URINARY SYSTEM Dr.Firdous
advertisement

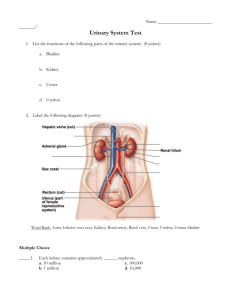
URINARY SYSTEM Dr.Firdous The urinary system consists of paired kidneys, ureters, and a single bladder and urethra. Function: 1. Maintenance of homeostasis by production of urine through filtration, absorption, and secretion. 2. Regulation of fluid and electrolytes balance of the body. 3. Production of Renin (important in regulation of blood pressure). 4. Production of Erythropoietin (stimulates the production of erythrocytes). KIDNEY The kidney is about 11cm, 6cm, 3cm in dimensions. Each kidney weights about 150 gm. It has a concave medial border; the hilum, where the nerves enter, blood and lymphatic vessels enter and leave, and the ureter exits, and a lateral convex side. Each kidney is surrounded by a connective tissue capsule that is surrounded by a mass of peri renal adipose tissue. The capsule consists of two distinct layers; an outer layer of fibroblasts and collagen fibers, and an inner layer of myofibroblasts. The capsule pass inward at the hilum covering the sinus, and become continuous with the connective tissue forming the walls of calyces and renal pelvis. The kidney is divided into an outer cortex and an inner medulla. Renal medulla consists of 10-18 conical or pyramidal structures; the medullary pyramids, whose bases form the cortico-medullary junction and vertices protrude into the minor calyces. The tips of pyramids are called renal papillae, where the collecting ducts open into. From the base of each medullary pyramids parallel tubules; the medullary rays, penetrate the cortex. Kidney lobe consists of medullary pyramid and associated cortical tissue at its base and sides, and they are about 8-18 in each kidney. Renal pelvis is the dilated upper portion of the ureter which is divided into 2-3 major calyces that branch into several smaller minor calyces. 1 NEPHRON It is the functional unit of the kidney. There are about 1-4 millions in each kidney. Each nephron consists of a dilated portion; the renal corpuscle, proximal convoluted tubule (PCT), thin and thick limbs of Henle's loop, and distal convoluted tubule (DCT). Some investigators consider the collecting tubules and ducts to be part of the nephron. RENAL CORPUSCLE It is about 200 µ in diameter, and consists of a tuft of capillaries; the glomerulus, and a double-walled epithelial capsule; glomerular(Bowman's capsule). Renal corpuscle has a vascular pole, where afferent arteriole enter, and efferent arteriole leave, and a urinary pole where the PCT begins. Glomerulus: When afferent arteriole enter the renal corpuscle, it will divide into 2-5 primary branches which will further divide into capillaries forming the glomerulus. The endothelial cells have thin cytoplasm except around the nucleus. It is of the fenestrated type with 70-90 nm in diameter, with no diaphragm. Bowman's capsule Composed of two layers; parietal and visceral, with a space in between called urinary space which receives the fluid filtered through capillary wall. Parietal layer consists of simple sequamus epithelium supported by a basal lamina and a thin reticular fibers. At the urinary pole, this epithelium will change into simple cuboidal epithelium of the PCT. Visceral layer is modified during embryonic life and the cells are called Podocytes. The cell body gives rise to several primary processes from which arise numerous secondary processes that called pedicels. These pedicels embrace the capillary of glomerulus and come in contact with the basal lamina at a periodic distance of 25nm. The pedicels interdigitate with each other defining a space about 25nm wide; the filtration slit which is bridged by a diaphragm of 6nm thick. Podocytes have bundles of actin microfilaments to give them the contractile capacity. A thick basement membrane (0.1µm) is formed by fusion of the basal laminae of both capillary and podocytes, forming a filtration barrier that separates urinary space and capillary blood. By E.M,the basement membrane consist of a central electron-dense layer called lamina densa, and, on each sides, a more lucent layer called lamina rara which contains fibronectin to bind them to the cells. Lamina densa contains typeIV collagen. The filtration apparatus(barrier) consists of: 1- Endothelium of glomerular capillaries: they are fenestrated, with no diaphragm, and posse a large number of aquaporin-1(AQP-1) water channels that allow fast movement of water through epithelium. 2 2- Glomerular basement membrane. 3- Podocytes. In diseases such as diabetes mellitus and glomerulonephritis, the glomerular filter is altered and becomes much more permeable to proteins, with the subsequent release of protein into the urine (proteinuria). Mesangial cell: This cell is found adherent to the wall of glomerular capillaries where the basal lamina is shared by two or more capillaries. It has cytoplasmic processes that extend to the endothelial cells. They have receptors for angiotensin II. When these receptors are activated, the glomerular flow is reduced. Mesangial cells also have receptors for the natriuretic factor produced by cardiac atria cells. This factor is a vasodilator that relaxes the mesangial cells, probably increasing the blood flow and the effective surface area available for filtration. Mesangial cells also have several other functions: they give structural support to the glomerulus, synthesize extracellular matrix, endocytose and dispose of normal and pathological (immune complex) molecules trapped in the glomerular basement membrane, and probably produce chemical mediators such as cytokines,prostaglandins, interleukin-1, and platelet-derived growth factor(PDGF) In certain diseases of the kidney it has been noticed that mesngeal cells proliferate, in which abnormal amount of proteins trapped in the basement membrane. Although mesangeal cells act as macrophages, embryologically they originate from smooth muscle cell precursors, rather than the precursors of mononuclear phagocytic system. PROXIMAL CONVOLUTED TUBULE(PCT) Begins at the urinary pole of the renal corpuscle, where the simple sequamus epithelium change into simple cuboidal or simple columnar epithelium. This tube is long and tortuous so it is more frequently seen in renal cortex than DCT. The cytoplasm is acidophilic due to the presence of numerous mitochondria. The cell apex has abundant microvilli, of 1µm in length, and they form the brush border. Each cell has a spherical, centrally located nucleus. In living animal PCT has wide lumen, but in histological section the lumen is collapsed and the brush border is disorganized. The apical cytoplasm has numerous canaliculi between the bases of microvilli. They are important in absorbing macromolecules. The basal portion of PCT has membrane invaginations and the mitochondria are concentrated at the bases of these cells parallel to the long axis of the cell. These are the characteristics of ion transporting cells. There is an extensive interdigitations of the lateral membrane of adjacent cells, so there is no discrete cell margins when observed by L.M. Cells of PCT are large, so they appear only 3-5 nuclei in transverse section. 3 HENLE'S LOOP It is a U shaped structure consist of thick and thin descending limbs, thin and thick ascending limbs. It starts as a thick limb in the outer medulla with a diameter of 60µm, lined by simple cuboidal epith. , then suddenly narrows to about 12µm in diameter as the thin descending limb. This segment has a wide lumen, and lined by simple seq.epith., whose nuclei protrude slightly into the lumen. This segment runs deep into the medulla, then continues upwards as the ascending thin limb, which will suddenly change into simple cuboidal epith. of the thick ascending limb. Most of nephrons are cortical, and they have very short thin descending limb with no thin ascending limb. Few number of nephrons are located near the corticomedullary junction and called juxtamedullary nephrons. They have very long Henle's loop. Juxtamedullary nephrons are important in producing concentrated urine. Intermediate or midcortical nephrons have their corpuscles in the mid region of cortex, and their loop of Henle is of the intermediate length. DISTAL CONVOLUTED TUBULE(dct) It is the continuation of the thick ascending limb of Henle's loop, when it penetrates the cortex. It is tortuous and lined by simple cuboidal epith. The cells of DCT are small and flat, so more nuclei are seen in histological section. The cells lack brush border or apical canaliculi and they appear less acidophilic than the cells of PCT. Their lumen is wide. Lateral boundaries between adjacent cells are not seen by L.M due to the interdigitations between these cells. Like cells of PCT, the cells of DCT have numerous basal membrane invaginations with large number of mitochondria. When DCT come in contact with the afferent arteriole of its parent nephron, its cells will be modified. They will become columnar and their nuclei are closely packed together, with the Golgi complex at the basal region. This modified area of the DCT appears darker in L.M. and called macula densa, which is sensitive to ionic contents and volume of tubular fluid. Juxtaglomerular apparatus: Tunica media of afferent arteriole of the renal corpuscle will be modified and called juxtaglomerular cells(J.G.C.) . The nucleus is spherical, the internal elastic membrane will disappear, and the cytoplasm is full of secretary granules. By E.M., J.G.C. show characteristics of protein-secreting cells; abundant RER, highly developed Golgi complex, and the presence of secretary granules of 10-40 nm in diameter. Macula densa of the DCT is usually located close to the J.G.C. Together,they form the J.G.apparatus. J.G.C. produce renin which act on a plasma protein; angiotensinogen, to produce an inactive angiotensin Ι, which will be converted into angiotensinΙΙ by a converting enzyme. Part of the J.G.apparatus are some light-staining cells whose function is not well understood, called extraglomerular mesangeal cells or Lacis cells. After a significant hemorrhage (decreased blood volume promotes a decreased blood pressure), there is an increase in renin secretion. Angiotensin II is produced, 4 enhancing blood pressure by both constricting arterioles and stimulating the secretion of the adrenocortical hormone aldosterone. Aldosterone acts on cells of the renal tubules (mostly the distal tubules) to increase the absorption of sodium and chloride ions from the glomerular filtrate. This increase in sodium and chloride ions, in turn, expands the fluid volume (particularly blood plasma volume), leading to an increase in blood pressure due to increased blood volume. Decreased blood pressure caused by other factors (eg, sodium depletion, dehydration) that decrease blood volume also activates the renin “ angiotensin II“ aldosterone mechanism that contributes to the maintenance of blood pressure. Aldosterone deficiency in adrenalectomized animals and in humans with Addison disease results in an excessive loss of sodium in the urine. COLLECTING TUBULES AND DUCTS DCT will open into a straight collecting tubules in the medullary rays. They lie side by side and make up most of the pyramids. Collecting tubules are lined by simple cuboidal epith., with a diameter of 40µm. these tubules join each other forming a larger straight collecting ducts, which widen gradually as they approach the tips of pyramids. The lining epith. of collecting ducts is simple columnar epith., with a diameter of 200µm. The cells of both tubules and ducts are lightly stained, with few organellls in their cytoplasm. There is no basal invagination, or lateral membrane interdigitations, so the intercellular limits are clearly seen. The epith. of collecting duct is under the control of the anti-diuretic hormone(ADH) There are two types of cells in collecting tubules and ducts: 1- Light cells: pale staining cells with basal infoldings, single apical cilium and few microvilli. The cytoplasm contains small spherical mitochondria. 2- Dark cells( intercalated cells): They are fewer in number, and appear denser, and their cytoplasm contains many mitochondria. Their apical cytoplasm contains microvilli and vesicles. They don’t show basal infoldings, but have basal interdigitations with neighboring cells. Dark cells gradually decrease in number as the collecting duct approach the papilla. Blood circulation of the kidney Renal artery will enter the kidney through the hilum, and divide into two branches; one supplies the anterior part, the other supplies the posterior part of the kidney. An inter -lobar artery will run between the medullary pyramids. At the cortico-medullary junction, inter lobar artery forms the arcuate artery, from which arise the interlobular arteries at right angle to the renal capsule. From inter lobular arteries, arise the afferent arterioles which supply the glomerular capillaries, then blood goes to the efferent arterioles which branch to give the peritubular capillary net work, to supply PCT and DCT. The efferent arterioles which are associated with juxta-medullary nephrons are long and thin capillaries and they follow a 5 straight path into the medulla, then loop back towards the cortico-medullary boundaries and called vasa recta. The descending vessel is continuous, while the assending one is fenestrated. These capillaries are important in the nourishment of medulla. Capillaries from outer cortex and capsule converge to form the stellate veins that empty into the interlobular vein. Veins follow the same course of arteries in a reverse way. Renal interstitium It represents the space between tubules, blood, and lymph vessels. It is little in the cortex, but increase in the medulla. It consists of small amount of connective tissue, collagen fibers, ground substance, and secreting cells; the interstitial cells. There are two types of cortical interstitial cells; fibroblasts and macrophages. Fibroblasts are found in between tubules and capillaries, and they synthesize and secrete collagen and glycosaminoglycans of the extracellular matrix of the interstitium. In the medulla, the principle interstitial cells resemble myofibroblasts. Their cytoplasm contains abundant actin filaments, abundant RER, well developed Golgi complex, and lysosomes. Some evidence suggests that these cells may secrete a hormone-like material that reduces blood pressure. Prostaglandins and prostacyclin may also been synthesized in the interstitium. URINARY BLADER It stores the urine temporarily, before its exsecretion to the outside. The wall of the bladder consists of three layers: 1-Mucosa: It is the inner layer, composed of transitional epith. and lamina propria. In an empty bladder, the transitional epith. is 5-6 cells in thickness, the superficial cells are rounded and bulge into the lumen, and they are usually polypoid or binucleated. When bladder is full of urine, the epith. will stretch and cells will become 3-4 only in thickness and the superficial cells become sequamous. The bladder contains three orifices; two upper ureteric orifices, and one lower internal urethral orifice. The triangular region defined by these three orifices is called trigone, is smooth and has constant thickness, while the rest of the wall of bladder has variable texture and thickness in relation to the fullness of bladder. The trigone originates embryologically from mesonephric ducts, while the rest of bladder wall originates from cloaca. 6 The superficial cells of the transitional epithelium have a special membrane of thick plates separated by narrow bands of thinner membrane that are responsible for the osmotic barrier between urine and tissue fluids. When bladder contracts, the membrane folds along the thinner regions, and the thicker plates invaginate to form cytoplasmic vesicles. These vesicles represent a reservoir of these thick plates that can be stored in the cytoplasm of the cells of the empty bladder and used to cover the increased cell surface in the full bladder. Lamina propria consists of loose connective tissue and diffuse lymphoid tissue. 2-Muscular layer: Thick layer that runs in every direction, without distinct orientation. At the bladder neck(origin of urethra), the muscular layer will arrange in three layers: a- Inner longitudinal layer: it will become circular distal to the bladder neck and surrounds the prostatic urethra in the male, and external meatus of the female, forming the true involuntary urethral sphincter. b- Middle circular layer: it ends at the bladder neck. c- Outer longitudinal layer: continues to the end of the prostate in male, and the external urethral meatus in female. 3- Adventitia: Loose connective tissue rich in blood vessels, except the upper part of the bladder which is covered by serosa(because it is an intra peritoneal part). URETER Renal calyces, renal pelvis, and ureters have the same histological structure. The wall consists of three layers: 1- Mucosa: similar to that of the urinary bladder. 2- Muscular layer: it has a helical arrangement, then near the bladder, it will become two layers; an inner longitudinal and outer circular. When the ureter pass through the wall of the bladder, the muscles will become longitudinal only. The ureter pass obliquely through the bladder forming a valve to prevent the back-flow of urine. In addition, there is a flap of bladder mucosal membrane act as a valve. 3- Adventitia: loose connective tissue. URETHRA It is a tube that carries urine to the outside. Male urethra It is divided into three parts: 1- Prostatic urethra: represents the initial part, surrounded by the prostate gland, very close to the bladder. In the dorsal and distal part, there is an elevation; 7 verumontanum, that protrudes into the interior. The two ejaculatory ducts open on the sides of the verumontanum, in addition to the prostatic glands. Seminal fluid enter through these ducts to be stored before ejaculation. Prostatic urethra is lined by transitional epith. 2- Membranous urethra: about 1cm long, extends from prostatic urethra to the bulb of corpora cavernosa. It is lined by stratified or pseudostratified columnar epith., and surrounded by striated muscle; the voluntary urethral sphincter. 3- Penile urethra: include both bulbous and pendulous urethra. Both extend through the corpus spongiosum of the penis. They are lined by pseudostratified columnar epith., or columnar epith. At the distal part, the lumen of urethra dilates forming fossa navicularis, which is lined by stratified sequamous epith. The lamina propria of the urethra is composed of loose connective tissue rich in blood vessels and mucous glands; Littre's gland(mostly at the pendulous part). Female urethra Short tube; about 4-5cm long, lined by pseudostratified epith., and near the external orifice, it becomes stratified sequamous epith. The middle portion is surrounded by the external voluntary sphincter. 8