MCQs in Rheumatology: Miscellaneous conditions
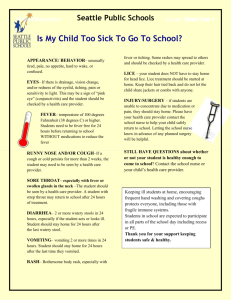
advertisement

MCQs in Rheumatology: Miscellaneous conditions Contributors: These MCQs were written by Dr Fran Rees, Dr Kar-Ping Kuet and Dr Michelle Hui; and were reviewed by Dr Neal Hopkinson, Dr Marian Regan, Prof Andy Hassell, and Prof Nigel Arden. The MCQs were edited by Dr A Abhishek who also facilitated the review process. www.rheumatology.org.uk/education Question 1 A 19-year old man presents with acute swelling of both ankles. On examination, there is positive stress test (pain at extreme movements) at the tibiotalar and subtalar joints with pitting oedema of the shins associated with painful raised red patches. What is the most appropriate investigation? 1. 2. 3. 4. 5. Aspiration of ankles Chest x-ray Skin biopsy Urethral swab X-ray of ankles Question 2 A four year old child is referred to accident and emergency unwell with fever and not feeding for 5 days. On examination he has fever of 40°C, BP of 140/90, HR 100 bpm, RR 20/min. He has palpable cervical lymph nodes, a red tongue and a truncal rash with desquamation of the hands and feet. What is the most likely diagnosis? 1. 2. 3. 4. 5. Infectious mononucleosis Kawasaki disease Measles Parvovirus infection Systemic lupus erythematosus Question 3 A 60-year-old man is admitted with fever, arthralgia and rash. He has been generally unwell for past 2 weeks. On examination, his temperature is 38.2 oC. He has tender, erythematous plaques over his hands, arms and legs. There is no synovitis. Investigations show a neutrophilia (15x109/l), a raised C-reactive protein (89mg/L), and a punch biopsy of the lesion shows neutrophilic infiltration of the dermis. What is the initial treatment of choice? 1. Colchicine 2. Dapsone 3. Ibuprofen 4. Indomethacin 5. Prednisolone www.rheumatology.org.uk/education Question 4 A 19-year-old Greek man presents with an 8 week history of intermittent attacks of left sided chest pain and fever. During the attacks he is unable to deep breathe or lie flat. His temperature has been recorded up to 39 degrees. In addition, he has developed generalised arthralgia and has noticed intermittent swelling of his right knee. On examination, temperature is 37.8 degrees. He has a left-sided pleural rub and a swollen right knee, which is aspirated. Initial investigations Joint aspirate No organisms, no crystals. C-reactive protein 110mg/L Hb 13.5g/dL WCC 19.8x109/l Plts 175 x109/l Blood cultures negative Which gene is most likely to be mutated? 1. CIASI 2. CINCA 3. MEFV 4. MVK 5. TNFRFSFIA Question 5 A 55 year old man with long standing Rheumatoid arthritis, and bronchiectasis, is seen in clinic with weakness, fatigue, weight loss and diarrhoea. He is currently taking Methotrexate 15mg weekly. He has recently been diagnosed with heart failure, and has developed peripheral neuropathy over the last few years. He has hepato-splenomegaly, and the urine dipstick in clinic shows 2+ proteinuria. Recent blood tests show a normal FBC, U&E. The CRP and ESR are 12 mg/l and 65 mm/hr. The serum albumin is 27g/l (35-55), and total protein is 90g/l (60-84). Which of the following investigations would you choose next? 1. 2. 3. 4. 5. Abdominal subcutaneous fat biopsy Liver biopsy Rectal biopsy Radiolabelled- SAP scan Stool sample www.rheumatology.org.uk/education Question 6 An 18 year old Turkish man presents with an 8 week history of intermittent fevers associated with severe abdominal pain. He has generalised arthralgia and has noticed a rash on his legs. On examination, the temperature is 37.8 oC. His abdomen is soft, but there is generalised tenderness. He has a swollen right knee, which is aspirated. He has a confluent erythematous macular rash on his legs. Joint aspirate No organisms, no crystals. What is the most useful long-term treatment? 1. 2. 3. 4. 5. Colchicine Methotrexate Naproxen Prednisolone Sulfasalazine Question 7 A 72 year old man with long standing Rheumatoid arthritis is seen in clinic with weakness, fatigue, weight loss and diarrhoea. He is currently taking Methotrexate 15mg weekly. On examination he has hepato-splenomegaly and peripheral oedema. Initial investigations Hb 10.5g/dL WCC 4.3 x109/l Plts 135 x109/l MCV 100fL U&E and LFTs normal. Urine dipstick Protein 3+ , Blood Albumin 27g/L (35-55) Total protein 90g/L (60-84). Serum electrophoresis no free light chains. What is the most likely diagnosis? 1. 2. 3. 4. 5. Amyloidosis Felty’s syndrome Methotrexate toxicity Neuroendocrine tumour Sarcoidosis www.rheumatology.org.uk/education Question 8 A 59 year old lady presented to the medical admission unit with arthralgia, sore throat and an intermittent temperature for 10 days. On further questioning she has had similar symptoms previously. She has no other significant past medical history. Examination reveals synovitis of the small joints of the hands and a faint macular papular rash was noted in the A&E but has completely resolved now. Her temperature is 37.50C but was 390C in A&E. Chest X-ray is normal as is urine dipstick. Throat swabs, blood cultures, urine dipstick, and a 2D echocardiogram are normal. Hb 9.6 g/dl(11-14.7) MCV 76.4 fl(80-98.1) Plts 777 x10/l(140-370) WCC 18.6 x10/l(3.5-9.5) Neu 16..0 x19/l(1.7-6.5) ESR 100 mg/l CRP120 mg/l ALT 44 iu/l AST 56 iu/l Which one of the following investigations would you do next? 1. 2. 3. 4. 5. ACE Anti-nuclear-antibody Anti- DNase titre Ferritin Viral throat swab Question 9 A 55 year old man is referred to your clinic with skin thickening. There is no history of Raynaud’s and he has no problems with swallowing. He is ANA negative. On examination, he has thickening of the skin of both arms, but sparing of the hands. On lifting his arm, the veins appeared sunken. What is the most likely histological finding on biopsy of the involved skin? 1. Normal epidermis, thickened and sclerosed reticular dermis with dermal expansion extending into subcutaneous tissue. Few adnexal structures seen. No cellular proliferation, minimal inflammatory component. (Morphoea) 2. Normal epidermis and dermis. The deep fascia and lower subcutaneous tissues are oedematous, thickened and infiltrated with lymphocytes, plasma cells, histiocytes and eosinophils. (Eosinophilic fasciitis) 3. The dermis contains an increase in fibroblasts, collagen and interstitial mucin. The fibroblasts are irregularly arranged, and the collagen has a whorled pattern. A sparse perivascular lymphocytic infiltrate is present. (Scleromyxoedma) www.rheumatology.org.uk/education 4. There is a normal epidermis with subjacent pigment incontinence in the papillary dermis. The reticular dermis is replaced by a thick band-like area of collagen. There is a decrease in adnexal structures. There is sparse mild superficial perivascular lymphocytic infiltrate. (Limited cutaneous systemic sclerosis) 5. Whorled, haphazardly arranged collagen bundles are seen in association with an increased number of spindled fibroblasts. There are scattered collections of multinucleated giant cells. There is no other inflammatory infiltrate. (Nephrogenic systemic fibrosis) www.rheumatology.org.uk/education Answers: Q1. 2. Chest x-ray The triad of erythema nodosum, synovitis and bilateral hilar lymphadenopathy is very suggestive of Löfgren's syndrome (Sarcoidosis). This usually carries a good prognosis. Q2. 2. Kawasaki disease This child has presented with Kawasaki disease. The diagnosis requires the following fever for >5days and 4/ 5 of the following conjunctivitis, rash, lymphadenopathy, strawberry tongue and desquamation of the hands and feet. The most important first line management is high dose aspirin. Q3. 5. Prednisolone This patient has features consistent with Sweet’s syndrome, an acute febrile neutrophilic dermatosis. Prednisolone is the initial treatment of choice Q4. 3. MEFV This patient has a periodic fever. He is of Greek origin which suggests Familial Mediterranean fever. This is associated with the MEFV gene mutation. CIASI is a gene mutation associated with the Cryopyrin-associated periodic syndromes (CAPS). CINCA is a subtype of CAPS. MVK mutation is associated with Hyper-IgD syndrome. TNFRFSFIA mutation is found in TNF receptor associated periodic syndrome (TRAPS). Q5. 1.Biopsy of abdominal fat This patient has symptoms and signs of peripheral neuropathy, hepatosplenomegaly, and congestive cardiac failure. He has raised total protein with low albumin suggesting the presence of a circulating protein. With a background of RA he is most likely to have developed reactive serum AA amyloidosis. The quickest test to confirm your diagnosis would be either rectal or abdominal subcutaneous fat biopsy stained for congo red. An abdominal subcutaneous fat biopsy is preferred as it is a more straightforward procedure than a rectal biopsy. However, in some centres rectal biopsy may be the preferred investigation. Q6. 1.Colchicine This patient has a periodic fever. He is of Turkish origin which suggests Familial Mediterranean fever. The most useful long-term treatment is colchicine as it can prevent the onset of Amyloidosis. www.rheumatology.org.uk/education Q7. 5.Amyloidosis This patient has symptoms and signs of malabsorption, nephrotic syndrome and hepatosplenomegaly. He has raised total protein with low albumin suggesting a circulating protein. With a background of RA he is most likely to have developed reactive serum AA amyloidosis. Q8. 4. Ferritin Adult onset Still’s disease (AOSD) is the most likely differential diagnosis. Typical features of AOSD include a quotidian fever often associated with a rash when the fever is present (salmon coloured, macular popular and often confused as a drug reaction). Patients often have sore throat. Other features include deranged transaminase, synovitis of small joints and myalgia. Pleuritis, pericarditis, lymphadenopathy and splenomegaly have been reported. The results of serum ferritin should be interpreted with caution, as it is an acute phase reactant, and likely to be elevated in those with any acute illness, but typically in those with AOSD the serum ferritin levels are extremely elevated. The pronounced neutrophilia makes a viral illness unlikely. Anti-DNAse antibody is positive in those with previous streptococcal infection, and not in those with streptococcal sore throat currently. There are no other features to suggest SLE, or ANCA associated vasculitis. Q9. 2.Normal epidermis and dermis. The deep fascia and lower subcutaneous tissues are oedematous, thickened and infiltrated with lymphocytes, plasma cells, histiocytes and eosinophils. Eosinophilic fasciitis is a scleroderma mimic. It is associated with venous guttering. Characteristic histological features are described in 2 above. Option 1 describes morphoea, 3 describes scleromyxoedma, 4 describes limited cutaneous systemic sclerosis, and 5 describes nephrogenic systemic fibrosis. For further details and pictures, please refer to http//dermatlas.med.jhmi.edu/derm/. www.rheumatology.org.uk/education