Grand Rounds 4/1/13 The internist as diagnostician – Clinical Pearls
advertisement

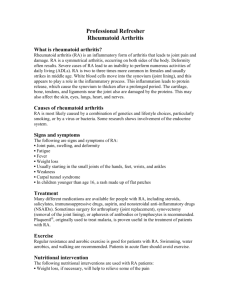
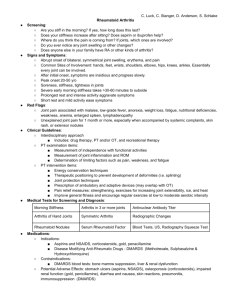
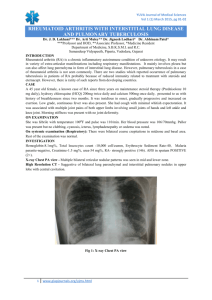
Grand Rounds 4/1/13 The internist as diagnostician – Clinical Pearls from Four Cases 1. 2. 3. 4. Pituitary tumor Myasthenia gravis Rheumatoid arthritis Genetics of hemochromatosis Learning Objectives: Understand the important role of the internist as diagnostician. Recognize common symptoms which may represent uncommon diseases Appreciate that certain genetic tests may be useful in the primary care setting. Recognize symptoms of pituitary tumors 2/15 Night sweat, hot flashes, and back pain for one month. Nausea improved. White nipple discharge for several months. Normal breast exam Fsh 0.7 (1.5- __) LH <.1 HCG – Progestoerone <.2 Estrodiol<10 Testosterone<12 DHEA 28 – nl Prolactin -47.2 (2.8-29.2) PMH: TBI secondary to skull fx in hs dropped while cheerleading Chicken pox F A&w M – kidney problems Sister – 26 a& w MRI- sellar and suprasellar mass enhancing intensely with gadoliminum.3.2 x 1.7 x 2.1 with waist at sellar diaphragm elevating optic chiasm Labs 4/10 FHS 7.3 LH 2.8 PRL 12.8 TSH 1.61 Prog .3 Estradiol <20 Testosterone 7 12/12 Abdom discomfort, nausea/vomiting since 8/22. Most days. Unimproved by ranitidine. Vomiting 1-2 times each morning. No improvement with stopping OCP or using acidiphilus. Nl BMs, apetite. 15 pound weight loss. Mild abdom discomfort with eating larger meals. Vomitus generally clear to yellow. Infrequently blood tinged. No history of eating disorder. Denied other symptoms suggesting eating disorder. Unrelated to type of food. Denied any chemical exposures. Denied anxiety. Transferring back to ETSU due to symptoms. p-83 BP 102/68 BMI 22 Wt 105 Gen – well developed,normal HEENT - nl Ht – nl Lungs –nl Abd – nl Neuro – nl MS – nl Psych – nl Lymph – nl TSH, HCG, Abd u/S UGI, CBc, CMP Metoclopramide UGI – mod reflux to upper esophagus u/s - 2 mm gb polyp, ? left renal stone CBC – nl CMP – nl TSH – nl HCG 2wks later – no response to metoclopramide but responded well to Phenergan once per day. Trial of omeprazole Denied alcohol tobacco or drugs 10/12 AM nausea most days, within 2 hrs of awakening and before eating. Stopped OCP but symptoms persisted. No other GI sx. Felt to be GERD and place on ranitidine. 7/12 19yo GO started on oral contraceptive 4/11 to regulate irregular menses. Started on LoEstrin which initially helped and then began to have breakthrough bleeding. Stress related to starting college at UT and boyfriend being in Tri-Cities area. Tired on higher dose estrogen pill. 4/11 17 yo GO. Amenorhea for 1.5 yrs after having periods. Advised that likely due to PCOS sarted on LoEstrin Was on OCP for 4-5 months and had menses regularly during that time. Stopped for unclear reasons Menarche age 13. Had regular periods for two years then abruptly stopped at age 15. Reportedly had hormone levels checked and normal. (LH, FSH, prolactin, estradiol, estrogen). Pelvic ultrasound all normal. Colnsiderd PCOS anovulatory cycles. No STI. Not sexually active. Complete ROS in 4/11 negative. September OA RA 67 yo m 13 yr history of episodes of intermittent joint pain, bilateral . Shoulders elbows wrists ankles, Freq one per month. No obvious precipitants. Worse over 6 months. WBC 4.1, plt 91. RA 25 (<20) ANA 1:40, Lyme neg, CMP, TSH, uric acid normal. Redness, warmth, and swelling increased to 1-2 /wk. PMH: CAD, lipid Nonsmoker, alcohol 1/day. Attorney Exam initlal nl except wrists warm and should crepitius. – nodes, ht lung abd Iniital impression intermittene inflammatory polyarthritis with borderlin post ANA & RA with leukopenian dthrombpcytopenei. Melox CRP 7.7 (<5) ESR 16 RA 14 (<10) WBC 2.8 (53% lymp, 30% polys, 17% mono HGB 15.3 (MCV 87) Plt 96 ANA 57 (nl) Symptoms completely controlled with meloxicam. New adenopathy neck – squamous cell of undefined primary. Surg Rad biologic tx, CT abd splenomeg 8 mos after initial presentation. Hand swelling. RA 17, ESR 28, 3 wk hx hands increased swelling Spleen 14 x 14 x 6.5 Felty’s syndrome Infrequent but severe form of RA – RA, splenomegaly, neutropenia Usually RA appears 10 yrs beofroe nurtorpenia recognized Infrequently neutropenia and splenomegaly before or at onset of RA sx Women 60-80%, onset 30s-40s. RA usually severe More frequejnt and sever extraarticular manifestaitons DDX RA OA Psoriatic Crystalline Psoriatic 1987 American College of Rheumatology (formerly American Rheumatism Association) revised classification criteria for rheumatoid arthritis Criterion Description Morning stiffness Morning stiffness in and around the joints, lasting at least one hour before maximal improvement. Arthritis of 3 or more joint areas At least 3 joint areas (out of 14 possible areas; right or left PIP, MCP, wrist, elbow, knee, ankle, MTP joints) simultaneously have had soft- tissue swelling or fluid (not bony overgrowth alone) as observed by a physician. Arthritis of hand joints At least one area swollen (as defined above) in a wrist, MCP, or PIP joint. Symmetric arthritis Simultaneous involvement of the same joint areas (as defined above) on both sides of the body (bilateral involvement of PIPs, MCPs, or MTPs, without absolute symmetry is acceptable). Rheumatoid nodules Subcutaneous nodules over bony prominences or extensor surfaces, or in juxta-articular regions as observed by a physician. Serum rheumatoid factor Demonstration of abnormal amounts of serum rheumatoid factor by any method for which the result has been positive in less than 5 percent of normal control subjects. Radiographic changes Radiographic changes typical of rheumatoid arthritis on posteroanterior hand or wrist radiographs, which must include erosions or unequivocal bony decalcification localised in, or most marked adjacent to, the involved joints (osteoarthritis changes alone do not qualify). Note: For classification purposes, a patient has RA if at least four of these criteria are satisfied (the first four must have been present for at least six weeks). Nails Myasthenia 65 yo m 2 mo his difficulty with speech slurring. Dysarthrai with eating. Difficulty swallowing. Sx cleared with stopping. No diplopia, drooping of eyelids. No weakness of extrem. No pain numbness tingling. No hoarseness, odynophagia, tong swelling. Ach Ab pos. CT chest - no thymus seen. Mestinon 30 tid plus azathio 50 qid. Exam tongue weakness with speaking or chewing. SCC well diff forehead OSA Spinal stenosis 2 to OA and DJD Myasthen HTN DM MO Venous insuff Tob never Wine 6/wk AZAthioprine 50 mg tid Mestinon 60 qid Slurred speech Dysrthria Difficulty chewing