HOSPITAL REIMBURSEMENT
Research
HIGHLIGHTS
Although patient race
significantly impacts hospitals’
30-day mortality and
readmission rates, these effects
are not taken into account in
CMS’s Hospital Compare data.
Risk-Standardized Rates for 30-Day
Mortality and Readmissions Vary
Significantly by Race
July 2011
David Foster, PhD, MPH | Janet Young, MD, MHSA | Sivana Heller, MD, MPH
This inequity could soon
become a real financial problem
for hospitals: starting in 2013,
the healthcare reform law will
allow CMS to penalize hospitals
for excess readmission rates.
Summary
Investigating discharge data
can provide value to hospitals
that are looking to better
understand the implications
of 30-day mortality and
readmission rate data.
The data in this study demonstrate that unless race is taken into account, bias may
The objective of this study was to evaluate the impact of race on risk-standardized,
30-day mortality and readmission rates used in the Centers for Medicare & Medicaid
Services (CMS) Hospital Compare reporting.
occur in comparing 30-day readmission for acute myocardial infarction (AMI),
heart failure, and pneumonia patients and 30-day mortality rates for heart failure
patients. And because CMS does not currently consider race when producing its
risk-standardized rates, differing race populations across hospitals may cause unfair
hospital comparisons.
Methodology
We performed a cross-sectional, correlation, and rate-comparison analysis of race
(black, white, or other) with 30-day, risk-standardized mortality and readmission
rates. Standard logistic regression models were used and specified as closely as
possible to the CMS Hospital Compare models by Krumholz.1,2
For validity and a more detailed profile, we performed this analysis by Hospital
Compare hospital-level data and discharge-level data. The data sources for each
were:
§§ 30-day mortality and 30-day readmissions for hospital-level results: Hospital
Compare data for Medicare patients with AMI, heart failure, or pneumonia from
the third calendar quarter of 2007 through the second calendar quarter of 2010
(hospitalcompare.hhs.gov/staticpages/for-professionals/poc/data-collection.aspx)
§§ 30-day mortality for discharge-level results: CMS Medicare Provider Analysis
and Review (MedPAR) data for Medicare patients with AMI, heart failure, or
pneumonia from the third calendar quarter of 2007 through the second calendar
quarter of 2010
§§ 30-day readmissions for discharge-level results: Calendar year 2010 CMS Standard
Analytical Files (SAF) — the only available SAF data with dates included
Research Brief
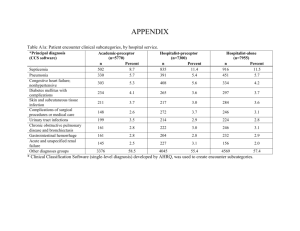
Results
We found that rates of 30-day mortality and readmissions were significantly and
substantively correlated with hospital proportional distribution of race (black,
white, or other) — suggesting that race is an uncontrolled confounder in the CMS
methodologies.
This analysis uses Pearson correlations, the most common measure of correlation
used in statistics, to define the relationships between race and rates. A Pearson
correlation shows the degree of correlation, or linear dependence, between two
variables using a value between +1 and -1. A correlation of +1 means that there is a
perfect positive linear relationship between variables, -1 means that there is a perfect
negative linear relationship, and 0 means there is no linear relationship. We found:
§§ Increased hospital-specific proportion of white patients with heart failure was
associated with significantly higher rates of 30-day mortality compared with
patients who had race coded as black or other (Figure 1).
§§ Increased hospital-specific proportion of whites was significantly associated with
decreased rates of 30-day readmissions among patients with AMI, heart failure,
and pneumonia (Figure 2).
§§ There is a statistically significant correlation between average, 30-day, riskstandardized rates and the proportion of white race (Figure 3).
Figure 1: As Proportion of White Patients Increases Relative to Black or Other
Patients, the Risk of 30-Day Mortality for Heart Failure Increases
Pearson Correlation Coefficient
Pearson Correlation Between Risk-Standardized, 30-Day Mortality Rate
and Hospital Race Proportion
Proportion White
Proportion Black
Proportion Others
0.3
0.2
0.1
0.0
-0.1
-0.2
-0.3
Heart Failure Death
Pneumonia Death
Heart Attack Death
Pearson Correlation Coefficient
Figure 2: As Proportion of White Patients Increases Relative to Black or Other
Patients, the Risk of 30-Day Readmissions is Decreased for all Three Patient Groups
0.4
0.3
Pearson Correlation Between Risk-Standardized, 30-Day Readmission Rate
and Hospital Race Proportion
Proportion White
Proportion Black
Proportion Others
0.2
0.1
0.0
-0.1
-0.2
-0.3
-0.4
Heart Failure Readmission
Pneumonia Readmission
Heart Attack Readmission
Figure 3: The Proportion of White Patients Relative to Black and Other is Associated
With Risk of 30-Day Mortality and/or Readmissions for Some Patient Groups
Association Between Average, 30-Day, Risk-Standardized Rates and Proportion of
White Race in Clinical Group (P<0.0001 for All Slopes)
Average Risk-Standardized Rate (%)
28
26
24
22
20
18
Heart Failure Readmission
Heart Attack Readmission
Pneumonia Readmission
Heart Failure Mortality
16
14
12
10
1 2 3 4 5 6 7 8 910
Decile of Proportion White Race (10=Highest Proportion)
The above results are gleaned from CMS Hospital Compare data, but similar results
are also found when reviewing discharge-level CMS MedPAR data. Figure 4 also
shows that white patients have higher 30-day mortality rates than blacks and others.
Figure 4: White Patients Have Higher Risk-Adjusted Rates Than Blacks and Other
Patients on 30-Day Mortality, Based on Discharge-Level CMS MedPAR Data
16
Risk-Adjusted Rate (%)
14
Risk-Adjusted Rates for 30-Day Mortality Vary by Race, Based on CMS
MedPAR Data
White
Black
Other
12
10
8
6
4
2
0
AMI
Heart Failure
Pneumonia
A crude death rate analysis (without risk adjustment) supports the hypothesis that
competing causes of death are responsible for higher 30-day mortality among whites
(Figure 5).
Figure 5: Crude Death Rates Show Black Patients Have Higher Observed Mortality
Rates at Younger Ages Than Whites
Crude Death Rates per 100,000 by Race, 2008
Deaths per 100,000 Population
16,000
14,000
White
Black
12,000
10,000
8,000
6,000
4,000
2,000
0
1-4
5-14 15-24 25-34 35-4445-54 55-64 65-74 75-84 85+
Age Categories
Model Performance for Discharge-Level Results
We used standard logistic regression models specified as closely as possible to the
CMS Hospital Compare models by Krumholz.1,2
The Pearson correlations for the 30-day mortality models were 0.82, 0.75, and 0.83
for pneumonia, AMI, and heart failure, respectively. The Pearson correlations for the
30-day readmission models were 0.50, 0.31, and 0.59 for pneumonia, AMI, and heart
failure, respectively. All correlations were statistically significant (p < 0.0001).
Limitations
Because only administrative data (Uniform Billing, UB) were used for this study,
differences across hospitals in coding practices, limitations in risk-standardization,
and other factors should be taken into consideration.
The models built to estimate the discharge-level results represented by the CMS
Hospital Compare hospital-level results, while as close as possible, were necessarily
imperfect due to our inability to use exactly the same data and patient population
used by CMS.
Conclusions
These results support the hypothesis that competing causes of death at earlier ages
lead to lower 30-day mortality among blacks for heart failure. They also maintain the
premise that socioeconomic status, support, and access factors are associated with
higher 30-day readmission rates for non-whites.
Consequently, unless race is taken into account, confounding (bias) may occur
in comparing risk-standardized, 30-day readmission for patients with AMI, heart
failure, and pneumonia and mortality rates for patients with heart failure.
Implications for Policy, Delivery, or Practice
The CMS Value-Based Purchasing (VBP) program bases reimbursement, in part, on
risk-standardized, 30-day mortality rates. The 30-day, risk-standardized readmission
rates, while not formally part of VBP, will impact hospital reimbursement.
Our study indicates that race, which currently is not taken into account in producing
the CMS risk-standardized rates, is a significant confounder that may result in unfair
hospital comparisons due to differential race distributions across hospitals.
This inequity could become a real financial problem for hospitals in the near future.
With the passage of the healthcare reform law (PPACA) in March 2010, Congress
gave CMS the authority to penalize hospitals for excess readmission rates starting
federal fiscal year (FFY) 2013. Initial efforts will focus on heart failure, AMI, and
pneumonia. Beginning FFY 2015, CMS may also begin withholding payments for
excessive readmissions related to chronic obstructive pulmonary disease, coronary
artery bypass grafts, percutaneous coronary interventions, and some vascular surgery
procedures.
Finally, this study also demonstrates the value that investigating discharge data can
provide to hospitals that are looking to better understand the implications of 30-day
mortality and readmission rate data. These data allow for more detailed comparisons.
1 Krumholz, HM, et al. “An Administrative Claims Model Suitable for Profiling Hospital Performance Based
on 30-Day Mortality Rates Among Patients with an Acute Myocardial Infarction.” Circulation. 2006; 113;
1683-1692.
2 Krumholz HM, et al. “An Administrative Claims Model Suitable for Profiling Hospital Performance Based
on 30-Day Mortality Rates Among Patients With Heart Failure.” Circulation. 2006; 113: 1693-1701.
For more information
Send us an email at
info@truvenhealth.com or
visit truvenhealth.com
ABOUT TRUVEN HEALTH ANALYTICS
Truven Health Analytics delivers unbiased information, analytic tools, benchmarks, and services to the healthcare industry. Hospitals, government agencies,
employers, health plans, clinicians, pharmaceutical, and medical device companies have relied on us for more than 30 years. We combine our deep clinical,
financial, and healthcare management expertise with innovative technology platforms and information assets to make healthcare better by collaborating with our
customers to uncover and realize opportunities for improving quality, efficiency, and outcomes. With more than 2,000 employees globally, we have major offices
in Ann Arbor, Mich.; Chicago; and Denver. Advantage Suite, Micromedex, ActionOI, MarketScan, and 100 Top Hospitals are registered trademarks or trademarks of
Truven Health Analytics.
truvenhealth.com
|
1.800.366.7526
©2012 Truven Health Analytics Inc. All rights reserved. All other product names used herein are trademarks of their respective owners. MDS 11365 0712