predictors of 30-day readmission in patients treated with robot
advertisement

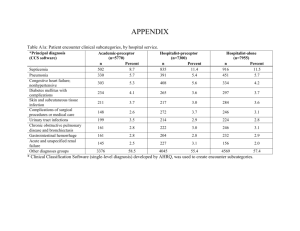
INCIDENCE AND PREDICTORS OF 30-DAY READMISSION IN PATIENTS TREATED WITH ROBOT-ASSISTED RADICAL PROSTATECTOMY Introduction. Although several studies reported advantages related to the adoption of robot-assisted radical prostatectomy (RARP) in terms of postoperative pain, blood transfusions, and length of hospital stay, evidence is scarce regarding the incidence and predictors of readmission in these patients. Methods. Overall, 1,402 prostate cancer (PCa) patients treated with RARP at a single center between 2006 and 2013 were identified. Baseline comorbidities were categorized according to the Charlson comorbidity Index (CCI). Postoperative complications during the first hospitalization were both categorized using both the Clavien-Dindo classification system and detailed as follows: bleeding/haematoma, lymphorrhoea/lymphocoeles, fever, urinary fistula, cardiovascular event, and other. Patients experiencing 30-day readmission were identified. Uni- and multivariate logistic regression analyses tested the association between 30-day readmission and age at surgery, the receipt of pelvic lymph node dissection, CCI, and the severity of postoperative complications classified according to the Clavien-Dindo system as well as the type of postoperative complications. Results. Median patient age was 63 years. Overall, 161 (11.5%) patients experienced a postoperative complication during the first hospitalization. The most frequent type of complication was bleeding/haematoma (6.1%), followed by lymphorrhoea/lymphocoeles (1.4%). Clavien- Dindo distribution during first hospitalization was 0 in 1241 (88.5%), 1 in 53 (3.8%), 2 in 69 (4.9%) and ≥3 in 39 (2.8%) patients. Overall, 38 patients (2.7%) needed a new hospitalization within 30 days after discharge. The most common causes of re-hospitalization were fever in 12 patients (31.6%), lymphoceles in 11 (28.9%) and urinary leak in 6 (15.8%). The proportion of patients who experienced 30-day readmission was significantly higher among patients who had a complication during the first hospitalization compared to those who did not experience a complication during the first hospitalization (6.2 vs. 2.3%, respectively; P=0.01). At multivariable analyses, the occurrence of a complication during the first hospitalization and its severity represented independent predictors of 30-day readmission, after accounting for confounders (all P<0.01).When looking at the type of complication, fever (OR: 7.05; P=0.01), urinary fistula (OR: 13.41; P<0.01), and cardiocirculatory complications (OR: 19.05; P<0.001) were significantly associated with 30-day readmission. Conclusions. Our observations show that patients undergoing RARP have a relatively low risk of 30-day readmission (2.7%). Of note, the occurrence of a postoperative complication represented the only independent predictor of 30-day readmission. In this context, fever, urinary fistula, and cardiovascular complications represent the type of complications significantly associated with higher risk of readmission. Our findings highlight the need for better patient management when a complication occurs during hospitalization for RARP.