OB GYN Review
advertisement

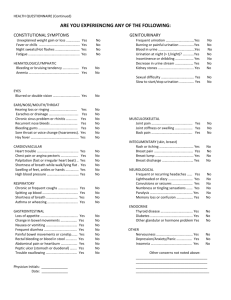
Dr. Christensen 1/28 Transcription: Czubatyj OB/GYN Review I. II. III. IV. V. Informed Consent: a. Least important part is signature b. Must include: i. Procedure vii. Complications (not particular surgeon but ii. risks (up to and including for procedure) death) viii. Self Efficacy—if patient is informed they iii. alternatives believe they can make proper choices iv. expectations ix. Demand efficacy—Patient trying to please v. failure chance the doctor vi. cost (overall) c. If have surgical emergency, don’t do any elective stuff as well Ethics a. Beneficence: do the right thing, advocate for the patient b. Nonmalficence: do no harm, no added procedures c. Futility: doing something with no expectation of working i. Not obliged to start something futile ii. Not allowed to stop a futile treatment once started d. Patient Autonomy: implies informed consent – they can choose e. Physician autonomy: you choose right thing for the patient f. Standard of care: legal term that is what a similar physician would do in a similar condition. Depends on geography. Female screening a. Pap smear i. Start at 21 or 3 years after first sexual encounter and go yearly ii. If low risk, q3 years b. Mammogram i. Start at 40-50 q2 years ii. >50 q1 year c. HPV—Yes starting at 30 d. BP, weight, general physical and Pelvic: yearly e. Rectal: i. >40 do rectal + pelvic and guiac every time f. Colon: i. Colonoscopy q10 years starting at 50 ii. Sigmoidoscopy q5 years starting at 50 g. Cholesterol: start at 20, q5 years until 65 h. TSH: starting at 65 i. CXR, CA-0125, TVUS: NOT screening tests—to many false + j. Endometrial thickness—no Maternal-fetal physiology (LOOK AT NOTES FROM CD) a. Increased progesterone causes increased CO2 causes increased respiration causes decreased PCO2 causes respiratory alkalosis causes kidney to dump bicarb b. End up with a compensated respiratory alkalosis and basic urine c. Every hormone in pregnancy goes up EXCEPT DHEA-SO4 d. Renal blood flow increases, GFR increases, glucose in urine increases e. Never should have protein in the urine – always pathologic Preconception care a. All patients: i. Folate 1. 0.4mg 2. 4mg if had previous NTD ii. Test for DM—if +--↑ risk of birth defects Dr. Christensen 2/28 Transcription: Czubatyj VI. iii. Rubella 1. if not immune—immunize 2. cannot immunize during pregnancy iv. General—Pap, VDRL, Chlamydia, CBC b. Normal patient i. First visit: Pregnancy Confirmation, CBC, T&S, Rubella, VDRL, GC, Chlamydia, HIV, HEP (core: infected, now immune; surf ab: immunized, immune; surf ag: infected), PAP, GA, PPD, UA & C&S, breast exam, Rh testing ii. Planned visits: 1. 16-18 weeks: AFP (triple screen/quad screen) 2. 22 weeks: ultrasound for anatomy 3. 26 weeks: glucola, if elevated do 3 hr GTT 4. 36 weeks: cervical cultures, repeat STDs, cervical check 5. 40-41 weeks: fetal surveillance (NST) c. Diabetic: IDDM pregestational i. Worry about: 1. Glucose: causes embryopathy. a. Most common: CV, GI b. Most specific: caudal regression c. Need to check HgbA1C, fasting glu, 2 hr postprandial d. Check i. Eye: fundoscopic exam ii. Heart: EKG iii. Kidney: 24 hr urine for protein, Cr clearance iv. Neuropathy: follow neuro exam ii. Problems: macrosomia, placenta gives out so induce early Triple screen a. Increased AFP i. Worry about: NTD, wrong dates, twins ii. Do an u/s and repeat AFP 1. If normal and AFP still up, do an amnio AFP and AChE 2. Confirmed increase is an occult NTD b. Decreased AFP: wrong dates, aneuploidy, IUGR i. Get u/s to confirm dates, in not – need amnio Trisomy 21 Trisomy 18 VII. AFP Down Down HCG Up Down Estriol Down Down Bishop Score/Fetal survey for inducibility: Factor 0 1 2 3 Closed 1-2 3-4 5+ Dilation 0-30% 40-50% 60-70% 80%+ Effacement -3 -2,-1 0 +1,+2 Station Firm Medium Soft Consistency Posterior Mid Anterior Position a. Cervical length (bad of long) b. Position (bad if post) c. Consistency (bad if firm) d. Effacement (bad if fingertip) e. Station (bad if <0) f. Treatment is to ripen the cervix byDilation with PGE1 or PGE2 and then pitocin Dr. Christensen 3/28 Transcription: Czubatyj VIII. Cardinal movements of labor (first 2 can be flip-flopped) a. Descent b. Flexion c. Internal rotation d. Extension e. External rotation (aka restitution) f. Expulsion IX. APGAR scoring 0 1 2 0 <100 >100 HR Absent Irreg Crying Resp None Grimace Cry Reflexes Limp Flexion Flex/Extension Tone Blue Blue extremities Pink Color a. Cannot get all pink (10) apgar at 1 min X. Postpartum care a. Hormones i. Lactation 1. ↑ PRL 2. Need decreased E2 to increase PRL so can’t use OCPs (progestin only when breast feeding) 3. ↑ Oxytocin - + suckling 4. hypoestrogenic: a. hot flashes b. Dyspareunia c. Vaginal Dryness b. Greatly increase metabolism postpartum (↑Caloric expenditure↓Fat) c. Increased risk of DVT d. Psychiatric i. Blues: normal – need reassurance 1. Should stay in bed ii. Depression (15%): ask about suicide, harm baby, call psychiatrist iii. Psychosis: told by Satan – need to protect family 1. Suicide/Homicide 2. Hospitalize, Call psychiatrist, antipsychotics XI. Ectopic Pregnancy: 1-2% of all pregnancies a. Risks: normal risk 1-2% i. Tubal Fulgaration ii. IUD—progesterone iii. Previous Ectopic iv. History of infertility and/or PID b. Presentation: i. Amenorrhea ii. Pain iii. Culdocentesis: 1. Non-clotting blood +--has ectopic 9/10 times 2. negative = clear fluid 3. everything else is non diagnostic c. Diagnosis: i. 1500 quant—Gest sac with TVU/S ii. 6500 quant—gest sac with TAU/S iii. No diagnosis if below these 2 iv. 3000 + TVUS = no Gest Sac = ectopic 1. if quant goes up—do something Dr. Christensen 4/28 Transcription: Czubatyj 2. MTX a. b. c. d. 3. D+C a. b. 4. Ectopic treatment Make sure not viable IUP Absolute contraindications: i. Hepatitis ii. Renal disease iii. Peptic ulcer iv. Allergic Relative: i. Size >3.5 ii. Hcg—5-15K iii. Cardiac motion Chorionic villi i. IUP ii. Might interrupt pregnancy no chorionic villi i. ectopic Scope: a. Diagnostic b. Surgery: i. Salpingostomy—open tube, leave open ii. Salpingestomy—take tube out d. BHCG should double in 48 hrs but should not use this exclusively i. If the BHCG is the same and there is no sac – abnormal pregnancy e. Examples: i. HCG of 1000 and no sac, repeat in 48 hours and get hcg of 1200 and no sac. Tx options: 1. Observe 2. D&C, if find POC then abort, if not then ectopic 3. Laparoscopy 4. Treat with MTX ii. Abdominal pain, abdominal distension, hypotension, + pregnancy 1. Needs laparotomy f. No surg if: previous surg g. No surg or MTX if: alcoholism with impaired liver fxn h. If patient gets second ectopic on same side, remove it surgically XII. Insulin dependent pregestational diabetes Diet-controlled Insulin controlled None B, C, D Pregestational A1 A2 Gestational a. Types B, C, and D are the worst patients and you see birth defects – GI, CV, and caudal regression b. Pre-gestational: i. White classification—A,B,C,D ii. 90% same as gestation 1. big babies 2. birth defects a. CV b. Genitourinary c. Caudal regression—arms and legs don’t develop iii. 10% IUGR: 1. Asymetrical—reversible (big head) 2. Symmetrical—worse a. Perinatal viruses (TORCH) b. Abnormal Karyotype Dr. Christensen 5/28 Transcription: Czubatyj XIII. c. Low fluid (oligo) iv. Normal fluid with symmetrical IUGR—normal baby v. Parvovirus: 1. big baby 2. slap baby appearance 3. anemia 4. hydrops fetalis vi. Maternal serum—Scans—Amnio c. Gestational: i. Risk: 1. Family history 2. Obesity 3. Large Placenta ii. Diagnosis: 1. 50gm 2. if abnormal do GTT iii. types: 1. A1—diet controlled 2. A2—med controlled iv. Problems: 1. ↓ Glucose, Ca, Temp 2. ↑Bilirubin, Hct 3. Macrosomeia a. Cephalopubic disproportion i. Distocia—Labor slow—C-section ii. Shoulder Distocia b. Risks for Shoulder Distocia: i. Big baby ii. Most don’t have any risk factors iii. Very slow labor iv. Turtle sign—baby crowns when pushing, then completely disappears when pushing stops c. Attempt to correct shoulder distocia: i. McRobert’s ii. Suprapubic pressure iii. Deliver posterior shoulder iv. Episiotomy (4th degree) v. Wood’s Screw vi. Break clavicles vii. Zavanelli—cannot get baby out, put it back in PIH (classic pre-eclampsia (after 20wks)) a. See non-dependent edema (hands, face), protein > 300 mg/dL, BP > 140/90 on 2 sep measurements, weight gain >2 lbs/wk b. Prostaglandin imbalance c. Risk factors: i. 1st pregnancy ii. Increased placenta volume iii. Vascular disease iv. History of preeclampsia v. Chronic HTN d. Tx: i. Mild: admit, bedrest on left side, BPP e. Severe: protein at 5000, bp: 160/110 1 time i. Neuro sx: ha, vision changes, increased reflexes, seizures, clonus ii. Heart sx: pulmonary edema, heart failure, ↑,↓CO iii. Kidney sx: 4 + prot, Cr >1.0, oliguira (<400cc) Dr. Christensen 6/28 Transcription: Czubatyj XIV. XV. iv. Liver sx: DIC, ↑LFT, RUQ pain, HELLP (**remember high bp not part of HELLP) v. Tx: delivery 1. amnio for lung viability if yes induce, if no bethamethasone vi. HTN Tx: 1. hydralazine (arterial vasodilator), labetalol (alpha/beta antagonist) if used can cause hypotension – fetal distress 2. never use diuretics f. Seizures: treatment is MgSO4 – can stop breath and lead to hypotension g. If mom in trouble, try to resuscitate for 4 minutes on mom and then get baby out Isoimmunization a. 85% of mothers are Rh + b. Prevention: RhoGAM – is IgG that can cross placenta i. Will kill baby’s cells within the mother ii. Small dose will not effect baby c. When given i. 28 wks ii. Maternal –fetal transfusions iii. Postpartum iv. D&C (miscarriage) v. Ectopic vi. Mom accident (MVA) d. Klenhauer-Betke: calculate how much fetal blood went into mom so you know how much RhoGAM to administer i. 300 mcg of RhoGAM kills 15 mL of fetal RBCs e. ROM at 12 weeks, Rh -, titer of 1:32: do amnios – if see bilirubin in amniotic fluid – indicates hemolysis – estimate danger via Liley curve i. Zone one—no worries ii. Zone II—slightly worried iii. Zone III—very worried f. Can cause hydrops fetalis in newborn if needed can transfuse O- blood (PUBS or cordocentesis) Twins a. How these come about: i. Remember that the chorion arises before the amnion ii. Separation day: (Amnion/Chorion) 1. 1-4 days--before trophoblast differentiation, get Di-Di 2. 4-8 days--after trophoblast diff but before amnion formation get Mo-Di 3. 8-12 days--after both trophoblast diff and amnion form, get Mo-Mo 4. >12days--conjoined b. Mo-Di i. Bilirubin = hydrops ii. TTTS: twin to twin transfusion syndrome iii. Rather be little – asymmetric growth retardation c. Mo-Mo i. Cord accidents d. Di-Di i. No increased risk over previous pregnancy ii. Increased PTL iii. Decreased fetal weight iv. Increased previa v. Increased PIH vi. Increased abruption vii. Want to carry to 32 wks vs. 40 wks viii. Increased c/s ix. If first is vertex, can deliver second breech Dr. Christensen 7/28 Transcription: Czubatyj XVI. Cancers: a. Cervical i. Risk Factors 1. HPV (16,18, 30s [not 6] ) LES, Multiple partners 2. Smoking 3. HIV—immune suppression, transplant 4. Transformational Zone (TZ) ii. Presentation: 1. No symptoms (abnormal Papcolposcopy) 2. Post-coital bleeding (pap/biopsy) 3. Terrible triad—cancer spread to pelvic side walls a. Edema b. Sciatica c. Hydronephrosis d. Prognosis not good iii. Diagnosis: 1. Biopsy—not Pap 2. Leep, Cone, Cervical iv. Staging: 1. stage I—cervix only 2. Stage III and IV—mets v. Treatment: 1. Radiation therapy: a. Brachy i. Up close ii. Radiate cervix iii. Cesium, Radium in cervix iv. 400 Rads is fatal v. Cervix receives 20,000 RADS b. Tele i. Cobalt used ii. Radiate pelvis iii. Kill off lymph nodes 2. Hysterectomy (radical—remove tissue around organs also) if caught early vi. Follow Up: 1. early—90% cure rate 2. late—very little chance 3. Return—fatal 4. return inside pelvis—remove pelvis—pelvic exoneration vii. Papsmear: 1. Systems: Papinicolou WHO (created by UN) Bethesday (created by US Negative Satisfactory Class 1 Atypical—inflammatory Inflammatory Class 2 Atypical—HPV LGSIL Class 2 Mild Dysplasia: CIN1 LGSIL Class 3a Moderate dysplasia: CIN2 HGSIL Class 3b Severe Dysplasia: CIN3 HGSIL Class 4 Cancer Cancer Class 5 a. Bethesda also has: i. ASCUS 1. Atypical Squamous cells of undetermined significance Dr. Christensen 8/28 Transcription: Czubatyj 2. b. c. d. e. f. b. c. Tx options are—colposcopy, repeat pap (if still abnormal colpo), HPV tping—high risk—colpo, low risk nothing ii. AGUS now replaced by AGC—Atypical Glandular cells Treatment NEG—repeat in 1-3 years UNSAT—repeat immediately ASCUS—see above LG, HG, ACG, CA--colposcopy Endometrial: i. 2 types: 1. Type 1 a. Excess estrogen b. Early grade, stage c. Very curable 2. Type II: a. N estrogen involved “ovarian cancer” b. Clear cell, papillary serrous c. Bad prognosis ii. Risk Factors: 1. ↑ Estrogen: a. Obesity b. Aromatase in adipose tissue converts testosterone to estrogen 2. Physician: a. Adding Estrogen b. Prempro (provera+Premaria) c. Granulosa cell tumor d. PCOS—no ovulation = no progesterone (stops endometrial ca) e. Tamoxifen--↓Breast Cancer, ↑endometrial Cancer iii. Diagnosis: 1. Endometrial Biopsy: a. + - treat cancer b. – D+C or hysteroscopy 2. Never use Pap for diagnosis iv. Treatment: 1. TAH + BSO + staging (lymph node dissection) 2. BSO pathology: a. Good: i. Watch ii. May recur in vaginal cuff iii. Pap, pelvic exams b. Bad: i. Grade III, deep invasion, spread ii. Radiation therapy—radiate pelvis Ovarian: i. Types: 1. Epithelial (90%) a. most common benign and malignant i. <50% benign ii. >50% malignant b. 5cell types: i. Type -- normal counter part—marker ii. Serrous—fallopian tube—CA125 iii. Clear cell—Kidney—CA125 iv. Brenner—Bladder—CA125 Dr. Christensen 9/28 Transcription: Czubatyj 2. 3. v. Endometrial—Endometrium—CA125 vi. Mucinous—endocervix—CEA vii. Germ Cell—AFP viii. Placental site trophoblastic tumor (PSTT)—HPL ix. Krukenberg—mets GI--CEA x. Serrous and clear cell also in endometrium c. False Positives for CA125: i. Endometriosis ii. Peritonitis iii. Fibroids iv. Pregnancy v. Cirrhosis *** Stromal (hormonally response) a. types: i. Granulosa cell 1. Makes estrogen 2. Maker—inhibin ii. Leydig cell tumor: 1. Testosterone 2. Marker = testosterone b. Presentation: i. Leydig—Virulization—temperol balding, beard, etc ii. Granulosa: 1. Child—abdominal mass, breast development, vaginal bleeding 2. Post menopausal—adnexal mas, endometrial cancer c. Treatment: i. Find and remove ii. Post menopausal—check for endometrial cancer Germ Cell Tumor a. types: i. Dermoids (teratoma)—can cause torsion—remove them 1. Dermal 2. Specialized a. Struma Overii—thyroid hormone i. Hyperthyroid ii. Adnexal mass b. Carcinoid: i. Serotoninbreakdown product—Carcinoid Syndrome ii. Flushing, Wheezing, Diarrhea c. Immature (malignant)—no markers ii. Dysgerminomas: 1. Seminoma 2. Most concern LDH iii. Choriocarcinoma 1. HCG 2. Gestational Trophoblastic Disease iv. Endodermal sinus tmors—AFP Dr. Christensen 10/28 Transcription: Czubatyj b. c. d. 4. d. Mets: a. Risk Factors: i. None ii. Age (teenagers) iii. Dysgerminomas found in patients with undescended testes (always find out if patient is XX or XY) iv. Infertility/amenorrhea Presentation i. Young ii. Rapidly growing mass iii. Ruptures iv. Intraperitoneal bleeding Treatment: i. USO ii. Surgical staging iii. Chemo (cure rate>90%) Rules: i. Bilateral ii. Breast iii. Colon iv. Endometrial b. Krukenberg tumor—gastric cancer, signet cell, CEA marker ii. Risks for ovarian Ca: 1. Ovulation (1-99) (OCPs↓), (clomaphene↑) 2. Genetics a. BrCa1—2 cancers—ovarian/breast b. BrCa2—1 cancer—breast c. Lynch1—hereditary nonpolyp colon cancer (HNPCC) d. Lynch2 i. HNPCC ii. Ovary iii. Breast iv. Endometrial v. Prostate e. Site specific ovarian cancer—ovarian cancer in family tree f. <5% of ovarian cancer fits genetics—95% only have ovulation as risk factor 3. Talc powder—controversial iii. Presentation: 1. Vague 2. GI complaints 3. Pelvic mass 4. ↑CA125 iv. Treatment: 1. TAH+BSO+staging+Chemo 2. most patients respond, most recur—once recur—incurable 3. Die of GI block—vomiting can’t stop 4. live maybe 3 years after recurrence Breast i. Risk factors: 1. age 2. gender 3. breast cancer on one side already Dr. Christensen 11/28 Transcription: Czubatyj Tamoxifen Raloxifen Premorin Prempro ii. medium risk factors: 1. Gail model a. Age b. Race c. Age of menarche d. # of first degree relatives with breast Ca e. # of abnormal breast biopsies f. Age of first child 2. gives #--if >1.8 offer tamoxifen iii. Others Risk factors 1. Genetics a. BrCa1,2 b. Lynch 2 c. Leifromeni—p53 defect i. Kids—sarcoma ii. Men—breast cancer 2. obesity: a. hormonal replacement therapy i. prempro—causes breast Ca, stroke, MI, dementia, ↓Colon Ca, osteoporosis ii. premorin—no—strokes (CVA)—prevents hot flashes, osteoporosis, colon cancer iii. OCP—no b. Fat and alcohol increase, c. smoking is protective 3. Alcohol 4. smoking ↓ breast Ca 5. ↑Exercise↓Breast Ca iv. Presentation: 1. Lump—suspiscious—biopsy 2. Mammogram— a. Positive if i. Microcalcifications ii. Spiculations b. Tests: i. Needle localized ii. Stereotactic biopsy v. Treatment: 1. modified Radical mastectomy a. lymph node dissection b. some tissue 2. Lumpectomy a. Quadrant of bast b. LND—if + i. Premenopausal—chemo ii. Postmenopausal—tamoxifen iii. Usually everyone gets both vi. SERMS (selective estrogen receptors modulator) ↓ Breast Ca ↑ Endometrial Ca ↓Osteoporosis ↑Vasomotor ↓Breast Ca ↓Endometrial ca ↓Osteoporosis ↑Vasomotor No change ↑Endometrial Ca ↓Osteoporosis ↓Vasomotor ↑ ↓ ↓ ↓Vasomotor Dr. Christensen 12/28 Transcription: Czubatyj e. f. g. Vulvar: i. ii. iii. iv. v. Most Squamous Cell Carcinoma from TZ, HPV (almost always type 16) 2nd most common = melanoma Adenocarcinoma—15-20% DES—clear cell carcinoma of cervix/vagina Lymph node drainage: 1. uterus cervixPelvicaorticthoracic 2. Vulvainguinalpelvicaorticthoracic 3. Vagina: (behaves like) a. L 1/3—Inguinal b. M1/3—behaves like both c. U1/3—Cervical vi. Stains: 1. Lugol—iodine stains glycogen—used for vaginal 2. Vulva uses Talofin Blue Gestational Trophoblastic Disease i. Mole—uncontrolled placenta—placenta grows out of control ii. Complete: 1. characteristics: a. Daddy’s girl b. All paternal DNA—sperm meets blighted ovum 23X46XX c. trophoblast d. No embryo, just placenta 2. Diagnosis in ER a. SD+C i. 85% resolve ii. GTD= 15% recur—1-3%-->choriocarcinoma (CCA) b. recur: i. act like cancer ii. grow into tissue iii. recurrent or invasive mole iv. Kill patient if not treated v. Chemo (MTX) c. CCA: i. Doubling time 24hrs ii. 65% cure rate iii. Incomplete: 1. characteristics: a. 2 sperm fertilize 1 egg b. 23x2 + 23X = 69 c. trophoblast+fetus 2. Diagnosis in ER—same as complete except 99% resolve and 1% recur iv. 1/20,000 pregnancy turn into CCA—check HCG v. Cytotrophoblasts--*synciotrophoblasts (both can turn into CCA vi. * = intermediate cell 1. placental site trophoblastic tumor (PSTT) 2. if INT cellCCA a. human placental lactogen b. hysteroscopy Vaginal: i. Mets ii. SCC iii. DESclear cell Ca of Vagina 1. 25%: a. t shaped uterus b. Cox comb cervix Dr. Christensen 13/28 Transcription: Czubatyj c. infertility d. adenosis—glands where not supposed to be 2. 1/10,000—Ca iv. Sarcoma bacteriodes 1. infertile with mass coming out of vagina 2. Rhabdomyosarcoma XVII. Polycystic Ovarian Syndrome: a. Hirsutism, oligomenorrhea, +/- obesity, may be infertile b. Diagnosis: i. Polycystic ovaries on TVUS—string of pearls ii. Anovulation by increased LH/FSH and increased androgens (LH/FSH >2:1) iii. Increased fasting insulin because have insulin resistance iv. Glucose/Insulin is decreased v. Abnormal GTT c. What to do: i. May have increased chance of endometri ca (>30yo) so do endo biopsy ii. Regulate cycles iii. Worry regarding insulin resistance, therefore give metformin XVIII. Amenorrhea: a. Primary—no period by 16 or 14 if appear abnormal i. Constitutional ii. Imperforate hymen 1. cyclic pain 2. blue bulge at perineum 3. treatment—cruciate opening iii. Septum iv. Mullerian Agenesis 1. no mullerian tract—vagina, cervix, uterus, tubes 2. ovaries normal 3. renal problems 4. XX 5. Need creation of neovagina v. Testicular Feminization (XY)—no testosterone receptor 1. very increased testosterone 2. +MIF, Y chromosome present, no uterus 3. Negative axillary/pubic hair (KEY) 4. excess test—converts to estrogen—breast development 5. have undescended testes a. 25% of dysgerminoma b. Need orchiectomy post puberty and neovagina b. Development: Disease Karyo Breast Uterus/ Pubic/Ax Cancer Other Treatment Vagina hair risk XX + + No Neovagina MA XY + Yes Neovagina, T Fem orchiectomy 45 XO Infantile + No Osteoporosis OCPs Gonadal dysgen 46XX Infantile + No Osteoporosis OCPs Gonadal dysgen 46 XY Infantile + YesOsteoporosis OCPs Gonadal testic Orchiectomy dysgen (no MIF) 46XX Infantile No Osteoporosis Malignant 17 HTN, make OHase tons of deficient Aldosterone Dr. Christensen 14/28 Transcription: Czubatyj c. XIX. Secondary amenorrhea workup i. Preg test—if – continue ii. Progestin withdrawal test 1. Bleeding = +annovulation a. TSH b. Prolactin c. PCO 2. no bleeding: - check estrogen and progesterone iii. Estrogen + Progesterone: 1. negative : a. asherman’s b. HSG c. hysteroscopy 2. Bleeding: a. uterus works—problem somewhere else b. check FSH level i. ↑ = menopausal ovary ii. ↓ or = =ovary okay 1. Pit CT/MRI a. + = Pituitary tumor b. - = hypothalamus i. Hypothalamic ammenorhea ii. – progesterone iii. – estrogen = osteoporosis d. Summary: i. + Progestin—bleeding—annovulation ii. – Progesterone = asherman’s iii. ↑FSH = ovarian failure iv. Everything normal= hypothalamic Virulization: a. Sites: i. Ovary 1. Leydig cell tumor 2. Adnexal mass 3. Testosterone levels ii. Adrenal 1. General: a. 17-21-11—Cortisol b. 21-11-18--aldosterone 2. 21-hydroxylase deficiency 3. ↓cortisol 4. **check ** ↑17-hydroxyprogesterone iii. Drugs (steroids) 1. Normal testosterone 2. No adrenal mass 3. UDS b. Presentation: i. Infant—ambiguous genitalia ii. Adult (19+) 1. period stops—ammenorhea, Congenital Adrenal Hyperplasia (CAH) 2. happens slowly c. Other: i. CAH or adrenal hyperplasia ii. Adrenal Adenoma—any age, DHEA sulfate Dr. Christensen 15/28 Transcription: Czubatyj iii. PCO—high LH, Low FSH (LH/FSH ratio >2) Abnormal/Normal Bleeding: a. Causes: i. Adenomyosis 1. tons of bleeding 2. tender boggy enlarged uterus 3. dysmenorrheal, dysparenuia, chronic pelvic pain ii. Coagulopathy (Von willebran’s disease and ITP) 1. Will die with first menstrual period if no intervention taken iii. Dysfunctional Uterine Bleeding: 1. Diagnosis of exclusion 2. no fibroids, ca, adenomyosis, endometriosis 3. some type of hormone problem a. decreased E2, spotting due to endometrial atrophy b. decreased Pg—see in teens who have 1-2 periods/p=year that are terrible and land them in hospital c. Increased PG—Give DepoP or OCP and they will spot/bleed iv. Endometriosis: 1. Pain and infertility 2. Adnexal tenderness 3. Only 1/3 have irregular bleeding v. Leiomyoma 1. most are asymptomatic 2. If symptoms—pain, pressure, irregular bleeding 3. Have a multinodular, irregular uterus vi. Carcinoma: 1. Postmenopausal bleeding—endometrial Ca 2. Postcoital bleeding—cervical ca 3. Vague complaints—ovarian ca 4. Painless lump—vulvar ca 5. Usually metastatic—vaginal ca b. Dysmenorhea:--pain during period i. Primary: 1. periods always were painful 2. ↑serum prosoglandins 3. no Pathology 4. Treatment—NSAIDS, OCPs Wrong diagnosisscope ii. Secondary: 1. Pain is new 2. Endometriosis—laparoscopy 3. Adenomyosis—hysterectomy 4. Diagnosis needed: a. Endo—Lupron, Laser, Hyst b. Adeno—TAH iii. GI complaints, Pelvic pain—Spastic Cholitis iv. Interstitial Cholitis--+ K sensitivity Test XXI. Climacteric: Drug Breast Cancer Endometrial Cancer Premarin* No change ↑ Tamoxifen ↓ ↑ Raloxifen ↓ ↓ Prempro** ↑ ↓ *--conjugated Estrogens **--combined conjugated estrogen/medroxyprogesterone acetate XX. XXII. PMS: Dr. Christensen 16/28 Transcription: Czubatyj a. Cyclic Depression i. Sleep ii. Intent iii. Guilt iv. Energy v. Concentration poor vi. Appetite vii. Psychomotor viii. Suicide ix. SIGECAPS b. 5+ for >2 weeks—depression episode c. PMS = 5-10 days out of the cycle before the cycle d. Somatic Symptoms i. Headache ii. Abdominal pain iii. GI iv. Etc e. Diagnosis made by Diary i. Rule out hyperthyroid (TSH test) ii. Alcoholism iii. Depression Questionare -, history of alcohol not prominent f. Treatment: i. Fluoxetine (prozac)—SSRI ii. Alprazolam (Zanex) XXIII. Reasons for surgery with fibroids: a. Severe symptoms b. Anemia c. Organ damage d. Suspiscios for cancer—almost never—sarcoma i. Post menopausal fibroid ii. Rapidly growing fibroid e. other treatments: i. Surgery ii. Lupron iii. Watch iv. Myomectomy—never do unless patient wants to retain fertility v. Uterine Artery (UA) embolization XXIV. Sexual response Cycle: a. Female: i. Libido ii. Excitement iii. Orgasm iv. Plateau v. Resolution b. male is the same except instead of plateau has refractory c. Libido is most common problem, poor prognosis i. No interest in sex (aversion disorder) ii. Depression, drugs (alcohol, SSRI, Illicit), relationships (domestic violence) d. Excitement: i. Lubrication—pain with intercourse, no lubrication ii. Infection—herpes, yeast, HPV, warts iii. Scarring iv. Meds—Anticholinergic—anything that causes dry mouth will cause dry vagina e. Orgasm: anorgasmic i. Primary—never had—directed masturbation is treatment ii. Secondary Dr. Christensen 17/28 Transcription: Czubatyj 1. had, cannot have currently—often because of relationship 2. Sensate focus exercises—foreplay iii. 80% success rate XXV. Domestic Violence: a. Risk factors: i. Partner (they were abused, drugs, Alcohol), won’t leave, overly protective ii. Patient previously abused b. Signs/symptoms—hypervigilance—jumps when you enter the room, unexplained multiple injuries, partner won’t leave, overly protective c. Diagnosis—History, Injuries, inquire about partner d. Encourage patient to have plan for safety—follow up e. Most common outcome—patient goes back to abuser XXVI. Recurrent Pregnancy Loss (1st and 2nd trimester) 3 in a row a. Need at least 3 in a row before doctor is worried b. Causes: i. Karyotype ii. Infection—ureaplasm iii. Anatomy—uterus—Fibroids, septum iv. Immunology—Incompatibility v. Thrombophilia 1. Factor V leiden 2. Protein C andProtein S vi. 50% are unknown causes XXVII. IUFD: >20wks: a. Etiology: i. Unknown ii. Diabetes iii. Sepsis iv. Cord Accident v. Ruptured Membranes vi. Abruption b. Fibrinogen levels ↓ DIC c. Test Coagulation, PT, PTT, fibrinogen XXVIII. Placental Issues: Placental Abruption Placenta Previa Vasa Previa Placenta comes out before baby Placenta over cervix Uncovered vessels that can be easily ruptured Contraction with or without pain Painless bleeding Baby bleeds +/- Bleeding +/- Contractions Spotting/Fetal Distress DIC DIC—only when patient is about Sinusoidal pattern to die (late) Convaliar uterus No convalair uterus IUFD IUFD--late Risk Factors HTN AMA, previous uterine surgery Velametous insertion PIH, Chronic HTN Twins, Grand Multiparity Succentorial obe (extra lobe) Drugs (cocaine, alcohol, Smoking smoking) Fibroids, ↓Folate, Vena Cava Acreta, Increta, Percreta syndrome (deadly—labor and hematuria) Had one before Treatment: C/S for live birth Control bleeding, give steroids C/S Vaginal delivery if baby dead C/S Dr. Christensen 18/28 Transcription: Czubatyj XXIX. Rupture of Membranes: a. ROM—rupture of membances b. AROM—artificial rupture of membranes—you did it (+/- labor) c. SROM—spontaneous rupture of membranes (+ labor) d. PROM—premature rupture of membranes (no contractions) e. PPROM—premature previable rupture of membranes (<37 weeks, no contractions) i. Check for infection 1. Chorioamnionitis a. Mother: i. ↑temp, ↑ pulse ii. ↑WBC, ↑uterine tenderness iii. ↑pus b. Baby: i. Tachycardia ii. ↓variability—acidosis c. amnio: i. just like spinal tap ii. ↓glucose, ↑ protein, + WBC, IL-6 2. + : a. no tocolytics b. no steroids c. ? induction 3. Negative: a. tocolytics b. steroids f. Diagnosis: i. Nitrozine 1. pH paper + (↑pH 2. False + --sperm, blood, betadine, UTI ii. Ferning: 1. NaCl 2. 2nd 3rd trimester 3. False - --rupture has sealed, sample urine g. You can do transvaginal U/S on ROM and Placenta Previa—just don’t touch cervix h. Cannot culture Vaginal fluid—need a cervical culture, but check vaginal fluid for maturity XXX. Preterm Labor: a. Etiologyinfection of cervix and/or vagina b. Are they in labor—cervical change with contractions c. Infection: i. Yes: 1. Induce labor if mother is dieing 2. no interference otherwise ii. No: 1. tocolytics: a. Alcohol—BAL 300 (don’t use anymore) b. Β2 Mimetic i. Ritidrine—relaxes uterus, β1 crossover ii. Terbutaline—relaxes uterus, β1 crossover c. Mg Sulfate i. Ca antagonist ii. ↓ Respirations d. NSAIDS—Indomethacin i. ↓ Platelets, GI disruption—mother ii. Premature closer of ductus arteriosus—baby iii. Do not give after 34 weeks Dr. Christensen 19/28 Transcription: Czubatyj 2. Steroids: a. Prednisone—doesn’t cross placenta b. Β-methasone—affects mother and baby equally XXXI. Decels: a. Look at contraction and decal to see if they match b. Look if symmetrical c. Early—head compression d. Late—uteroplacentalinsufficiency e. Variable: i. Cord compression—low fluid on BPP—may try amnioinfusion ii. bad signs 1. Back to baseline very slowly 2. 60x60—60 beats in 60 seconds 3. Decel within a Decel f. tachycardia: i. >160 bpm ii. fever (maternal of fetal) iii. ↓variability—acidosis iv. Late Decel + ↓ Variability—baby usually born braindead XXXII. Mortality: a. Direct Maternal—Directly caused by pregnancy—PE, etc b. Indirect Maternal—underlying disease caused death while pregnant c. Nonmaternal—trauma, nothing to do with pregnancy XXXIII. BPP (biophysical profile) a. 41 weeks—NST looking for accelerations i. Reactive—repeat in 3-5 days ii. Nonreactive—try VAS (vibratory acoustic stimulation) 1. if becomes reactive—repeat in 3-5 days 2. nonreactive: a. BPP: i. NST ii. Movement iii. Tone iv. Breathing v. AFI vi. 10/10 theoretically best, 8/8 in real life 1. 8/8 because of NST 2. worried if AFI is low—baby problem or ruptured—Deliver if term b. Contraction Stress Test (oxytocin Challenge Test) give PIT i. Looking for 3 contraction in 10min ii. Late/NR--+ OCT—deliver—50% false + iii. No late, Reactive—negative c. If nonreactive—No delivery—DO BPP b. >42 weeks: i. Macrosomia 1. Labor dystocia 2. ↑C/S 3. Shoulder dystocia 4. DM—4000-4500, otherwise its 4500-5000 (grams) ii. Uteroplacental insufficiency: 1. programmed suicide in cells—placenta begins to die off 2. ↓ BP--↑Fetal distress (severe Lates) 3. meconium, ↑Fetal death (IUFD) 4. dysmature baby—looks like YODA (long hair, long fingernails XXXIV. IUGR: Dr. Christensen 20/28 Transcription: Czubatyj Assymetric Symmetric <10th procetile Late Early (organogenesis) Nutritional problem (HTN, Drugs, PIH, Vascular Infection( TORCH)/Karyotype (aneuplody) Disease Toxo, other, rubella, CMV, herpes a. Fluid: i. Normal: 1. Assymetric—small baby, ↑calorie 2. Symmetric—small baby ii. Low:--problem no matter if asymmetric or symmetric b. <20 weeks--↓fluid—test Karyotype (make sure baby is viable) otherwise no need to test for infection XXXV. Postdates: >42 weeks a. Etiology: i. Incorrect dates 1. bad GYN history 2. Irregular cycle ii. Smoking is not part of it…will cause earlier delivery iii. ZEBRAS: 1. abdominal pregnancy a. induced labor—nothing happens b. C/S c. Don’t remove placenta d. Remove baby, clamp cord 2. Hormones: a. Fetal AnencephalyNo fetal brain—no trigger for labor b. Sulfatase ↓--↓Estrogen—no labor c. Fetal Adrenal Hypoplasia—no estrogen XXXVI. Graphs: I. Freidman curves o Normal: 10 Dilation Station Active 0 -3 Plateau Latent 0 +3 Dr. Christensen 21/28 Transcription: Czubatyj o Abnormal dilation 10 Plateau Arrest of dilation Dilation Prolonged latent Active Protracted active Latent 0 +3 o Abnormal descent -3 Station Failure to descend 0 Arrest of descent +3 XXXVII. a. Post Partum Hemorrhage: Early—in delivery room: Dr. Christensen 22/28 Transcription: Czubatyj i. Atony—prolonged labor, pit, infected uterus, grand multiparity ii. Massage uterus—meds 1. Pit—like ADH--hyponatremia 2. Methergine a. HTN b. LSD like c. Psychosis 3. PGF2α: a. Asthma b. Hemo + rate b. PGE: i. 1—cervical ripening ii. 2—cervical ripening iii. Both induce labor c. PGF2α: i. Causes contraction ii. Never use on viable pregnancy XXXVIII. Necrotizing Fascitis: a. Increased T, wound infection, blistering, pain, worst sign is loss of pain b. Everything scoops off muscle in debridement but muscle is intact c. 2 types: i. Type 1—group A strep ii. Type 2—mixed d. Treatment—radical debridement in the OR e. Do NOT bleed f. RF—DM, HTN, source of infection XXXIX. Stats: a. Errors: i. Type I (false positive error)—falsely rejecting the null hypothesis ii. Type II (flase negative error)—falsely accepting the null hypothesis (worse because no one will go back and retest b. Level of Evidence: i. I—gold standard—randomized control trial ii. II-1—controlled randomized iii. II-2—retrospective and prospective studies iv. II-3—dramatic series/time series v. III—opinions of respected experts c. Quality of Evidence: i. A—strong support for ii. B—fair support for iii. C—neither—level of support of most things done in medicine iv. D—fair support against v. E—strong support against d. 2x2 table DRAW on BACK) i. specificity ii. sensitivity iii. PPV iv. NPV v. Accuracy e. prospective study: i. look at smokers and nonsmokers and see who gets lung ca ii. analysis by RR (risk you smoke/risk you don’t smoke) iii. Attributable risk = R smoking – R nonsmoking f. Retrospecive study: i. Look at those who got lung ca, see who smoked and look at those who didn’t get lung cancer, look who smoked Dr. Christensen 23/28 Transcription: Czubatyj XL. XLI. ii. Analysis by OR = odds you smoked/ odds you were a nonsmoker Infertility: a. Definition i. Attempting conception for 1 year (85% will conceive on their own) ii. AMA is exception (>35yo) send to specialist iii. Primary—never conceived iv. Secondary—had kids, but can’t now b. Factors: c. Cervix—Post Coital Test—Spiteterkeit*?—mucus stretches at ovulation d. Uterus—Histosalpingogram (HSG), Hysteroscopysurgery e. Tubes—HSG, Tubal Dye Perfusion—tubalplasty, Tubal bypass (Invitro Fertilization) f. Ovaries—Ovulation—Basal Body Temp (BBT) i. ↑ temp caused by progesterone 1. Figure out day, subtract 2—day of ovulation 2. PCO? If alatory ii. Ovulation Induction: 1. Clomefine 2. side effects a. hyperstimulationmultiple gestations b. OHD—ovarian hyperstimulatory Disease—looks like ovarian Ca g. Periteneum—Laparoscopy, Lupron i. Adhesions ii. Endometriosis h. Male—semen analysis (check twice) i. NEVER Do anything invasive until Male Factor is Ruled Out Contraception a. Sterilization i. Male is better than female, and cheaper ii. Hysterectomy never used for sterilization b. hormonal: i. efficacy vs. effectiveness ii. theoretical vs actual iii. types: 1. OCP— a. ↓ effectiveness (forget to take). ↑DVT, Factor V leiden, Vascular Disease, ↑ Mi, ↑CVA, ↓ endometrial and ovarian CA, ovarian cysts, ↓bleeding, ↓dysmenorrhea b. Do not give tosmokers >35yo 2. Depo-provera--↑effectiveness—weight gain—about 8lbs—contra DM 3. Patch—like OCP—No 1st pass, no liver effect 4. Ring—like OCP—no 1st pass, no liver effects 5. Norplant—5 years, Levoprogesterone c. IUD: i. Copper—Paraguard—Few failures, no change in risk for ectopic or PID, 10 yrs, no benefit for bleeding, ↓sperm motility, capacitation ii. Progesterone—Progestasert--↑Failure, 1 year, ↑ectopic, ↓dysmenorhea, ↓blood loss, thickens mucus, atrophies endometrium, Unilteral TOA, actinomyces israelii iii. Levoprogesterone—Mirena—like progersterone, 5 yrs, no change for ectopics d. Barrier: 85% effectiveness i. Diaphragm 1. Cystitis 2. TSS ii. Sponge—Nanoxidil 9—Vaginal ulcers--↑HIV risk iii. Condom—High failure rate—used incorrectly—Latex allergy Dr. Christensen 24/28 Transcription: Czubatyj iv. Cervical Caps—cervical dysplasia Rhythm <85% i. Calender—regular cycle—block off 2 weeks for ovulation ii. BBT--↑temp—day before is ovulation iii. Spinnbarkeit—check cervical mucus XLII. Abortion: a. 1st trimester: >8wks i. D+C suction 1. very few risks, post aborted syndrome= retained productsrepeat D+C 2. if + Chlamydia/GC—can spread infection into tubes—PID 3. post abortion regret—Informed consent—give patient all options ii. RU 486: 1. Antiprogestin—1st 42 days—does not cause expulsion 2. give with PGEexpulsion 3. 15% need D+C anyway iii. MTX iv. “Menstrual Extraction” 1. D+C done in 1st 6 weeks of pregnancy 2. good chance of missing pregnancy 3. pregnancy then continues 4. limb reduction defects b. 2nd trimester: i. D+E 1. Dilation and extraction 2. surgical complications ii. PG induction PGE, PGF2α 1. Fever 2. N/V 3. live born—KCl—kills baby, inject into heart 4. do not give PGF2α with asthma iii. Urea/Saline injection—DIC, PE, Shock, Death—high complication rate iv. Hysterectomy—extreme XLIII. Vaginitis Org Discharge pH Whiff Saline KOH Tx White, mid 4.5 Neg Lacto Neg None Lacto cycle normal Thin, grey, >4.5 +--fishy Clue cells Neg Metronidizole BV sticky, foul smelling Green, >4.5 +/Trich Neg Flagyl Trich bubbley, Pear shaped Metronidizole “strawberry Maybe treat cervix” partner also Cottage <4.5 Neg Spores, Spores Difluconazole Yeast cheese/ no hypahe…1/3 hypahe (1/3 (diflucan) discharge, not visible not visible) Imidazole just itching Watery, >4.5 Neg WBC Neg Estrogen Atrophic clear e. XLIV. Ulcers: a. Painful: i. HSV—multiple small ulcers (2-3mm) ii. Chancroid—1 or 2 large ulcers (>1cm) iii. Behcet’s 1. eyes Dr. Christensen 25/28 Transcription: Czubatyj 2. 3. b. VDRL + + - Painless: i. Syphilis—chancre 1. Diagnosis a. Dark field b. VDRL, FTA FTA + + 2. XLV. mouth perineum stages: a. b. c. d. Untreated syphilis Biological false + for syphilis Treated syphilis No symptoms or early infection/not infected primary—chancre secondary—rash, fever, lymphadenopathy, murmur Latent no symptoms, infectious for 1 year tertiary: i. organ damage ii. AA—abdominal aneurysm—athersclerosis iii. TT—trunkal aneurysm—treponem 3. Treatment: a. Penicillin alone is not ok—needs to be long lasting b. Bicillin—PCN in oil or IV PCN (14days—ofen for tertiary) c. PCN allergy i. Tetracycline—teeth problems in fetus ii. Erythromycin—macrolide—does not cross placenta d. Pregnancy and PCN allergy i. ICU and desensitize ii. LGV—Lymph Granular Venerum 1. Chlamydia 2. painless ulcer + lymph clumping (bubore—lymph coalesce into a big one) iii. Granuloma Inguinale 1. chamylla bascterium 2. Bleeding painless ulcer iv. CANCER 1. 60yrs old—top of list 2. 20yrs old—not c. Non cancerous vulvar lesions: i. Lichen sclerosis—caused by lack of estrogen (kids and post menopausal) 1. white patch, itchy 2. Commonly referred as onion skin or tissue paper 3. treatment—steroid cream ii. Paget’s Disease—is a CIS 1. if on nipple—find cancer underneath about 100% of the time 2. if on vulva—find cancer underneath about 15% of the time 3. red scaly itchy 4. Commonly referred to as cake frosting or cake icing Cervicitis: a. Silent i. GC and Chlamydia—found during prenatal care ii. For G/C ceftrioxone + doxycycline (for chlamydia) (+zithromax if pregnant, doxy) b. Mucopurelent Cervicitis i. pus coming out of cervix Dr. Christensen 26/28 Transcription: Czubatyj ii. No other signs of PID iii. G stain—WBS—chalmydia—Doxy iv. G+ diplococci c. If GC is positive treat for both GC and chlamyia (ceftrioxone + doxy) d. If Chlamydia is only + just trat Chlamydia (doxy) XLVI. PID: a. Risk Factors: i. Age—risk ↑ when younger ii. Exposure iii. Menstruation (GC follows flow during/after cycle) iv. Contraception (↓PID)—OCPs b. Diagnosis: Laparoscopy is gold standard i. Big 3: 1. cervical motion tenderness 2. Lower abdominal tenderness 3. Adnexal tenderness ii. >1 of the following: 1. Fever, ↑WBCs, ↑sed rate 2. Discharge, abnormal bleeding, + culture 3. Mass on U/S, pus in culdesac iii. 50% diagnostic accuracy c. What to do: i. Indications for admission: 1. Tried outpatient therapy but failed 2. Can’t tolerate PO 3. sepsis—severe illness (↑P, ↓urine, etc) 4. Pregnancy 5. IUD 6. HIV 7. first episode 8. nulliparity—no longer on the list 9. Uncertain diagnosis—Appendicitis a. CT b. Compression U/S ii. When admitted: 1. Regiment A: a. Cefaoxitin + doxy b. Ceflotetan c. “Foxy Doxy” 2. regiment B (Gent/Clinda/Amp—triples 3. Outpatient—Ceftraoxone + Doxy iii. Consequences: 1. Ectopics, infertility—chlamydia, chronic pelvic pain, recurrent/chronic PID—end up with hysterectomy that doesn’t alleviate pain 2. Note—if have Chlamydia in a pregnant woman treat with azithromycin XLVII. Incontinence: Etiology Diagnosis Treatment UA, C+S not needed if 1st time E.coli—sulfa, cephalosporin, UTI macrodantan Anti-cholinergic Spastic bladder Cystometrogram (pressure spikes when filling bladder with fluid Urge incontinence Post void residual >50 in cath Self Cath, treat DM Neurogenic bladder Physical Exam Remove mass Pelvic Mass (preg, Fibroids) Dye test (cause surgery in US, Surgery Fistula (continuous leaking) preg in world) True incontinence Exam—atrophy, thinning of Unknown Atrophy, post menopausal Dr. Christensen 27/28 Transcription: Czubatyj Stress incontinence folds, etc Hypermotile urethra, bulges when cough (qtip test) Retropelvic urethroplexy XLVIII. Endometriosis a. Polygenic, multifactorial—unknown—related to immunology b. Retrograde mentration—cervical stenosis (cones/LEEPs) c. Implantation—Lap scar, episiotomy scar d. Metaplasia—perineum turning into endometrium e. Heme/Lymph spread—pulmonary endometriosis Endometriosis Adenomyosis External to uterus Internal to uterus Growing outside uterus Growing in myometrium Sx—pain, dysmenorrheal, dyspareunia, adnexal Sx—pain, dysmenorrheal, dyspareunia, fertile tenderness, fixed uterus, nodules on culdesac, (previous C/S) enlarged, tender, boggy uterus infertile Dx—laparoscopy Dx—US or MRI Tx—laser therapy or HRT Tx—hysterectomy Bleeding—1/3 patients Bleeding is main reason for visit Causes: Cause is unknown for sure—Labor, C/S, surg 1)retrograde menstruation (cervical stenosis) 2)Implantation (prev surgery) 3)Lymph/heme spread (cyclic hemoptysis) 4)metaplasia (people with no uterus— mullerian agenesis 5)Immune surveillance (immune suppressed) XLIX. Pelvic Pain: a. GYN: i. Endometriosis—Laparoscopy--Lupron 1. Infertility, Dysmenorhea 2. uterus small, tender ovaries ii. Adenomyosis--hysterectomy 1. bleeding, bleeding, bleeding 2. Anemia, clots, tender, bogy uterus iii. adhesions: 1. tender pelvic exam 2. PID/infertility iv. Fibroids—don’t usually cause pain v. cysts b. Non-GYN: i. Spastic cholitis/ IBS 1. alternating constipation/diarrhea with gas 2. bloating, cramping ii. Interstitial Cystitis:--inflamed bladder wall 1. Pelvic pain, urgency, frequency 2. negative UA 3. diagnosis—K test—pain with K in bladder or cystoscopy 4. Tx—DMSO/elmiron iii. Muscoloskeletal iv. Carnett’s sign—tense abdominal wall, pain gets worse 1. if positive—hernia, trigger point 2. of negative—visceral Dr. Christensen 28/28 Transcription: Czubatyj 3. L. Remember tha spigellian hernia occurs at the lateral border of the rectus muscle v. SIGECAPs—depression (5 for 2wks) vi. History of ↑ incidence of abuse/violence Impaired Physicians: a. Must report intoxication, is a law in MI b. At night can report to charge nurse c. During day can report anonymously through various avenues d. If you are intoxicated and call in—you should call a colleague e. Criteria for drug dependence—works for any addictions i. Craving ii. Lose control iii. Do despite consequences