Common causes of left-sided heart failure
advertisement
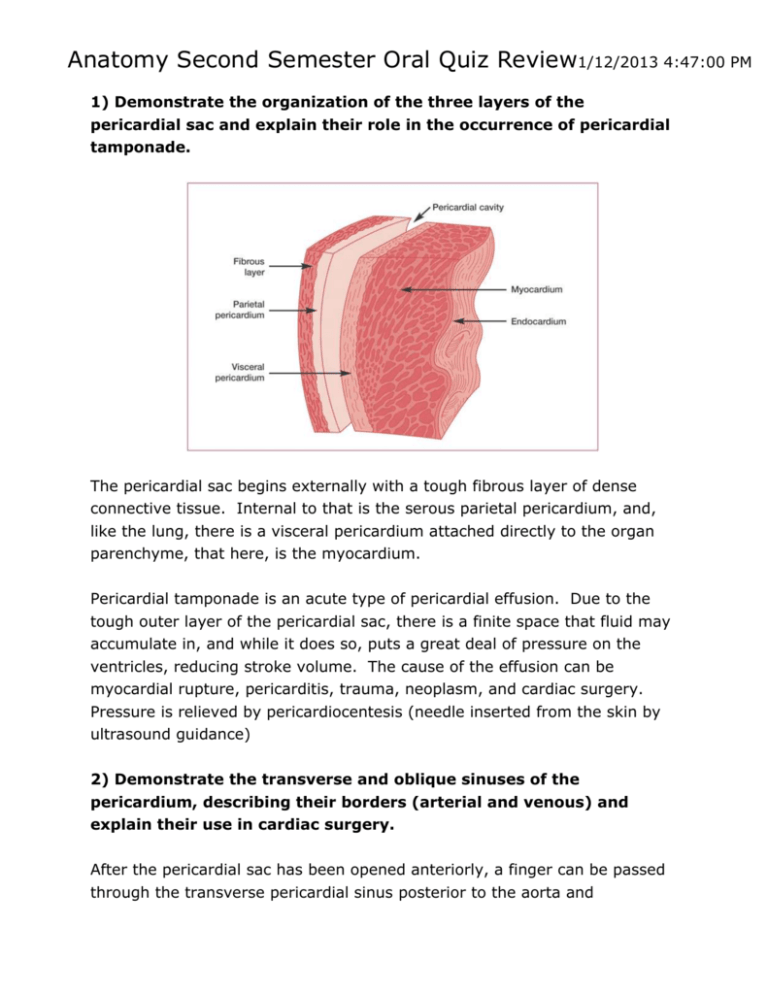
Anatomy Second Semester Oral Quiz Review1/12/2013 4:47:00 PM 1) Demonstrate the organization of the three layers of the pericardial sac and explain their role in the occurrence of pericardial tamponade. The pericardial sac begins externally with a tough fibrous layer of dense connective tissue. Internal to that is the serous parietal pericardium, and, like the lung, there is a visceral pericardium attached directly to the organ parenchyme, that here, is the myocardium. Pericardial tamponade is an acute type of pericardial effusion. Due to the tough outer layer of the pericardial sac, there is a finite space that fluid may accumulate in, and while it does so, puts a great deal of pressure on the ventricles, reducing stroke volume. The cause of the effusion can be myocardial rupture, pericarditis, trauma, neoplasm, and cardiac surgery. Pressure is relieved by pericardiocentesis (needle inserted from the skin by ultrasound guidance) 2) Demonstrate the transverse and oblique sinuses of the pericardium, describing their borders (arterial and venous) and explain their use in cardiac surgery. After the pericardial sac has been opened anteriorly, a finger can be passed through the transverse pericardial sinus posterior to the aorta and pulmonary trunk. The transverse pericardial sinus is between the venous and arterial mesocardia, namely, the ascending aorta and pulmonary artery cranio-ventrally and the superior vena cava dorsally. The transverse pericardial sinus is especially important to cardiac surgeons. By passing a surgical clamp or placing a ligature around these vessels, inserting the tubes of a coronary bypass machine, and then tightening the ligature, surgeons can stop or divert the circulation of blood in these large arteries while performing cardiac surgery. The oblique pericardial sinus lies posterior to the heart (dorsal) and is bounded Anteriorly by serous pericardium of the left atrium Posteriorly by the parietal pericardium of the pericardial sac Superiorly and laterally by the reflection of serous pericardium around the four pulmonary veins, SVC & IVC Lift the apex of the heart and place fingers posterior to the heart to identify the oblique pericardial sinus. This space is utilized during cardiac surgery to manually massage and manipulate the heart. 3) Demonstrate the four borders of the heart seen in the anterior view (inferior, superior, left or right pulmonary) and describe the structures composing each border. Right border (from superior to inferior) SVC Right atrium IVC Left border (from superior to inferior) Arch of the aorta (aortic knob on film) Pulmonary trunk (knob) Left auricle Left ventricle 4) Demonstrate the four surfaces of the heart (anterior, posterior, left & right lateral, inferior & superior) ….[that’s six for those counting] and describe the structures composing each surface. Superior: where the great vessels are located Inferior (floor): directed downward and dorsally, is formed by both ventricles and rests on the central tendon Right Lateral: Right atrium, ventricle and vena cavae Left Lateral: Left auricle, atrium and ventricle Posterior: Left atrium, vena cavae, pulmonary veins, coronary sinus Anterior: The apex of the heart, formed by both ventricles, and the left auricle and right atrium compose the anterior aspect of the heart. 5) Demonstrate the components present in the right atrium and right ventricle and explain the clinical aspects of right sided failure. The right atrium receives venous, oxygen-poor blood, from the systemic circulation via the superior vena cava (SVC), inferior vena cava (IVC), and (posteriorly) the coronary sinus. The pectinate muscles extend from the crista terminalis (vertical muscular ridge on the internal surface of the anterior right atrial wall.) The fossa ovale is also visible, a region of the interatrial septum, which, in the patient’s embryonic life, served as a rightto-left shunt, known as the foramen ovale. The smooth interior portion of the anterior right atrial wall is what remains of the sinus venarum. The right ventricle receives from blood from the right atrium via the tricuspid valve. The chordae tendineae are ligaments that connect each cusp to the papillary muscles, allowing them to open when the papillary muscles are contracting. The valve has a septal, anterior and posterior valve. Tracking the anterior papillary muscle inferiorly, one can locate the muscular moderator band (aka septomarginal trabeculae) and follow it to the ventricular septum. The moderator band carries the right bundle branch from the AV node. The trabeculae carnea is the term for the musculature of the right ventricular wall. The conus arteriosus is the narrowing, smooth walled portion of the ventricle located left and superiorly, leading to the pulmonary valve, which also has three cusps; anterior, right and left cusps. When the right ventricle begins to lose efficiency (losing ejection fraction) Common clinical symptoms of right-sided heart failure: Dyspnea Peripheral edema Jugular vein distension (JVD) Nocturia Hepatomegaly Common causes of right-sided heart failure: Coronary artery disease (CAD) Left-sided heart failure COPD or chronic bronchitis / emphysema alone Congestive Heart Failure (CHF) Pulmonary embolism (PE) Valvular disease / damage / defect Anemia (associated) Hyperthyroidism 6) Demonstrate the components present in the left atrium and left ventricle and explain the clinical findings in left sided failure. The left atrium receives oxygen-rich blood from the pulmonary venous system (2 veins per lung). These pulmonary veins dump into the posterior region of the left atrium. The left atrium lack pectinate muscles. Blood passes from the left atrium to the left ventricle via the mitral valve (aka bicuspid valve). The left ventricle receives oxygen-rich blood and is responsible for pumping that into the systemic circulation. With a much thicker myocardium than the right ventricle, the left also has two papillary muscles, (one per mitral cusp). Blood is ejected through the aortic (semilunar) valve into the ascending aorta. From the ascending aorta, you can see the 3 sac-like depressions called aortic sinuses. From these sinuses you can find the coronary artery and vein branch points. Left-sided heart failure is associated with these symptoms & findings: Increased work to breath Rales or crackles upon auscultation (lung bases) Cyanosis Cough, frothy Hemoptysis Needs to elevate head Decreased urine production Fatigue, weakness Paraoxysmal nocturnal dyspnea Weight gain Laterally displaced heart apex beat Gallop rhythm Common causes of left-sided heart failure: MI Myocarditis High blood pressure Valvular damage, defect, disease Hypothryroidism 7) Demonstrate the course of the great vessels in and out of the heart and explain the two ‘crosses’ present in the heart. Identify them on your own heart: Pulmonary veins Pulmonary arteries Ascending aorta Inferior & Superior Vena Cavae The two crosses of the great vessels are (1) between the pulmonary veins and the vena cavae and (2) aorta and the pulmonary trunk (45° from floor) (Thanks reader) 8) Describe and identify the sites of auscultation of the cardiac sounds on your partner. A(ortic) region: Between 2nd & 3rd intercostal spaces, immediately lateral to sternum (RUSB) P(ulmonary) region: Left 2nd intercostal space, immediately lateral to sternum (LUSB) T(ricuspid) region: 4th to 6th intercostal spaces, at lower left sternal border (LLSB) M(itral) region: between 5th and 6th intercostal spaces on the left mid-clavicular line