Highlights of Unit 3: Classification of mechanical ventilation

Highlights of Unit 3:
Classification of mechanical ventilation
By Elizabeth Kelley Buzbee AAS, RRT-NPS, RCP
obtains power and converts this power into a force that can move gas into a patient’s lung.
Sends gas down a circuit to the patient interface and back to ventilator for analysis of data
The parts of a mechanical ventilator
is dependent on the patient’s R
AW his compliance
, the volume required and the elastic recoil of the lung
Mechanical ventilators and the
WOB
How does it get power to operate?
How does it use this power to drive gas into the patient and how does it control the flow of gas into the patient?
How does it control the various parameters of ventilation such as starting and stopping a breath?
How does it communicate information to the operator in such a manner that the
RCP can monitor the patient’s responses and modify the ventilator’s action?
We classify ventilators by these questions
electrical power : A/C D/C 110-115 volt current
pneumatically-powered.
50-60 psig
Battery powered [emergency only or transport]
◦ Internal batteries
◦ External batteries
◦ Run about one hour then require 8-12 hours to recharge
Input Power
How does this machine get power to operate?
Drive mechanisms
◦ Compressors
piston-driven-
◦ rotary–driven- delivers a Sine wave
◦ linearly driven-- constant flow pattern .
Bellows: start with constant flow but as pressures rise and R
AW increases results in descending
◦ spring,
◦ a weight
◦ gas pressure
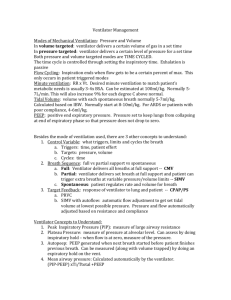
Power transmission and conversion
How does it use this power to drive gas into the patient?
microprocessors are tiny computers that do only one or two tasks
solenoid valves control flow to the patient by electronic switching
Electromagnetic
Pneumatic poppet valves
Proportional solenoid valves
Output control valves:
How does it control the flow of gas into the patient?
Fluidics use gas power, but differs from pneumatic in that there are no moving
parts.
◦ Coanda effect- gas moves along the side of the wall and we can direct gas to go down another tube by application of gas into that flow to move it
pneumatic control: uses gas but there are moving parts- mushroom valves ect
Fluidic and pneumatic control
Means of Communication:
How does it communicate information to the operator in such a manner that the RCP can monitor the patient’s responses and modify the ventilator’s action
?
Monometers/
◦ bourdon gauges- measure pressure
◦ digital monometer may be displayed as a
bargraph, or as numbers
Spirometers: Volume measurements
Waveforms alarms
Apnea alarm: adults 20 seconds; when these alarms go off the apnea parameters on many ventilators will start breathing for the patient
Loss of electrical power alarm: if battery operational will come on with indicator light
Loss of gas power alarm: may ventilate patient will remaining gas
Disconnect alarms: may have a time delay
Low or high humidifier temperature-
0
Where do we set the alarm limits?
High/Low V
E
: V
E needs to stay within 10-
20% +/- [or 2-5 LPM above and below]
V
T
alarms: 100 ml lower than set V
T
Low airway pressure alarmabout 5-10 cmH20 below average PIP.
High airway pressure – 10-20 above average PIP; when this goes off, the breath will stop [pressure-cycled]
Where do we set the alarm limits?
Fi0
2
alarms -5% +/-.
High/low rate alarms: more than 10-
20% from baseline—
Loss of PEEP/CPAP alarms: are generally set about 3-5 below the PEEP
Where do we set the alarm limits?
How does the mechanical ventilator control the various parameters of ventilation such as starting and stopping a breath?
Control variables:
Open vs. closed loop control of ventilator output
open; we dial in a VT or a f and the machine delivers the VT to the circuit. the open loop machine will not adjust.
In an closed loop system the ventilator is smart enough to monitor and interpret changes in such a way that the machine will alter the next breath to maintain the
VT.
A control variable is the primary variable that the ventilator manipulates to cause an inspiration:
Pressure controlled [PC]
Volume controlled [VC]
Flow controlled
Time [usually based on the other parameters]
Only one control, the other two will be variables
a PC [pressure controlled] breath is one in which the pressure stays the same, but changes in the patient’s condition will alter the delivered volume and the flow rate.
The doctor orders a PIP which will deliver a VT
Pressure control:
During VC ventilation, the PIP varies with changes in the patient’s conditions, while the volume and the flow stay constant.
The doctor orders a VT
Volume controlled:
mechanical ventilators had consistent flow rate and volumes, but the airway pressure changed with patient parameter changes.
The doctor will order a VT but we will set up the flow rate and the Ti to deliver this
VT
Flow controlled
What event triggers inspiration, what stops the breath, what changes the breath?
Phase Variables:
Trigger: what starts the inspiratory phase?
Limit: what limits the actual inspiratory cycle without stopping it?
Cycle: what cycles the inspiratory phase off- starts exhalation?
Baseline: what changes the base line pressures? PEEP or CPAP
Phase variables:
Time triggering.
At 10 BPM, there is a breath initiated by the ventilator every 6 seconds [cycle time]
Patient triggered : the inspiration is started by the patient demand. is called the
“Sensitivity.”
◦ pressure trigger
◦ flow trigger
◦ volume trigger
◦ NAVA
Manual trigger : push a button on the ventilator to trigger a breath– used during suctioning
What event triggers inspiration?
set the Sensitivity knob to -.5 to -1.5 cmH
2
0. if the Sensitivity is adjusted from -1 to -3, we say that the sensitivity is decreased; the patient’s WOB is increased.
The patient creates a pressure gradient
◦ If there is a leak in the system the pressure may not drop.
◦ Complicated by having to drop the pressure all the way back to the ventilator
◦ If baseline pressure rises, may not be able to pressure trigger
◦ If there is auto-PEEP from air trapping, the pressure cannot drop enough to trigger a breath
Pressure triggered:
There is always a small constant flow moving through the circuit
2 Pneumotachymeters measure and compare the flow coming to patient and going away from patient.
As the patient pulls in the gas, there is now less expiratory flow than inspiratory flow, and it is this flow gradient that will trigger a breath
Usual set 1-3 LPM in adults
Flow triggered
Water in the circuit can mimic a breath and trigger more breathes than patient needs
Leaks can also alter the constant flow so that the machine may ‘auto-cycle’ or
‘chatter’
Problems with flow triggers
only the Drager Baby Log actually uses the volume inspired by the patient to trigger a breath
Volume triggered
Neutrally adjusted ventilatory assist
A probe is sent down the esophagus and as the phrenic nerve fires, the probe’s sensor notes the breath effort and triggers the ventilator.
NAVA
If not sensitive enough
◦ Increased WOB
◦ ‘asynchrony with the ventilator’
◦ ‘Fighting the ventilator’
If too sensitive
◦ Triggers too many breaths– called ‘chattering
‘or ‘auto-cycling’
◦
◦ Could lead to air trapping and baratrauma
What happens when triggering is not accurate or responsive?
A limit on a breath is some parameter that affects the breath without stopping it.
◦ A pressure limit may mean that the patient continues to deliver the VT but the flow slows down in an attempt to keep the airway pressures down
◦ The actual VT delivered is usually decreased, but still higher than it would be if the breath was pressure cycled off
Limit: what limits the actual inspiratory cycle?
many manufacturers use the term
“limit” when discussing alarms.
If a high pressure alarm is set and the breath stops being delivered once that PIP limit is exceeded, it is not pressure limiting; it is pressure cycling off.
IMPORTANT:
what parameter cycles the inspiratory
phase off- starts exhalation?
◦ Volume cycledwhen preset VT is reached.
Most VC breaths are also volume-cycled
◦ Time cycledthe breathes initiated by the ventilator can be time triggered and maybe time cycled off. Most PC breaths will be timecycled off
◦ Pressure cycledin VC ventilation, if the high pressure alarms goes off and the breaths stops we can say that the breath was pressurecycled.
◦
Cycle:
flow cycle
◦ Some ventilators will cycle off once a preset low flow rate is noted.
◦ You can see this on the graphic when we watch the descending flow wave suddenly drops to zero
◦ This occurs always with PS breaths and you might be able to chose flow cycling with the VC mandatory breaths
Flow cycling
We can raise the pressure during exhalation phase from zero to a positive number; we have raised the baseline
Baseline: What changes the base line pressure?
◦ Both raise the baseline pressure
◦ Both used to treat refractory hypoxemia
◦ Both will increase the FRC and can increase the lung compliance
◦ PEEP positive end-expiratory pressure ‘ with a ventilator rate set [full or partial support] the lower pressure
◦ CPAP- ‘continues positive airway pressure’ without a ventilator rate set [a spontaneous mode] the only pressure
PEEP or CPAP?
Keep more air inside alveoli and airways
◦ Raises RV [residual volume] which raises the FRC
Return the FRC to normal will generally increase the lung compliance and decrease the WOB
Excessive PEEP
◦ hampers CO, increases VD and causes air trapping and can damage the lung tissue
◦ If patient is on PC ventilation, raising PEEP might decrease the VT because the driving pressure drops.
Excessive CPAP can decrease VT which will raise the PaC02
Effects of increased baseline pressure
small amount of gas are trapped because the exhalation valves closes before the circuit pressure drops back to zero.
How much gas is left in the lung is a function of :
◦ level of PEEP selected,
◦ I:E ratio [if the exhalation time is too short more gas can trap
◦ time constant of the lung units.
With PEEP
flow restrictor : the exhalation port is too small for the gas to all escape. The faster the flow through the tiny hole, the more back pressure the flow restrictor creates threshold resistor : creates back pressure that is independent of flow rate.
In these types of PEEP valves, the gases passes freely until some balances of forces on the other side equalize and the pressure is held in the circuit.
basic types of PEEP/CPAP devices
Water Column:
Weighted ball:
Flexed springs:
Venturi diaphragm:
Electromagnetic valve:
Types of threshold PEEP valves
When the flow is too fast for the exhalation valve to get all the gas out
Ventilator circuits are rated for their resistance to flow and a max flow rate will be suggested.
Failure to keep the flow rate below this max will result in PEEP rising as the flow rate rises.
This is a real issue with neonatal circuit that are so tiny that airway resistance rises quickly