidence based reports related to clinical practice/topics ( S) Value the need for continuous improvement in clinical practice based on new knowledge (A) Patient Centered Care Integrate multiple dimensions of patient centered care ( K) Value seeing health care through the patient’s eyes (A) Communicate patient values, preferences and needs to other members of the health team (S) Value the active participation with patients or designated surrogates in planning, implementing and evaluating care (A) What the Student will do during the simulation Prior to the simulation : Identify one clinical question about Multiple Organ Dysfunction Syndrome, and find evidence to determine best practice for the question you indentify. Research one article to explain the rationale for the Sepsis Bundle protocol. Compare your information with others in the online forum. Use information literacy criteria to determine the validity and reliability of the information you researched. Modify the plan of care when the patient experiences an undesired outcome ( pulmonary edema) Communicate therapeutically with the patient’s family , considering caregiver role strain and guilt Consider cultural and developmental factors when assessing the patient’s pain Acknowledge the family’s expertise, and ensure they are involved in care decisions Answer the family's questions clearly and explain the treatment plan Consider the patient's rights and wishes related to end of life care and communicate these to the health team members, Debriefing and Reflection Describe evidence based interventions that were implemented to manage Systemic Inflammatory Response Syndrome and septic shock for this patient. Which sources did you utilize to find evidence based information? What modification was made when there was an unintended outcome? Did you feel there was any conflict with the patient’s values or preferences? How has evidence based practice improved outcomes for patients with sepsis? Describe the level of “caring” that was demonstrated in communication with this patient and family. What was being done to facilitate the patient/family’s empowerment and shared decision making? How did developmental level and culture influence your interventions for the patient's pain and discomfort? (For the patient’s daughter) Describe the extent to which you felt were involved in the care being provided to your family member. Provide patient centered care with sensitivity and respect for human diversity (S) Safety Assess own level of communication skill in encounters with the patient and family (S) Examine human and environmental factors that impact patient safety (K) Use strategies to reduce reliance on memory (S) Use error reporting systems for error reporting (S) Participate in root cause analysis to analyze errors (S) Implement specific interventions addressed in the National Patient Safety Goals (S) Communicate observations or concerns related hazards or errors to members of the health care team (S) Describe factors that create a culture of safety ( K) Demonstrate effective use of standard practices to support patient safety (S) (recognize and intervene when patient’s status changes) Perform a physical assessment, comparing findings with textbook norms for the geriatric patient. What psychosocial and ethical considerations guided communication with the patient’s daughter? What cultural considerations influenced the care for this patient? National Patient Safety Goals Identify a “Do not use” abbreviation and implement appropriate action Complete a medication reconciliation form Validate the accuracy of telephone orders through “ read back and confirm” Respond immediately to critical lab results Identify a change in patient’s condition and call a “Rapid response” Utilize an organized format to provide hand-off communication Scan the environment to identify threats to patient safety and address problems. Provide feedback to ancillary staff when asepsis is broken Take appropriate action when a wrong IV solution is hanging. ( reporting and root cause analysis) Utilize strategies to validate information and to decrease reliance on memory. How did the nurse use initiative to resolve issues related to patient safety? What signs of multiple organ dysfunction did the patient exhibit and how did these impact safety? How did nurse implement strategies to minimize distraction and chaos during the stress of managing an unstable patient”? Describe factors that create a “culture of safety” in health care. What were possible root causes of the error that occurred in the simulation? What steps should the nurse take to prevent such errors in the future? How did the implementation of the sepsis bundle protocol contribute to patient safety? What are the criteria for a rapid response and which of these did you identify in this scenario? Which National Patient Safety goals were met during this scenario? What environmental factors did the nurse consider to ensure safety for this patient? Teamwork and Collaboration Describe the scope of practice and roles of health team members (K) Communicate assessment findings to the health care team, using SBAR format. Describe how interdisciplinary collaboration helped promote safe patient outcomes Function competently within own scope of practice as a member of the health care team. (S) Delegate appropriate tasks to unlicensed personnel and provide corrective action as needed to ensure patient safety. What led to your request to call for help? Initiate requests for help when appropriate to the situation. (S) Collaborate with other members of the health team (respiratory therapist, radiologic technician, case manager ) Collaborate and communicate with health team members to ensure continuity of care (S) Initiate actions to resolve conflict (S) Report critical information to the members of the Rapid Response team Manage conflict proactively when the resident asks the daughter to leave Describe the respective roles and responsibilities during the crisis? Describe the strengths and limitations of the teamwork in this scenario. Explain how conflict was resolved? How did the various team members prevent gaps in communication? Provide a comprehensive report to ICU Quality Improvement Identify gaps between actual and best practices in this simulation (S) Identify tools that can be used to collect data to understand variations in care (K) Describe approaches for changing processes of care (K) Seek information about Quality Improvement projects in the care setting (S) Work in a small group in the classroom or online to create a simulated quality Improvement project to reduce the incidence of nosocomial urinary catheter infections Identify factors in the scenario that would contribute to infection risk Explain how data would be collected Design a plan to effect a change to reduce the incidence of nosocomial UTI Explain how outcomes would be evaluated How would you describe the quality of care in this scenario? Who is responsible for quality in a health care setting? Describe the steps you would encounter in designing a quality improvement project to prevent nosomcomial urinary tract infections. How can the nurse motivate staff to implement changes directed to improve quality care? If you could experience this simulation again, what would you do differently?