outline31095
advertisement
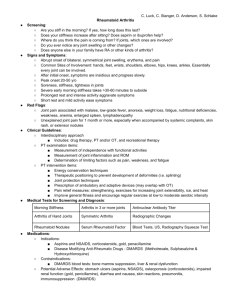
TITLE: A Tale of White Spots ABSTRACT: This case documents a progressive retinal micro-angiopathy caused by systemic methotrexate toxicity induced pancytopenia. Prompt work up and communication with the prescribing physician is imperative to save lives. I. Case History a. 52 y/o White female b. No complaints – routine exam c. Last eye exam: 1 year prior – glasses d. Systemic history/meds: 12.5 mg/week oral methotrexate for rheumatoid arthritis x 11 years; 1 mg/d folic acid supplementation e. Denies smoking, drinking or drug use II. Pertinent Findings a. Clinical 1. Best corrected VA 20/20 O.D., O.S. 2. Pupils, EOM’s, Confrontation VF’s - WNL OD, OS 3. Slit lamp OU – normal findings 4. Goldmann IOP: 14mm Hg OD, 15 mmHg OS 5. Blood pressure: 110/60 mmHg 6. DFE: 1. Single cotton wool spot O.S. 2. Healthy optic nerves 7. Denies weakness, fatigue, sudden weight loss, paresis or paresthesias. Denies risk for sexually transmitted diseases b. Contacted rheumatologist and patient referred for laboratory work-up c. Initial laboratory work-up ordered 1. CBC with differential, ESR, CRP, RF, FBS, HgBA1c, HIV antibody, lipid panel, lupus panel. d. Ocular Follow-up 2 weeks later 1. No visual complaints 2. Patient did NOT get blood work yet (missed appointment) 3. BCVA 20/20 O.D., O.S. 4. Entrance/anterior seg findings all normal 5. DFE: 1. Multiple cotton wool spots both eyes 2. Healthy optic nerves O.U. 6. Blood work obtained same day and results (to be presented after DDX) 1. White blood cell, red blood cell, hemoglobin, hematocrit and platelet counts at critically low levels 2. Neutrophils, lymphocytes and monocytes – low 3. ESR – critically high level 4. CRP - high 5. HIV antibody negative 6. Glucose, HgBA1c, lipid panel, lupus panel – normal/negative 7. Lab contacted myself and rheumatologist same day to admit patient to hospital due to critical results of blood cells. Patient was admitted the same day and had hematologist consult. e. Further lab tests (ordered by rheumatologist) 1. Liver panel – normal III. Differential Diagnosis a. b. c. d. IV. Blood dyscrasia retinopathy Diabetic retinopathy HIV retinopathy Lupus/autoimmune retinopathy Diagnosis and Discussion: a. Diagnosis: 1. Progressive, retinal micro-angiopathy secondary to pancytopenia from systemic methotrexate toxicity b. Rheumatoid Arthritis (RA) 1. Chronic, progressive autoimmune inflammatory disorder 2. Primarily results in joint destruction but may also affect other organs. 3. Current approach to RA therapy = early, more aggressive treatment with disease-modifying anti-rheumatic drugs such as methotrexate c. Methotrexate 1. Folic acid antagonist used in treatment of variety of inflammatory disorders and cancers 2. Low dose (5-30mg/week) – reduces joint damage by decreasing disease activity and enhances effects of other therapies – has become treatment of choice for many RA patients. 3. Side effects: 1. Mild: gastro-intestinal irritation, alopecia, skin rash, stomatitis oral ulcers 2. Severe/life threatening: pancytopenia, myelosuppression, hepatotoxicity and pulmonary complications 4. Because of potential life-threatening complications associated with methotrexate therapy, patients are monitored with blood work every 1-3 months by their prescribing physician. (this patient had actually missed her most recent follow-up with her rheumatologist, but had never had abnormal blood work in past 11 years of therapy prior to this episode). d. Pancytopenia 1. Potentially fatal complication 2. Reduction of all 3 cellular components found in blood: white blood cells, red blood cells, platelets 3. ~1-1.5% patients on low dose methotrexate 4. Sudden without warning signs 5. Most within 10 days of starting therapy – late reactions have been reported 6. Mechanism unknown 7. Associations: bone marrow suppression especially in kidney insufficiency, hypoalbuminemia, low folate levels, concomitant infections, use of more than 5 medications and lack of folate supplementation (this patient had none of these) e. Ocular effects in methotrexate therapy 1. RARE 2. Usually in patients receiving high dose, intravenous therapy (30250mg/kg) 3. Periorbital edema, ocular pain, blurred vision, photophobia, conjunctivitis, blepharitis and decreased reflex tear secretion 4. Isolated reports: optic neuropathy and internuclear ophthalmoplegia, macular edema, epiphora, lacrimal duct stenosis and optic nerve demyelination; but, concomitant other anti-cancer medications were also used. f. Cotton wool spots 1. Acute, focal, inner-retinal ischemia caused by occlusion of pre-arteriolar capillary network in retina 2. Transient, non-specific finding 3. Common in diabetes, hypertension and vein occlusions 4. When these causes are excluded, serious systemic disease can be found in 95% of cases. 5. Additional causes include blood dyscrasia, autoimmune etiologies, and other immunosuppressant medications (interferon alpha and beta) 6. In this case, cotton wool spots could be due to immunologic or hematologic disorders. 1. Immunologic less likely: rarely, systemic vasculitis in RA could result in vaso-occlusive disease; most cases described are with anterior ischemic optic neuropathy. 2. Hematologic most likely: may be linked to decreased hemoglobin and hematocrit levels < 50% of normal 7. Although RA can’t be ruled out as the cause of cotton wool spots, the progressive nature of the ischemic lesions, as well as their resolution with decreased methotrexate therapy, makes it unlikely. 8. Cotton wool spots in this case most likely a consequence of blood dyscrasia (pancytopenia), which was induced by methotrexate. V. Treatment/Management a. Tapering of methotrexate by hematologist and rheumatologist to 5mg/wk over 3 months resulted in normalized blood work and resolution of cotton wool spots. VI. Conclusion a. Methotrexate induced pancytopenia can be fatal b. Patients taking methotrexate and presenting with ischemic retinal findings warrant investigation for pancytopenia c. Thorough history, prompt work-up and communication with the prescribing physician may be life saving. VII. Bibliography 1.Ward JR. Historical perspective on the use of methotrexate for the treatment of rheumatoid arthritis. J Rheumatol. 1985;12:3–6. 2.Chan ESL, Cronstein BN. Molecular action of methotrexate in inflammatory diseases. Arthritis Res. 2002;4(4):266–273 3.Dalrymple JM, Stamp LK, O'Donnell JL, et al. Pharmacokinetics of oral methotrexate in patients with rheumatoid arthritis. Arthritis Rheum. 2008;56(11):3299–3308 4.Prey S, Paul C. Effect of folic or folinic acid supplementation on methotrexate-associated safety and efficacy in inflammatory disease: a systematic review. Br J Dermatol. 2009;160:622– 628. 5.Endresen GK, Husby G. Folate supplementation during methotrexate treatment of patients with rheumatoid arthritis. Scand J Rheumatol. 2001;30:129–134. 6.Jabs DA, Rosenbaum JT, Foster CS, et al. Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol. 2000;130(4):492–513. 7.Lustig MJ, Cunningham ET. Use of immunosuppressive agents in uveitis. Curr Opin Ophthalmol. 2003;14:399–412. 8.Felly MG, Erickson A, O'Dell JR. Therapeutic options for rheumatoid arthritis. Exp Opin Pharmacother. 2009;10(13):2095–2105. 9.Visser K, Katchamart W, Loza E, et al. Multinational evidence-based recommendations for the use of methotrexate in rheumatic disorders with a focus on rheumatoid arthritis: integrating systematic literature research and expert opinion of a broad international panel of rheumatologists in the 3E initiative. Ann Rheum Dis Epub 25 Nov 2008. Available at: http://ard.bmj.com. Last accessed February 17, 2009. 10.Sizova L. Approaches to the treatment of early rheumatoid arthritis with disease-modifying antirheumatic drugs. Br J Clin Pharmacol. 2008;66(2):173–178. 11.Salliot C, van der Heijde D. Long term safety of methotrexate monotherpay in rheumatoid arthritis patients: a systematic literature research. Ann Rheum Dis Epub 5 Dec 2008. Available at: http://ard.bmj.com. Last accessed February 17, 2009. 12.Hocaoglu N, Atilla R, Onen F, et al. Early-onset pancytopenia and skin ulcer following lowdose methotrexate therapy. Hum Exp Toxicol. 2008;27:585–589. 13.Grove ML, Hassell AB, Hay EM, et al. Adverse reactions to disease-modifying antirheumatic drugs in clinical practice. Q J Med. 2001;94:309–319. 14.Calvo-Romero JM. Severe pancytopenia associated with low-dose methotrexate therapy for rheumatoid arthritis. Ann Pharmacother. 2001;35:1575–1577. 15.Gutierrez-Urena S, Molina JF, Garcia CO, et al. Pancytopenia secondary to methotrexate therapy in rheumatoid arthritis. Arthritis Rheum. 1996;39(2):272–276. 16.Arevalo FJ, Lowder CY, Muci-Mendoza R. Ocular manifestations of systemic lupus erythematosus. Curr Opin Ophthalmol. 2002;13:404–410. 17.Schmid KE, Kornek GV, Scheithauer W. Update on ocular complications of systemic cancer chemotherapy. Survey of Ophthalmology. 2006;51(1):19–40. 18.Golnik KC, Schaible ER. Folate-responsive optic neuropathy. J Neuro-Ophthalmol. 1994;14(3):163–169. 19.Balachandran C, McCluskey PJ, Champion GD, et al. Methotrexate-induced optic neuropathy. Clin Exp Ophthalmol. 2002;30:440–441. 20.Wilson R. Cotton wool spots in AIDS: a review. J Am Optom Assoc. 1994;65:110–116. 21.Ho AC, Brown GC, McNamara A, et al. Retina: Color atlas & synopsis of clinical ophthalmology Wills Eye Hospital. Madrid: McGraw-Hill; 2003;76-77. 22.Aristodemou P, Standford M. Therapy insight: the recognition and treatment of retina manifestations of systemic vasculitis. Nat Clin Pract Rheumatol. 2006;2(8):443–451. 23.Chen YH, Wang AG, Lin YC, et al. Optic neuritis as the first manifestation of rheumatoid arthritis. J Neuro-Ophthalmol. 2008;28(3):237. 24.Hamilton P, Gregson R, Fish GE. Text atlas of the retina: blood dyscrasias. UK: Martin Dunitz; 1998;355. 25.Moon SJ, Mieler WF. Retinal complications of bone marrow and solid organ transplantation. Curr Opin Ophthalmol. 2003;14:433–442. 26.Alexander LJ. Primary care of the posterior segment, Second ed. New York: McGraw-Hill; 1994;186-188. 27.Longmuir R, Lee AG, Rouleau J. Cotton wool spots associated with interferon beta-1 alpha therapy. Sem Ophthalmol. 2007;22:49–53. 28.Schulman JA, Liang C, Kooragayala LM, et al. Posterior segment complications in patients with hepatitis C treated with interferon and ribavirin. Ophthalmology. 2003;110(2):437–442