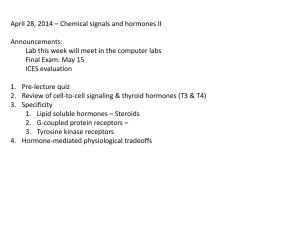
Case Studies 1-7
advertisement

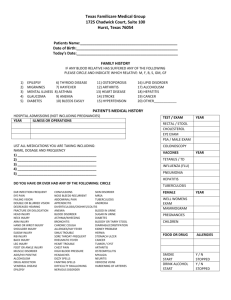
Endocrine Case Studies Case 1 Thomas L. a 28-year-old male, complained of abrupt polydipsia and polyuria. Blood and urine analyses provided the following results: Fasting blood glucose 93 mg/dL Serum sodium 145 mEq/L Serum potassium 2.8 mEq/L Urine osmolarity <200 mOsm/L Urine volume 15 L/day Urine glucose 0 Water deprivation and hypertonic saline infusion did not cause a significant reduction in the polyuria and concentration of urine. Complete water-deprivation resulted in the following: Urine osmolarity 225 mOsm/L. However, there was a significant concentration of the urine and a decrease in urinary output following administration of ADH. 1. Define polydipsia and polyuria. 2. To maintain a steady state, about how much fluid must Thomas drink per day? 3. Why was a water deprivation and hypertonic saline infusion ordered? How would a normal healthy person respond to these tests. Interpret the results of Thomas L.’s tests. 4. Why did the water deprivation and hypertonic saline infusion not result in a concentrated urine? 5. Are Thomas's kidneys capable of responding to ADH? What is the evidence? 6. What is the name of this endocrine disorder? 7. Is there a defective endocrine gland? If so, which is it? 8. Thomas L. was given a nasal spray containing a synthetic substance to self-administer to treat this condition. What type of compound was present in the nasal spray? 9. Why was this compound given as a nasal spray? Why not have Thomas take it in tablet form? 10. Diagram the hypothalamic-pituitary-target organ pathway for this individual and indicate the normal and pathophysiological conditions involved. 11. The symptoms appeared abruptly. What could have been the cause of this endocrine disorder? 11. What is the long-term prognosis for Thomas L? Must he take the nasal spray for the rest of his life? Why or why not? Case 2 Hazel C. a 30-year-old female demonstrated a subtle onset of the following symptoms: dull facial expression; droopy eyelids; puffiness of the face and periorbital swelling; sparse, dry hair; dry, scaly skin; evidence of intellectual impairment; lethargy; a change of personality; bradycardia (60 b/min); a blood pressure of 90/70; constipation, and hypothermia. Plasma concentrations of total and free T4 and T3 follow: Total T4 3 ug/dL (normal = 4-12 ug/dL) T3 0.14 ng/dL (normal = 75-195 ng/dL) Free 0.6 ng/dL 0.01 ng/dL Radioimmunoassay (RIA) of peripheral blood indicated elevated TSH levels. A TSH stimulation test did not increase the output of thyroid hormones from the thyroid gland. 1. Why does Hazel have a lower-than-normal body temperature? 2. How do Hazel's levels of T3 and T4 compare to normal? 3. What do Hazel's elevated levels of TSH reveal about the function of her anterior pituitary? about her thyroid glands? 4. What is a TSH stimulation test and how are the results interpreted? 5. Is this a primary or secondary disorder? How is this determined? 6. Name the endocrine disorder in this case. 7. Diagram the feedback loop involved. 8. What is a palpable goiter and would you expect to find a palpable goiter in this case? Explain your answer. 9. If a person has bradycardia and hypotension, which of the following hormones would most immediately restore heart rate and blood pressure to normal: TH or EPI? 11. What is the most likely explanation for the bradycardia and low blood pressure? 12. What is the most likely explanation for the constipation? 13. Describe a suitable treatment for Hazel. Would this treatment require injections or capsules? 14. Why would it be unnecessary to treat Hazel with supplemental EPI? 15. Is this treatment expected to return blood pressure and heart rate to normal? Why or why not? Case 3 Oscar T. a 45-year-old male from the Midwest presented with the following symptoms during February: weakness, fatigue, orthostatic hypotension, weight loss, dehydration, and decreased cold tolerance. His blood chemistry values follow: Serum sodium 128 mEq/L Serum potassium 6.3 mEq/L Fasting blood glucose 65 mg/dL Serum creatinine 0.5 mg/dL Hematology tests resulted in the following values: Hematocrit 50%; Leukocytes 5000/cu mm Oscar also noticed increased pigmentation (tanning) of both exposed and nonexposed portions of the body and back. A plasma cortisol determination indicated a low cortisol level. Following administration of ACTH, plasma cortisol did not rise significantly after sixty and ninety minutes. Endogenous circulating levels of ACTH were later determined to be significantly elevated. 1. What endocrine organ is the site of the malfunction? . Is this a primary or secondary disturbance? 2. What is the name of this disorder? 3. Discuss the electrolyte (Na+ and K+) disturbances resulting from this disorder. Which hormone is involved and are the levels of this hormone abnormally high or abnormally low? 4. Discuss the metabolic disturbances resulting from this disorder. Which hormone is responsible? 5. What is the cause of Oscar's tanning? 6. What type of replacement therapy would be required for Oscar? 7. Diagram the feedback loop for this endocrine disorder. 8. What is the long-term outlook for Oscar? Might one expect Oscar's abnormal pigmentation to resolve? Explain. Case 4 A 50-year-old male (Horace C.) had a total thyroidectomy followed by thyroid hormone-replacement therapy. Thirty-six hours later he developed laryngeal spasms, a mild tetany, and cramps in the muscles of the hands and arms. The following tests were performed: Urine calcium 20 mg/dL Urine phosphorus 0.1 g/day Plasma calcium 7.0 mg/dL Plasma phosphorus 5.0 mg/dL Calcium gluconate and vitamin D (calcitriol) were given orally each day and the tetany and laryngeal spasms were alleviated. (Your textbook will prove particularly useful in this case.) 1. What endocrine disorder is present in Horace? 2. What is the purpose of vitamin D administration with the calcium? 3. What caused Horace's tetany and laryngeal spasms? 4. How is blood calcium normally maintained at its physiological level? 5. Diagram the negative feedback loop for the hormone(s) involved. 6. Is hormone replacement therapy necessary for Horace or could his case be managed by nutritional supplements? Case 5 (requires some knowledge of pulmonary physiology) A 21-year-old noncompliant male with a history of type I (insulin-dependent) diabetes mellitus was found in a coma. His blood glucose was high, as well as his urine glucose, urine ketones, and serum ketones. His serum bicarbonate was <12 mEq/L. His respiration was exaggerated and his breath had an acetone odor. His blood pressure was 90/60 and his pulse weak and rapid (120). 1. Define noncompliant. 2. Is this person experiencing ketoacidosis or insulin shock? Explain your answer. 3. Why is the serum bicarbonate low? 4. What is the acid-base status of this individual? 5. What is the cause of the dyspnea, hypotension, and tachycardia? 6. What type of treatment does this person need? Case 6 A 59 year-old female complains of numbness of the hands, excessive sweating, and an unpleasant body odor. She also remarked that she has gone up a ring size and shoe size. Upon examination, she presents with the following symptoms: thick, oily skin; skin tags; impaired vision; headaches, fatigue, and weakness; and menstrual cycle abnormalities and breast discharge. Evaluation of a blood sample revealed the following levels: GH level (ng/ml) GHRH level (µg/mL) IGF-1 level (ng/ml) Blood pressure (mm Hg) Measured 16.3 0.08 1044 150/90 Normal <5 < 0.1 125 to 460 Below 120/80 1. What endocrine organ is involved? How does one determine which it is? 2. What is the name of this disorder? 3. What is an explanation for the patient's high blood pressure? 4. Give an explanation for the patient's breast discharge and unpleasant body odor? Based on the site of the disorder, what might the nature of the visual impairment be? 5. What could be a possible cause for the development of this disorder? 6. Diagram the negative feedback loop for the hormones involved. 7. What is a possible treatment for this disorder? Case 7 A thirty-five year old female visited her gynecologist early one morning and complained of the following symptoms: fatigue, depression, unexplained weight gain, and an irregular menstrual cycle. Her doctor ordered a series of tests to determine the cause of her symptoms. The following were reported: · Serum Human Chorionic Gonadotropin Test: Negative · Fasting Blood Glucose: 65 mg/dL · Serum Cortisol: 28 mg/dL · Leukocytes (WBC): 6,500 cu mm · Hematocrit: 43% The doctor reviewed her results and asked her to return to repeat the test the next afternoon. The results were nearly identical. Next, a dexamethasone test was ordered for the following morning and revealed that her cortisol level had decreased to 10 mg/dL. 1) What endocrine gland(s) is/are the site of malfunction? 2) What is the name of this disorder? 3) What are the possible causes of this disorder? 4) Is there a diurnal cycle for levels of cortisol in a healthy individual? Does this patient have a normal diurnal cycle? 5) What is a dexamethasone suppression test? Why was it ordered for this patient? How are the results of this test interpreted? 6) What does the dexamethasone suppression test reveal as to the site of endocrine disorder in this patient? 7) What other tests could be done to determine the exact cause of the malfunction of this endocrine gland? 8) What are the possible treatments for an individual with this disorder? 9) What is the long term outlook for this patient? Case 8 Susie B., a three and a half-year-old female, is brought to the hospital by her parents who are concerned about her slow growth, night sweats, and craniofacial abnormalities. Blood analyses provided the following results: - Fasting Glucose: 42 mg/dL - Serum sodium: 140 mmol/L - 8am Cortisol: 28 mg/dL - Fasting GH: 9 ng/dL - IGH-1: 12 ng/dL Upon observation, craniofacial abnormalities include protruding forehead, small (double) chin, delayed teething, sparse hair. Slow motor development was also observed. She was unresponsive to growth hormone therapy treatments. Normalization of growth was observed with IGH-1 therapy. Questions: 1. What types of cells are abnormal in this patient? How do you know? 2. What could be a possible cause of high GH and cortisol levels? 3. What is a possible explanation for retarded growth in the presence of high GH levels? 4. Describe the feedback loop involved. 5. What is the most likely diagnosis for Susie? 6. Why did treatment with IGH-1 work for Susie, while GH therapy did not? 7. What's the prognosis for Susie with AND without IGH-1 treatment? Case 3 Oscar T. a 45-year-old male from the Midwest presented with the following symptoms during February: weakness, fatigue, orthostatic hypotension, weight loss, dehydration, and decreased cold tolerance. His blood chemistry values follow: Serum sodium 128 mEq/L Serum potassium 6.3 mEq/L Fasting blood glucose 65 mg/dL Hematology tests resulted in these values: Hematocrit 50%; Leukocytes 5000/cu mm Oscar also noticed increased pigmentation (tanning) of both exposed and nonexposed portions of the body and back. A plasma cortisol determination indicated a low cortisol level. Following administration of ACTH, plasma cortisol did not rise significantly after sixty and ninety minutes. Endogenous circulating levels of ACTH were later determined to be significantly elevated. 1. What is orthostatic hypotension? 2. What hormone from which organ is most likely involved with Oscar's serum electrolyte imbalance? 3. Is Oscar anemic? Which of the test results answers this question? 4. Does Oscar have an infection? Which of the test results answers this question? 5. Which hormone is most likely associated with the symptoms of weaknesss, fatigue, weight loss and decreased cold tolerance? 6. What endocrine organ is the site of the malfunction? What hormones are normally secreted from this gland? Is more than one hormone deficient in Oscar? 7. What is the name of this disorder? 8. Is this a primary or secondary disturbance? Explain your answer. 9. In a normal person, how would plasma cortisol levels be affected following administration of ACTH? What do Oscar's ACTH test results imply? 10. Why is Oscar's endogenous circulating level of ACTH significantly elevated? 11. What is the cause of Oscar's hyperpigmentation? How is this related to his high levels of ACTH? 12. What type of replacement therapy would be required for Oscar? Will the replacement of one hormone suffice to treat all his symptoms? 13. Diagram the feedback loops for this endocrine disorder. 14. What is the long-term outlook for Oscar? Might one expect Oscar's abnormal pigmentation to resolve once his treatment has begun? Explain. Case 4 A 50-year-old male (Horace C.) had a total thyroidectomy followed by thyroid hormonereplacement therapy. Thirty-six hours later he developed laryngeal spasms, a mild tetany, and cramps in the muscles of the hands and arms. The following tests were performed: Plasma calcium 7.0 mg/dL Plasma phosphorus 5.0 mg/dL Plasma chloride 99 mEq/L 1. Of the plasma electrolytes, which is most seriously disturbed? 2. What hormone(s) regulate plasma calcium? 3. What gland is the source of those hormone(s)? 4. What has happened to those glands in Horace? 5. What endocrine disorder is present in Horace? Could this have been avoided? 6. What caused Horace's tetany and laryngeal spasms? As a follow-up, calcium gluconate and vitamin D (calcitriol) were given orally each day and the tetany and laryngeal spasms were alleviated. 7. During the treatment phase, what is the purpose of vitamin D administration with supplemental calcium? 8. Diagram the negative feedback loop for the hormone(s) involved and be sure to identify the effectors. 9. Is hormone replacement therapy necessary for Horace or could his case be managed by supplements and vitamins?