Synchronization with spontaneous ventilation on breathing pattern
advertisement
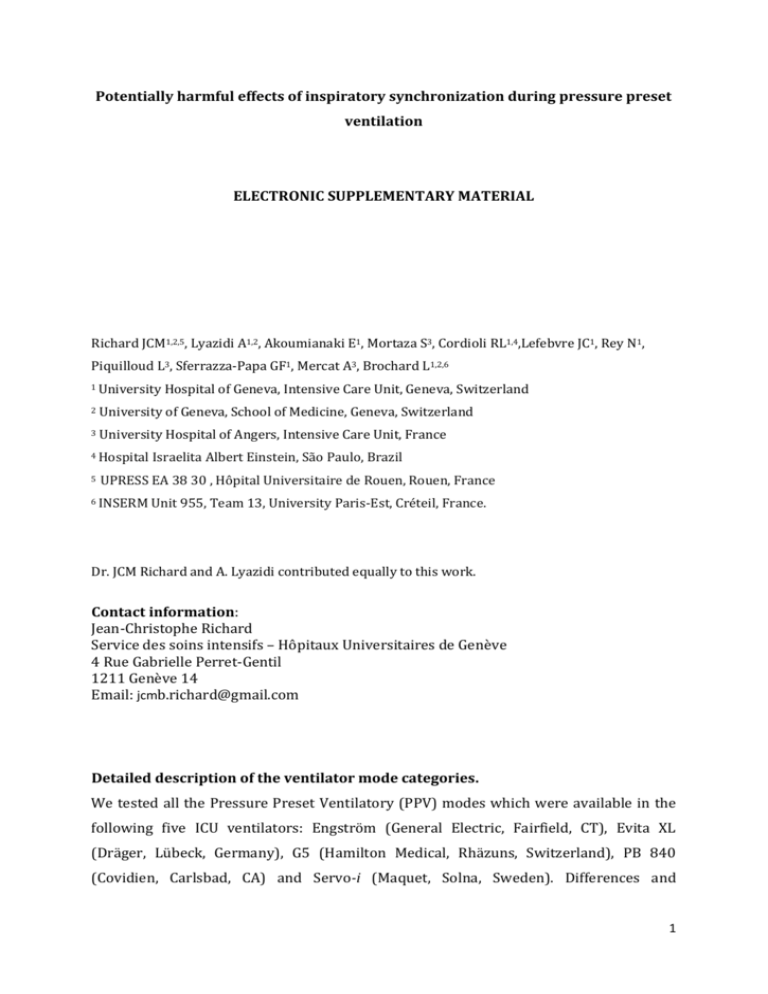
Potentially harmful effects of inspiratory synchronization during pressure preset ventilation ELECTRONIC SUPPLEMENTARY MATERIAL Richard JCM1,2,5, Lyazidi A1,2, Akoumianaki E1, Mortaza S3, Cordioli RL1,4,Lefebvre JC1, Rey N1, Piquilloud L3, Sferrazza-Papa GF1, Mercat A3, Brochard L1,2,6 1 University Hospital of Geneva, Intensive Care Unit, Geneva, Switzerland 2 University of Geneva, School of Medicine, Geneva, Switzerland 3 University Hospital of Angers, Intensive Care Unit, France 4 Hospital 5 Israelita Albert Einstein, São Paulo, Brazil UPRESS EA 38 30 , Hôpital Universitaire de Rouen, Rouen, France 6 INSERM Unit 955, Team 13, University Paris-Est, Créteil, France. Dr. JCM Richard and A. Lyazidi contributed equally to this work. Contact information: Jean-Christophe Richard Service des soins intensifs – Hôpitaux Universitaires de Genève 4 Rue Gabrielle Perret-Gentil 1211 Genève 14 Email: jcmb.richard@gmail.com Detailed description of the ventilator mode categories. We tested all the Pressure Preset Ventilatory (PPV) modes which were available in the following five ICU ventilators: Engström (General Electric, Fairfield, CT), Evita XL (Dräger, Lübeck, Germany), G5 (Hamilton Medical, Rhäzuns, Switzerland), PB 840 (Covidien, Carlsbad, CA) and Servo-i (Maquet, Solna, Sweden). Differences and 1 similarities concerning the function of PPV modes in each ventilator tested are presented in Table 1S. In the presence of spontaneous inspiratory efforts the PPV modes differ with regard to the presence of an inspiratory synchronization window i.e. a time period during which the ventilator can be triggered by the patient. We called this attempt of the ventilator to provide pressure delivery in response to patient’s effort ‘inspiratory synchronization’ (isynchronization). We subsequently defined three PPV mode categories based on their different levels of i-synchronization: (1) Non i-synchronized modes are those, in which the ventilator is never triggered by the patient, i.e., the ventilator does not attempt to synchronize the transition between the two pressure levels with patient’s effort. The mode that falls into this category is ‘Airway Pressure Release Ventilation’ (APRV) in Evita XL and G5 and Pressure Assist Control (PAC) with the inspiratory triggering inhibited in the Engström ventilator. Despite different names it functions identically in all three ventilators: it is a timetriggered and time-cycled PPV mode allowing, though, unrestricted spontaneous breathing due to a constantly open expiratory valve. Non i-synchronized PPV mode is not available in PB 840 and Servo-i ventilator. (2) In partially i-synchronized modes there is an i-synchronization window. Provided that spontaneous efforts appear during this window the ventilator will be triggered. Hence, whether an effort manages to trigger the ventilator depends not only on the phase of the cycle in which it occurs (inspiratory, expiratory) but also on the duration of the synchronization window: the longer the window the more likely for an effort to trigger the ventilator. The latter differs from one ventilator to another (Table 1S). Partially i-synchronized modes are available in all ventilators tested. However, they are named differently: Biphasic positive airway pressure (BIPAP), BiLevel, Bivent, DuoPaP. In all but one (Engström) ventilators tested, partially i-synchronized modes allows the addition of pressure support (PS) either for any spontaneous effort (Servo-i) or, more commonly, for efforts occurring during PEEP level (PB 840, G5, and Evita XL). (3) In fully i-synchronized modes any effort occurring at PEEP level will trigger the ventilator. This category corresponds to pressure assist control (PAC) in Engström, G5, PB 840 and Servo-i and to BIPAP assist in Evita XL. Detailed description of sedation protocol during the observational study. 2 Nurses adapted sedation three times per day according to the algorithm that proposed four distinct rules according percentage (%) of spontaneous ventilation (SV), pH and Richmond Agitation Sedation Scale (RASS) score. The RASS target was -2 to -3. The percentage of SV during APRV should be kept between 10 to 50% of total mechanical ventilation and it can be easily assessed at the bedside by means of the trends displayed on the screen of Dräger ventilator (figure 2S) and pH should stay between 7.30 to 7.45. 1. SV < 10% and RASS < - 2: consider sedation decrease (too much sedation) 2. SV < 10% and RASS OK (pH>7.45): consider reduction in RR of APRV (too much ventilation) 3. SV > 50% and RASS OK (pH<7.30): consider increase of RR of APRV (ventilation insufficient) 4. SV > 50% and RASS > -2: consider increase sedation (not enough sedation) 3 Ventilator EvitaXL G5 Modes I synchronization APRV Non BIPAP Partially BIPAPassist Fully APRV Cycle Time-trig only Time-trig or Patient-trig (variable synch. window) Time-trig or Patient-trig (Any effort at PEEP) Time-cycled only Time-cycled or Patient-cycled (variable synch. window) Rate Unrestricted Rate Unrestricted Time-cycled only THIGH Unrestricted NA Non Time-trig only Time-cycled only Rate Unrestricted Relative to PEEP level Partially Time-trig orPatient-trig (Synch. window for the last 25% of TLOW, max 1.5 s) Time-cycled or Patient-cycled (Synch. window for the last 25% of THIGH, max 1 s) Rate Unrestricted Relative to PEEP level Fully Time-trig or Patient-trig (Any effort at PEEP ) Time-cycled only THIGH Insp: Unrestricted Exp: Not possible NA Partially Time-trig or Patient-trig (Synch. window for the last 25% of PEEP ) Time-cycled or Patient-cycled (Synch. window for the last 25% of THIGH) Rate Unrestricted Relative to PEEP & to PHIGH level PAC Fully Time-trig or Patient-trig (Any effort at PEEP ) Time-cycled only THIGH Insp:Unrestricted Exp: Possible (Paw > 3 cmH2O) NA BiLevel Partially Time-cycled or Patient-cycled (Synch. window for the last 30% of THIGH, max 3 s) Rate Unrestricted Relative to PEEP level PAC Fully Time-cycled only THIGH Unrestricted NA Bilevel Partially Time-trig or Patient-trig Time-cycled or Patient-cycled (variable synch. window) Rate Unrestricted Relative to PEEP level PAC Fully Time-trig or Patient-trig (Any effort at PEEP ) Time-cycled only Rate Unrestricted NA Non Time-trig only Time-cycled only Rate Unrestricted NA DuoPAP Bi-vent Servo-i Engstrom Parameter constant SPONTANEOUS CYCLES Additional During PHIGH PS Trigger PAC PB 840 MANDATORY CYCLES trigger ON PAC (APRV) trigger OFF Time-trig or Patient-trig (Synch. window for the last 40% of PEEP , max 4 s) Time-trig or Patient-trig (Any effort at PEEP ) NA Relative to PEEP level 4 Table 1S: Description of the different names of pressure preset modes and their characteristics in the five ICU ventilators tested. Hence PEEPhigh or Phigh correspond to high airway pressure; TPEEP or TPEEPlow is the time spent at PEEP (or low airway pressure) and THIGH or TPEEPhigh or TINSP the time at high airway pressure. NA: not applicable 5 Figure 1S: The percentage of spontaneous ventilation during APRV displayed on the screen of Dräger ventilator indicating total minute ventilation and spontaneous ventilation (black and gray on the ventilator screen, respectively). 6 I-synchronized cycles Non i-synchronized mode (ml/kg) 10 VT (ml) Mandatory cycles 6 Spontaneous cycles in PEEP 4 0 (ml/kg) 10 Partially i-synchronized mode VT (ml) 6 4 0 (ml/kg) 10 Fully i-synchronized mode VT (ml) 6 4 0 Without inspiratory effort With inspiratory effort Time (sec) Figure 2S: Volume-time curves of the 3 different PPV modes, before and after the initiation of spontaneous efforts. The inspiratory to expiratory ratio was 1:3. The dotted horizontal lines below and above 6ml/kg/ ideal body weight (IBW) correspond to 4 and 10 ml/kg IBW, respectively. The VT values are expressed in ml/kg IBW for a male subject of 182 cm height and IBW of 75 kg. As the level of synchronization increases, the occurrence of cycles with high VT increases (i-synchronized cycles). 7 Figure 3AS: The i-synchronization effect of spontaneous breathing during pressure preset ventilation modes. Tidal volume and its variability at a spontaneous respiratory rate of 30 cycles/min and an I:E ratio of 1:3. Partially i-synchronized modes were tested with and without pressure support (PS) for efforts occuring at PEEP level. 8 I/E 3:1 RR 30 1000 70 60 Tidal volume (ml) 50 600 40 30 400 20 200 10 0 Non i-synchronized modes Partially i-synchronized modes PS 0 Partially i-synchronized mode PS 15 Fully i-synchronized modes Coefficient of variation (%) 800 0 Figure 3BS: Tidal volume and its variability at a spontaneous respiratory rate of 30 cycles/min and an I:E ratio of 3:1. Partially i-synchronized modes were tested with and without pressure support (PS) for efforts occuring at PEEP level. *p<0.05 vs non isynchronized modes, † p<0.05 vs partially i-synchronized modes (PS 0) 9 Figure 4S: Tidal volume and its variability at a spontaneous respiratory rate of 20 cycles/min and an inspiratory to expiratory ratio of 3:1. Partially i-synchronized modes were tested with and without pressure support (PS) of inspiratory efforts at PEEP level. 10 Table 2S: Tidal volume measured at each ventilator during spontaneous breathing. The inspiratory to expiratory ratio was 1:3 and the respiratory rates tested were 20 and 30 cycles/min. Partially i-synchronized modes were tested with and without pressure support (PS) of inspiratory efforts at PEEP level. *p<0.05 vs non i-synchronized modes, † p<0.05 vs partially i-synchronized modes (PS 0), ‡ p<0.05 vs partially i-synchronized modes (PS 15). 11 Comparative study Study Observationnel study Patient Sexe Age Weight (years) (kg) Size (cm) IGS2 PaO2/FiO2 Crs Ventilation ICU stay (mmHg) (ml/cmH2O) (days) (days) Recording duration (days) ARDS etiology P01 M 47 73 172 44 147 22 7 10 1 Pneumonia P02 M 83 112 165 36 100 29 15 16 6 Pneumonia P03 M 63 76 158 52 77 36 50 60 14 Pneumonia P04 M 66 79 162 30 108 18 8 8 2 Pneumonia P05 F 77 67 164 50 96 21 32 32 7 Pneumonia P06 F 36 68 165 30 74 18 6 8 3 Pneumonia P07 F 64 101 156 71 86 27 7 7 5 CPR P08 F 41 64 159 35 118 24 5 9 2 Malaria Mean 60 80 163 44 101 24 16 19 5 (SD) (16) (17) (5) (14) (24) (6) (16) (18) (4) P01 M 44 57 163 36 180 35 16 35 NA Pneumonia P02 F 66 65 169 89 169 71 10 15 NA Pneumonia P03 F 80 62 160 79 236 22 5 7 NA Pneumonia P04 M 83 74 167 59 233 44 12 15 NA Pneumonia 68 (18) 65 (4) 165 (4) 66 (23) 205 (35) 43 (21) 11 (5) 18 (12) NA Mean (SD) Table 3S: General clinical characteristics 12 Figure 5S: Individual averaged VT according to the PPV modes tested during the clinical comparative study. Patient number 02 ventilated with I:E ratio of 1:3.2 exhibited larger VT during PAC compared to the 3 others patients ventilated with a I:E around 1:2. 13