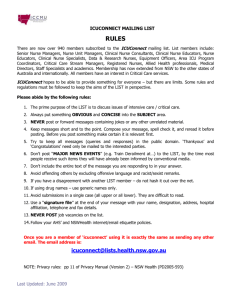
Test Questions for the Final
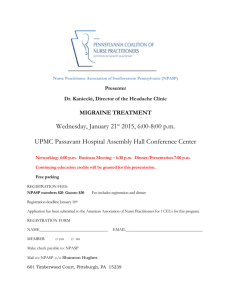
advertisement
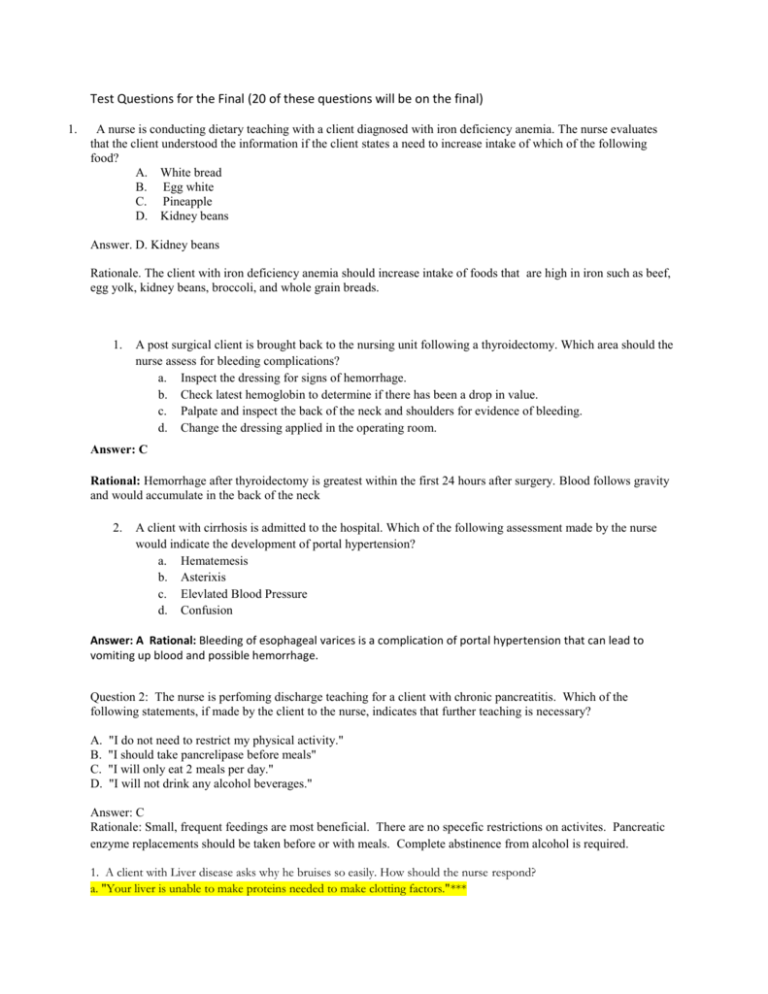
Test Questions for the Final (20 of these questions will be on the final) 1. A nurse is conducting dietary teaching with a client diagnosed with iron deficiency anemia. The nurse evaluates that the client understood the information if the client states a need to increase intake of which of the following food? A. White bread B. Egg white C. Pineapple D. Kidney beans Answer. D. Kidney beans Rationale. The client with iron deficiency anemia should increase intake of foods that are high in iron such as beef, egg yolk, kidney beans, broccoli, and whole grain breads. 1. A post surgical client is brought back to the nursing unit following a thyroidectomy. Which area should the nurse assess for bleeding complications? a. Inspect the dressing for signs of hemorrhage. b. Check latest hemoglobin to determine if there has been a drop in value. c. Palpate and inspect the back of the neck and shoulders for evidence of bleeding. d. Change the dressing applied in the operating room. Answer: C Rational: Hemorrhage after thyroidectomy is greatest within the first 24 hours after surgery. Blood follows gravity and would accumulate in the back of the neck 2. A client with cirrhosis is admitted to the hospital. Which of the following assessment made by the nurse would indicate the development of portal hypertension? a. Hematemesis b. Asterixis c. Elevlated Blood Pressure d. Confusion Answer: A Rational: Bleeding of esophageal varices is a complication of portal hypertension that can lead to vomiting up blood and possible hemorrhage. Question 2: The nurse is perfoming discharge teaching for a client with chronic pancreatitis. Which of the following statements, if made by the client to the nurse, indicates that further teaching is necessary? A. B. C. D. "I do not need to restrict my physical activity." "I should take pancrelipase before meals" "I will only eat 2 meals per day." "I will not drink any alcohol beverages." Answer: C Rationale: Small, frequent feedings are most beneficial. There are no specefic restrictions on activites. Pancreatic enzyme replacements should be taken before or with meals. Complete abstinence from alcohol is required. 1. A client with Liver disease asks why he bruises so easily. How should the nurse respond? a. "Your liver is unable to make proteins needed to make clotting factors."*** b. "Your liver is breaking down blood cells too rapidly." c. "Your liver can no longer store platelets." d. "Your liver is unable to metabolize good stuff for lumps." A 24 year old male is admitted to the ED after collapsing during a marathon. He is diagnosed with severe dehydration. The nurse expects to be infusing which fluids to correct this fluid deficit? a. 0.9% sodium chloride and 20% dextrose in water b. 5% dextrose in water and 3% sodium chloride c. 0.9% sodium chloride and 5%dextrose in water***** d. Lactated ringer's solution and 0.45% sodium chloride The nurse is caring for a pt. admitted for severe ascites secondary to Cirrhosis. His vital signs have been stable, but he has been consistently demonstrating hypotension. What might the nurse expect the doctor to order to assist with pulling the fluid back into the vascular space? a. Hypertonic 3% sodium chloride to increase release of intercellular fluid b. Fresh frozen plasma to increase vascular volume c. Lactated Ringer's to facilitate rapid movement from the extravascular space to the intravascular space d. Albumin to increase the colloid pressure within the vascular space**** 1. a. b. c. d. e. Which of the following criteria indicate and increased risk for pneumonia? (Select all that apply) Stroke victim with dysphagia 34 yo male pt with AIDS 64 yo woman who was vaccinated for pnenumococcus and influenza 6 months ago Post-op pt who received local anesthesia only 17yo female pt with a closed head injury receiving mechanical ventilation A, B, E - A pt with difficulty swallowing is at increased risk of aspiration, which increases the risk of PNA. A pt with AIDS is immunocompromised, which increases the risk of opportunistic infections such as PNA. Mechanical ventilation is invasive and increases the risk of respiratory infections. ATI, Adult Med-Surg Nursing pg 120 ___________________________________________________________________________________________ A nurse reviewing a client's chart discovers that the client's DNR order has expired. The client's condition has not been stable today. The most appropriate action for the nurse to take at this time is to: A. assume that the client still wishes to be a DNR client and anticipate no action if he goes into cardiopulmonary arrest. B. write a note on the front of the primary care provider order sheet asking that the DNR be reordered. C. anticipate that CPR will be instituted if the client goes into cardiopulmonary arrest. D. call the primary care provider to get the order immediatley reinstated. Answer: D Rationale: DNR orders must be reinstated by the primary care provider on an institutionally specified basis. Without a current DNR order, the nurse must institute CPR if the client goes into cardiopulmonary arrest. Since the client has been unstable today, it would be best practice for the nurse to call the primary care provider to get a current order reinstituted. Resource: Leadership and Management Version 4.1 (ATI book) p. 9 Who are at risk for folic acid deficiency anemia? (select all that apply) a. b. c. d. e. Older adults Alcoholics Drug addicts Pregnant women Chemo patients Answer: a, b, c, d, e – those at risk for Folic acid anemia are those with inadequate dietary intake, poor nutrition, increase metabolic requirements and those with malabsorption/impaired metabolism. Pg 1105-1106 In obtaining a nursing history from a 22yr old client admitted with a diagnosis of acute Glomerulonephritis, the nurse specifically asks the client about a recent history of which of the following? a. b. c. d. e. UTI Strep throat Xray using contrast media Illicit drug use Salty meal Answer: b – the most common cause of Acute Glomerulonephritis is an abnormal immune response to beta-hemolytic streptococcus A infection, usually strep throat. Appendix C – A15 1. A pathologist has staged a breast tumor as: T1 N1 M0. When the client asks if her disease has spread to other parts of her body, the nurse explains that: a. a single tumor was found in one lymph node. b. the disease has metastasized to multiple organs. c. the tumor is encapsulated in one area of the breast tissue d. there is no evidence of distant metastasis at this time. Rationale: Tumor staging is used to classify solid tumors and the extent of the disease. T1 refers to the size of the tumor on a 1 to 3 scale; N1 indicates that there is spread of the cancer from the original tumor to one node, and M0 indicates that there is no distant metastasis or spread of the disease. Answers 1, 2, and 3 are incorrect. 1. A 35 year old has just undergone a total thyroidetomy. Which nursing dx has priority with this pt? A. Acute Pain B. Risk for fluid volume deficit C. Risk for airway obstruction D. Imabalanced nutrition less than body requirements Rationale: pg539 Resp distress may result from hemorrage and edema which may compress the trachea, from tetany/laryngeal spasms resulting form decreased hormones due to removal/damage of parathyroid glands, and from damage to laryngeal nerve causing spasm of vocal cords 2. When caring for a patient with chronic renal failure, a nurse should expect to see what laboratory findings?( select all that apply) A. Metabolic acidosis B. Increased urea C. decreased BUN/creatine D. hypophosphatemia/hypercalcemia Rationale: pg916 & 917 Hydrogen ion excretion and buffer production impaired leading to metaboloc acidosis uric acid levels increased creatine/BUN significantly increased (kidney func impaired and not eliminating nitrogenous wastes) phosphate excretion impaired=hyperphosphatemia and hypocalcemia (due to dec vit D synthesis/acitvation) #2. A nurse caring for a patient with a history of CHF, may expect to find which of the following labs elevated? a. Sodium b. BUN/Creat c. Glucose d. WBC Answer: B. Rationale: BUN/Creat may be elevated due to decreased renal function r/t persistent fluid overload. Sodium may be decreased in CHF due to dilution or diuretic therapy. Answers of C,D are not symptoms associated directly with CHF. Sally is a 55 year old female who arrived in the ER complaining of not being able to eat for past 24 hours, feeling nauseous, and complains of pain to her right upper quadrant. Upon assessment you note neck vein distention and edema to the lower extremities. She has a history of hypertension, diabetes, and smokes on regular basis. Based on your assessment and Sally’s complaint what would you say is the probable reason for her complaints and the presenting symptoms? A.) Left sided heart failure B.) C.) D.) Right sided heart failure Myocardial infarction None of the above Page 1026. “In right sided heart failure, increased pressures in the pulmonary vasculature or right ventricular muscle damage impair the right ventricles ability to pump blood into the pulmonary circulation. The right ventricle and atrium become distended, and blood accumulates in the systemic venous system. Increased venous pressures cause abdominal organs to become congested and peripheral tissue edema to develop. Dependent tissues tent to be affected because of the effects of gravity; edema develops in the feet and legs, or if the client is bedridden in the sacrum. Congestion of gastrointestinal tract vessels causes anorexia and nausea. Right upper quadrant pain may result from liver engorgement. Neck veins distend and become visible even when the client is upright due to increased venous pressure.” Risk factors for myocarditis include all of the following except: A.) B.) C.) D.) Stress Alcohol use Intravenous drug use Malnutrition Page 1049, risk factors for myocarditis include, factors that alter immune response, malnutrition, alcohol use, immunosuppressive drugs, exposure to radiation, stress and advanced age. Page 1045 risk factors for infective endocarditis include: heart damage, intravenous drug use, invasive catheters, dental procedures or poor dental health, and recent heart surgery. Question #1 Which statement by a client undergoing external radiation therapy indicates the need for further teaching? 1. "I will wash my skin with mild soap and water only." 2. "I will not use my heating pad during my treatment." 3. "I will wear protective clothing when outside." 4. "I will expose my family members to radiation." Answer #4. Rationales: The client undergoing external radiation therapy requires further teaching when he voices a concern that he might expose his family to radiation. Internal radiation, not external radiation, poses a risk to the client's family. The client requires no further teaching if he states that he should wash his skin with mild soap and water, wear protective clothing when outside, and avoid using a heating pad. Question #2 The staff nurse on the oncology unit must teach the new unit assistant about infection control practices on the unit. The nurse should explain that which measure is most important for preventing the spread of infection? 1. Restricting the presence of fresh flowers and plants on the floor. 2. Using sick time when not feeling well. 3. Frequent handwashing. 4. Refraining from eating or drinking at the nurse's station. Answer #3. Rationales: Frequent handwashing is the most important measure for preventing the spread of infection. Fresh flowers and plants should be restricted in the client's rooms; the staff should use sick time when feeling sick; and she should refrain from eating or drinking at the nurses' station-however, these measures aren't the most important for preventing the spread of infection. 1. Which anemia is an inherited disorder of hemoglobin synthesis in which either the alpha or beta chains of the hemoglobin molecule are missing or defective… a. b. c. d. folic acid anemia glucose-6-phosphate dehydrogenase (G6PD) anemia thalassemia Vitamin B12 anemia Answer: c definition o0f Thalasssemia: an inherited disorder of hemoglobin synthesis in which either the alpha or beta chain of the hemoglobin molecule is missing or defective. (LeMone glossary definition) 1. Hepatitis __________ co-infects people who are also suffering Hepatitis______. a. b. c. d. D and B B and C A and D E and B Answer : A Hepatitis delta only causes infection in people who are infected with Hepatitis B. (LeMone 706). a. b. c. d. 1. This condition results in a goiter as an attempt to increase production of TH. Hyperthyroidism Hypothyroidism Hyperparathyroidism Hypoperathyroidism Answer: B When thyroid hormone production decreases, the thyroid gland enlarges in a compensatory attempt to produce more hormone. a. b. c. d. 2. A toxic multinodular goiter is seen in this condition. Hyperthyroidism Hypothyroidism Hyperparathyroidism Hypoperathyroidism Answer: A Toxic multinodular goiter is a tumor characterized by small, discrete, independently functioning nodules in the thyroid gland causing excessive secretion of thyroid hormone. 2. When a nurse is taking care of a client with hypomagnesemia, which of the following would you expect to see? a. Increased bowel sounds b. hyperactive deep tendon reflexes c. decreased blood pressure d. deep respirations answer: b. hyperactive deep tendon reflexes are an expected finding for a client with hypomagnesium 1. A patient is admitted to the medical surgical unit with exacerbation of multiple sclerosis (MS). What medications do you anticipate being on your MAR for administration to assist the patient with exacerbation of MS? (select all that apply) A. Prozac (fluoxetine) B. Avonex (interferon beta) C. Solu-Medrol (methylprednisone) D. Lioresal (baclofen) E. Ativan (lorazepam) Answer: B, C, D Rationale: Interferon is provided to patients with relapsing MS. It decreases lesions associated with MS. Methylprednisone is used to treat acute exacerbation of MS. Baclofen is a muscle relaxant used to relieve muscle spasms associated with MS. Though a client with MS may feel anxious and have depression due to this debilitating disease process, Prozac and Ativan are not directly associated with the treatment of MS. 2. A man presents to the clinic with possible testicular cancer. What clinical manifestations would you expect to see in this patient? (select all that apply) A. Slight discomfort to testicle B. Swelling to one testicle C. Painful nodule to testicle D. Pelvic pain E. Acute pain to scrotum Answer: A, B, D, E Rationale: One of the first signs of testicular cancer is slight enlargement of one testicle with slight discomfort. Occasionally the patient may complain of pelvic ache. Though uncommon, a patient may complain of acute pain to the scrotum. If a nodule is detected, it usually is painless. 1. The MD ordered 200ml of fluids hourly for the patient who was diagnosed with acute pancreatitis. What is the rationale for this intervention? a. Hyperglycemia has caused an osmotic diuresis b. PLeural effusion of the left lung has reduced blood volume c. Dehydration has occurred due to vomiting d. FLuid has shifted into the retroperitoneal space. Answer: D. Rationale: Activated pancreatic enzymes activated other enzymes (phospholipase A and elastase), which causevasodilation, an increase in vascular permeability and edema. As a result, a large volume of fluid may shift from circulating blood into the retroperitoneal space, the peripancreatic spaces, and the abdominal cavity. LeMone 726 2. The nurse knows that the primary goal of treatment for all shock is to increase: A. Tissue perfusion B. Cardiac contractility C. Sympathetic innervate D. Circulating volume Answer: A. Rationale: Nursing care for the client in shock focuses on assessing and monitoring overall tissue perfusion. As shock progresses, diminished tissue perfusion causes ischemia and hypoxia of major organ systems. A 50 year old Caucasian male with a history of alcoholism, presents to his MD with complaints of nausea, vomiting, steatorrhea and recurrent epigastric and LUQ pain that radiates to his back. The patient states he’s been experiencing all of these problems for a couple weeks. Based on his symptoms, history and timeframe of current change in health status which of the following is/are most likely to be the cause? A) B) C) D) E) Appendicitis Acute Pancreatitis Chronic Pancreatitis Alcohol withdrawal Liver disease Rationale: C (pg 726-727) All of the patients symptoms are related to manifestations of Chronic Panreatitis. Most are also related to Acute Pancreatitis except steatorrhea and he has recurrent epigastric and LUQ pain not an abrupt onset, which are what defines it as Chronic. The patient is male and has a history of alcoholism. 1. The nurse evaluates her teaching as effective when the client recovering from Acute Renal Failure states that he will: A. Limit his fluid intake to 1500 ml or less per day B. Consume only vegetable proteins C. Avoid taking drugs that may be nephrotoxic D. Self-catheterize for residual urine at least once a week. Answer: C pg. 927 Rationale: Nephrotoxic drugs, including over the counter products, can produce further damage to the kidneys and should be avoided. 2. DKA is a result of which pathological process? A. An excess amount of insulin drives all glucose into the cells. B. A decreased amount of glucagon causes low protein levels. C. A deficient in insulin causes fat stores to be used as an energy source. D. An increase occurs in the breakdown of glucose molecules with hypoglycemia. Answer: C pg.598 Rationale: Increased glucagon levels and deficit of insulin increases the liver’s production of ketone bodies and increased releases of free fatty acids. With this process, bicarbonate production is decreased and it cannot buffer so metabolic acidosis occurs. 1. Mr Jefferson is in advance renal stage disease. Which of the following prescribed medications should the nurse be concerned about? a. b. c. d. Benadryl Iron Tylenol Maalox Answer D. Page 916. Hypermagnesia develops with advancing renal failure. It is necessary to avoid antacids containing magnesium. Possible effects of hypermagnesia: deep tendon reflexes, facial paresthesia, flaccid muscle paralysis, depressed respiration and apnea. 1. Jack come to ER with diagnosis of pulmonary embolism. It is a medical emergency. The nurse realizes that the possible manifestations of pulmonary embolism are the following. (Select all that apply.) a. b. c. d. e. dyspnea chest pain bradycardia low grade fever cough Answers A,B,D,E. Page 1348. Bradycardia is not included. It should be tachycardia because the patient is trying to compensate. The classic triad of symptoms of renal cell carcinoma include which of the following symptoms? A) Gross hematuria B) Oliguria C) Flank pain D) Uremia E) Palpable abdominal mass Correct answer: A, C, E Rationale: Renal tumors are often silent with few manifestations. The classic triad of symptoms, gross hematuria, flank pain, and a palpable abdominal mass, is seen in only 10% of renal cell carcinoma (Lemone pg 896). Which of the following neurological disorders does not exhibit sensory or cognitive changes? A) Multiple Sclerosis B) Amyotrophic Lateral Sclerosis C) Myastrenia Gravis D) Parkison's disease Correct answer: B Rationale: ALS is a rapidly progressive and fatal degenerative neurological disease characterized by weakness and wasitng of muscles under voluntary control, without any accompanying sensory or cognitive changes (Lemone pg 1645). 1) Which of the following medications would a patient take that suffers from systemic lupus erythematosus and require an eye exam every six months to prevent irreversible blindness? a. Imuran b. Prednisone c. Plaquenil d. Cylosporine Answer: C Rationale: Retinal toxicity and possibly irreversible blindness are the primary concerns with the antimalarial drug Plaquenil. Page 1473 2) Sickle cell anemia can have the following potential complications. Select all that apply. a. Stroke b. Polycythemia c. Pathologic fractures d. Pulmonary embolism Answer: A & D Rationale: Stroke may result from cerebral vessel occlusion. Acute chest syndrome a symptom complex that includes fever, chest pain, an increasing WBC count, and pulmonary infiltrates, may develop as well as other pulmonary complications such as pneumonia, pulmonary infarction, and pulmonary embolism. Page 1109 Pathologic fractures are seen in acquired hemolytic anemia. 2. Cooper is a 28 year old male that comes to the ER for continual weight loss over the last 2 months. The nurse asks Cooper during the assessment if he drinks, smokes, or uses drugs. Cooper states he has been drinking since he was 14, but only beer and only a 12 pack a day. The nurse asks Cooper do you have any other health problems, "Cooper states my DR. said I was anemic. Whatever that means." The nurse knows she needs to educate Cooper on what type of anemia: A. Folic acid anemia B. Vitamin B anemia C. Sickle cell anemia D. Beta Thalassemia anemia Answer: Folic acid anemia Rational: Folic acid anemia is caused by poor nutrition, and chronic alcohol abuse. 1. Mr. Smith, 78 years old presents to the Emergency department with anorexia, polyuria, and a blood glucose of 625. He has type 2 diabetes and his urine shows hyperosmolality without ketones, based on the clinical findings what would be his likely diagnosis? a) DKA b)HONK c) hyperglycemia d) metabolic acidosis Answer is B; Rationale: HONK is characterized by a blood glucose of >600, typically in elder patients with type 2 diabetes. HONK is also characterized by hyperosmmolality from osmotic diuresis, without ketones present. DKA usually has a blood glucose of >250 but with the presence of ketones which rules answer a out. A blood sugar of greater than 600 would be significant of hyperglycemia, but with all the other evidence in the question there is a more accurate diagnosis which is B rather than C. Acidosis is not present in HONK which rules out answer D 1. A nurse reviewing a client's chart discovers that the client's DNR order has expired. The client's condition has not been stable today. The most appropriate action for the nurse to take at this time is to: A. assume that the client still wishes to be a DNR client and anticipate no action if he goes into cardiopulmonary arrest. B. write a note on the front of the primary care provider order sheet asking that the DNR be reordered. C. anticipate that CPR will be instituted if the client goes into cardiopulmonary arrest. D. call the primary care provider to get the order immediatley reinstated. Answer: D Rationale: DNR orders must be reinstated by the primary care provider on an institutionally specified basis. Without a current DNR order, the nurse must institute CPR if the client goes into cardiopulmonary arrest. Since the client has been unstable today, it would be best practice for the nurse to call the primary care provider to get a current order re-instituted. 1. Which of the following criteria indicate and increased risk for pneumonia? (Select all that apply) a. Stroke victim with dysphagia b. 34 yo male pt with AIDS c. 64 yo woman who was vaccinated for pnenumococcus and influenza 6 months ago d. Post-op pt who received local anesthesia only e. 17yo female pt with a closed head injury receiving mechanical ventilation A, B, E A pt with difficulty swallowing is at increased risk of aspiration, which increases the risk of PNA. A pt with AIDS is immunocompromised, which increases the risk of opportunistic infections such as PNA. Mechanical ventilation is invasive and increases the risk of respiratory infections. ATI, Adult Med-Surg Nursing pg 120 ______________________________________________________________________________ _____________ 2. The nurse should closely monitor a pt who has a nasogastric tube for suctioning for which of the following electrolye imbalances? a. Hypokalemia b. Hyponatremia c. Hypokalemia and hyponatremia d. Hypomagnesemia C Nasogastric losses are isotonic, containing both sodium and potassium ATI, Adult Med-Surg Nursing pg 391