Dissection 20, Pericardium and Heart
advertisement

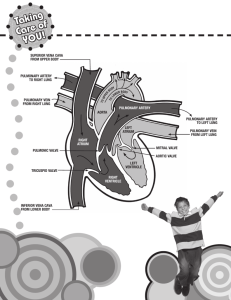
DISSECTION 20 The Pericardium and the Heart References: M1 128-160, 171-173; N 207-221; N 211-225; R 242-253, 257-271 AT THE END OF THIS LABORATORY PERIOD YOU WILL BE RESPONSIBLE FOR THE IDENTIFICATION AND DEMONSTRATION OF THE STRUCTURES LISTED BELOW: 1. Structures associated with the pericardium and pericardial sac: fibrous pericardium, parietal layer and visceral layer (epicardium) of the serous pericardium, transverse pericardial sinus, oblique pericardial sinus, pericardial cavity. 2. Features of the exterior of the heart: base, apex, diaphragmatic surface, sternocostal surface, acute margin, obtuse margin, anterior interventricular sulcus, posterior interventricular sulcus, atrioventricular (coronary) sulcus, right atrium and right auricle, left atrium and left auricle, right ventricle, left ventricle, conus arteriosus. 3. Arteries: right coronary, artery of the sinoatrial node, right marginal, posterior interventricular, left coronary, anterior interventricular, circumflex, pulmonary trunk, aorta, aortic sinus. 4. Veins: great cardiac, coronary sinus, middle cardiac, small cardiac, anterior cardiac, openings of least cardiac veins, pulmonary veins, superior vena cava, inferior vena cava. 5. Features of the interior of the heart: interatrial septum, sinus venarum, fossa ovalis and its limbus, orifice and valve of inferior vena cava, orifice and valve of coronary sinus, crista terminalis, musculi pectinati, supraventricular crest, pulmonary valve (valvule, nodule, lunula, commissure), tricuspid valve (commissures, anterior, posterior, and septal cusps, chordae tendineae, anterior, posterior, and septal papillary muscles), trabeculae carneae, septomarginal trabecula, mitral valve (anterior and posterior cusps, chordae tendineae, anterior and posterior papillary muscles), interventricular septum (pars muscularis, pars membranacea), aortic valve (valvule, nodule, lunula, commissure), openings of the coronary arteries. YOU SHOULD ALSO BE ABLE TO DO THE FOLLOWING THINGS: 1. Describe or draw the surface projection of the heart on a diagram of the anterior thoracic wall. On this projection show the location of the four valves. 2. Locate the sinoatrial and atrioventricular nodes. Trace an impulse from the sinoatrial node to either ventricle, naming in order the components of the conducting system traversed. 3. Describe the pathway of blood flow through both fetal and adult hearts. 4. Trace the route of blood flow to various parts of the myocardium and back to the right atrium naming in order all vessels traversed. 5. Identify the various heart chambers, borders, etc. on X-rays of the heart. Dissection 20, Pericardium and Heart Page 2 LEFT VENTRICLE and APEX of the heart, and ANTERIOR INTERVENTRICULAR GROOVE the or sulcus. The right ventricle forms most of the sternocostal and part of the DIAPHRAGMATIC SURFACE of the heart. The left surface is composed mainly of the left ventricle. Also locate the positions of the SUPERIOR VENA CAVA and the INFERIOR VENA CAVA. Expose the pericardial sac fully by pulling the mediastinal pleurae aside. Expose the heart widely by making superior and inferior transverse incisions connected by a vertical incision through the pericardium. The PERICARDIAL CAVITY is a narrow interval between the external surface of the heart and the internal surface of the pericardial sac. In the cadaver this is sometimes filled with a coagulation of fluid present before death or an effusion of the embalming fluid. Like the pleura, the pericardium is composed of a parietal portion and a visceral component (G1.44A; N208; N212). The VISCERAL PERICARDIUM is frequently referred to as the EPICARDIUM. The PARIETAL PERICARDIUM has an external fibrous layer, called the FIBROUS PERICARDIUM (N194; N198), that is firmly attached to the diaphragm below and to the outer layer of each great vessel entering or leaving the pericardial sac. The fibrous sac is also attached to the deep surface of the sternum by the sternopericardial ligaments (composed of condensations of mediastinal connective tissue). The serous lining of the pericardial sac (parietal pericardium) reflects upon the heart as the epicardium. What layers separate the pericardial cavity laterally from the pleural cavity? Where are the visceral and parietal layers of the pericardium continuous? For orientation of the heart within the pericardial cavity, identify the following structures with reference to atlas figures (G1.43, 41A; N208; N212; A192-193); the RIGHT ATRIUM, the RIGHT AURICLE, and the RIGHT VENTRICLE with its outflow tract, the PULMONARY TRUNK; the LEFT ATRIUM, the Pass your fingers upward behind the heart; they are stopped in a cul-de-sac of pericardium known as the OBLIQUE SINUS, formed by the reflection of parietal pericardium to the epicardium along the line of entrance of the major veins into the heart. Identify each vein by name as you encounter it. Next, place your fingers in front of the atria and behind the AORTA and PULMONARY TRUNK where they lie in the TRANSVERSE SINUS of the pericardium (G1.44, 53; N211; N215; A193, 194). Replace the chestplate and review the projection of the outline of the heart on the anterior thoracic wall. Where would you palpate the maximal impulse (apex)? Where would you listen for the sound of the mitral valve? Next review the features of the interior of the pericardial sac. What is the name of the space between the atria and the arterial outflow tracts of the ventricles (pulmonary trunk and aorta)? Using atlas figures as a guide (G1.43, 41; N208; N212; A193) identify on the heart in situ the CONUS ARTERIOSUS or infundibulum, PULMONARY TRUNK, AORTA, LEFT ATRIUM, PULMONARY VEINS, LEFT AURICLE, RIGHT ATRIUM, SUPERIOR VENA CAVA, INFERIOR VENA CAVA, and RIGHT AURICLE. What is an auricle? How is an auricle distinguishable from an atrium? Identify the ATRIOVENTRICULAR (coronary) GROOVE or sulcus and the ANTERIOR and POSTERIOR INTERVENTRICULAR SULCI. Note the APEX (apex of left ventricle), RIGHT VENTRICLE, LEFT VENTRICLE, and the ACUTE (right) and OBTUSE (left) MARGINS of the heart. Locate the RIGHT and LEFT CORONARY ARTERIES (G1.43, 45; N211, 212; N215, 216; A195) arising from the aorta just distal to the aortic semilunar valve. Dissection 20, Pericardium and Heart Page 3 Note: At odd-numbered tables, the heart is not to be removed from the cadaver but is to be studied in place in order to retain as many of the relationships as possible. It may be necessary to refer to excised hearts to visualize some of the structures called for below. Dissectors at the even-numbered tables should remove the heart by transecting the INFERIOR VENA CAVA, the PULMONARY VEINS, the AORTA, the PULMONARY TRUNK, and the SUPERIOR VENA CAVA within the pericardial cavity (G1.44B; N208; N212; A194). With the heart removed review the internal features of the pericardial sac, identifying in turn the orifices of the severed vessels. Be sure that you can replace the heart in its normal position in order to review its relationships with adjacent thoracic structures. (Note: In the excised hearts, identify the aortic and pulmonary valves described below.) Expose the internal features of the heart by cutting: (1) the anterior surface of the right atrium laterally, just above the right coronary artery in the coronary sulcus; (2) the right ventricle just below the right coronary artery in the coronary sulcus (in excised hearts this ought to begin at the cut pulmonary trunk and pass between the left and right valvulae of the pulmonary valve, (G1.54; N216; N220) continuing along the base of the ventricle, leaving the right coronary artery intact); (3) the right ventricle again just to the right of the anterior interventricular sulcus (in hearts remaining within the body, this incision should begin by curving to the left, from the top of cut (2), pass to the interventricular septum, and extend to the apex of the right ventricle on the right side of the septum. In excised hearts begin at the cut pulmonary trunk and extend the cut between the anterior and right cusps of the pulmonary valve (G1.53; N218; N222); (4) the left ventricle to the left of the anterior interventricular sulcus passing to the right of the anterior interventricular artery to the apex of the heart (in excised hearts this should begin in the commissure between the left and right cusps of the aortic semilunar valve, and for in situ hearts the incision ought to be extended through this commissure into the ascending aorta); (5) the posterior surface of the left atrium just above the coronary sulcus, extending the ends of the incision superiorly to the cranial border of the chamber but avoiding the openings of the pulmonary veins. Clean the major branches of the CORONARY include the ARTERY TO the RIGHT MARGINAL ARTERIES. These should THE SINOATRIAL NODE, and the POSTERIOR INTERVENTRICULAR branches of the right coronary artery and the ANTERIOR INTERVENTRICULAR and CIRCUMFLEX branches of the left coronary artery. In the atrioventricular sulcus on the posterior surface of the heart (G1.45), locate the CORONARY SINUS (G1.46, 44A; N210; N214; A197, 200) and clean its tributaries: the SMALL CARDIAC VEIN, the MIDDLE CARDIAC VEIN, and the GREAT CARDIAC VEIN. Also look for ANTERIOR CARDIAC VEINS (G1.43; N212; N216; A195) draining directly into the right atrium from the right margin of the right ventricle. Begin the study of the interior of the heart with the right atrium. Remove any clotted blood which remains within the cavity. Note that the posterior wall of the right atrium is smooth (G1.49; A206, 207). This is the SINUS VENARUM, demarcated by the CRISTA TERMINALIS from the Dissection 20, Pericardium and Heart Page 4 anterior wall which is marked by MUSCULI PECTINATI. Identify the OPENINGS of the SUPERIOR VENA CAVA and the INFERIOR VENA CAVA. Between these, in the INTERATRIAL SEPTUM, is an oval depression, the FOSSA OVALIS, the margin of which is known as the LIMBUS. Locate the opening of the CORONARY SINUS anterior to the fossa ovalis, and note that this aperture as well as that of the inferior vena cava is guarded by a small flap known as a VALVE. The TRICUSPID or RIGHT ATRIOVENTRICULAR ORIFICE forms the communication between the right atrium and the right ventricle. ovalis. Examine the atrial septum to determine if any communications exist between the right and left chambers. Within the right ventricle, identify the SEPTAL, ANTERIOR, and POSTERIOR CUSPS of the TRICUSPID VALVE (G1.50; N216; N220; A207-208). Locate the ANTERIOR, POSTERIOR and SEPTAL PAPILLARY MUSCLES and the CHORDAE TENDINEAE which attach them to the valve cusps. Much of the surface of the ventricle presents rough bands of muscle known as TRABECULAE CARNEAE. A particularly prominent one passing from the interventricular septum to the base of the anterior papillary muscle is the MODERATOR BAND (septomarginal trabecula). The narrow superior part of the right ventricle below the PULMONARY VALVE is the CONUS ARTERIOSUS. Its walls are relatively smooth, and it is marked off from the rest of the cavity by a transverse ridge, the SUPRAVENTRICULAR CREST. The interior of the left atrium is smooth. Locate the valvule of the foramen ovale which forms the floor of the fossa Identify the AORTIC VALVE as three cupshaped VALVULES (G1.57B, 1.55A; N219; N223; A209). The free edge of each valvule has a slight thickening near its middle (the NODULE). LUNULES of adjacent valvules attach to the walls of the vessel at a point known as a COMMISSURE. Identify the AORTIC SINUS, and the ORIFICES of the CORONARY ARTERIES (G1.52A; N219; N223; A210, 217) noting the valvule with which each is associated. Follow the aorta through its valve into the LEFT VENTRICLE and locate the MEMBRANOUS PORTION of the INTERVENTRICULAR SEPTUM beneath the valvule that does not have a coronary artery opening associated with it. Note that the wall of the left ventricle is also marked by TRABECULAE CARNEAE. Identify the ANTERIOR and POSTERIOR CUSPS of the MITRAL(left atrioventricular) VALVE. These are attached to ANTERIOR AND POSTERIOR PAPILLARY MUSCLES by CHORDAE TENDINEAE. In all four chambers of the heart, note OPENINGS OF THE LEAST CARDIAC VEINS. Finally, attempt to trace the conduction pathway on your specimen by reference to G1.56; N219; N223; A215-218. You will not be able to visualize the actual components of the conduction system (except for the moderator band), but you ought to be aware of the location of the major elements of the system. STUDY QUESTIONS ON NEXT PAGE Dissection 20, Pericardium and Heart Page 5 STUDY QUESTIONS 1. Define the following terms: 1. Epicardium Visceral pericardium. Sternocostal surface of the heart Principally formed by the right ventricle; that part of the heart facing the sternum, costal cartilages, and ribs. Oblique sinus Blind segment of pericardial sac bounded by the reflection of the serous parietal to the visceral pericardium around the pulmonary veins and the venae cavae. Transverse sinus Part of the pericardial sac located between the atria and the great vessels. Endothoracic fascia Connective tissue which attaches the parietal pleura to the thoracic wall. 2. What are the boundaries of the anterior mediastinum? 2. Anterior - central portions of body of sternum and transversus thoracis muscle. Posterior - central part of anterior wall of pericardial sac. Lateral - anterior part of mediastinal pleura. Inferior - anterior part of diaphragm. Superior - anterior part of imaginary line from sternal angle to intervertebral disc between T4 & T5. 3. What are the contents of the middle mediastinum? 3. The contents of the middle mediastinum include the contents of the pericardial sac and a few structures in contact with it: heart; pericardium; ascending aorta; pulmonary trunk; roots of the lungs; and tracheobronchial lymph nodes. In addition, parts of the following are also considered to lie within the middle mediastinum: superior vena cava; pulmonary veins; azygos vein; phrenic nerves; and pericardiacophrenic vessels. 4. What are the locations of the cell bodies of the fibers in the phrenic nerve? 4. Cell bodies of efferent fibers to skeletal muscle (diaphragm) are located in the anterior gray column of the third, fourth, and fifth cervical segments of the spinal cord. Afferent fibers (from diaphragm and mediastinum) have their cell bodies in the dorsal root ganglia of C3, 4 and 5. Postganglionic efferent fibers (to blood vessels) arise from cells in the upper two ganglia of the cervical sympathetic trunk. Dissection 20, Pericardium and Heart Page 6 5. What types of fibers, functionally and structurally, are found in the cardiac plexus? 5. The cardiac plexus contains three types of fibers. These are afferent, preganglionic efferent (parasympathetic), and postganglionic efferent (sympathetic). The parasympathetic fibers are supplied by the vagus, the sympathetic from the cervical and thoracic sympathetic ganglia, and the afferent from both vagus and sympathetic trunk. Of the afferent fibers, those mediating sensations of pain from the heart travel with the sympathetic system, whereas those involved in cardiorespiratory reflexes reach the central nervous system via the vagus. The pain fibers are processes of nerve cells located in the first four thoracic dorsal root ganglia. 6. What nerves supply the heart? Contrast the effects of sympathetic and parasympathetic stimulation of the heart. 6. Cardiac branches of the vagus and the sympathetic trunk. Activation of sympathetic fibers increases the rate and strength of myocardial contraction; parasympathetic stimulation results in a decrease in heart rate and little if any effect on force of contraction. 7. Outline the projection of the heart on the anterior thoracic wall. 7. The right border of the heart extends from the third costal cartilage about a finger's breadth to the right of the sternum to the sixth costal cartilage at the sternocostal junction. The apex lies in the fifth intercostal space in the midclavicular line. The left border of the heart extends from the apex in a curving line to the second intercostal space at the sternocostal junction. 8. Define: Musculi pectinati 8. Muscular bundles making ridges in the inner surface of the auricles. Chordae tendineae Fibrous attachments from papillary muscles to the leaflets of the atrioventricular valves. Moderator band A prominent band of muscle fibers at the apex of the right ventricle which usually carries a branch of the atrioventricular bundle of conduction fibers to the septum; also called the septomarginal trabecula. Trabeculae carneae Bands of muscle fibers on the inner surface of the ventricles. Dissection 20, Pericardium and Heart 9. Page 7 Venae cordis minimae Very small veins which drain blood from the myocardium, opening directly into the right atrium, primarily; also called Thebesian veins or least cardiac veins. Lunule Thin, free margin of aortic and pulmonary valves located on either side of the nodule (thickening). What are the components of the fibrous skeleton of the heart? 10. What is the normal "pacemaker" of the heart? 11. Trace the stimulating impulse of the heart from the pacemaker to the apex of the left ventricle, naming all the components of the conduction system involved. 9. Components of the fibrous skeleton of the heart: mitral valve ring; tricuspid valve ring; aortic valve ring; pulmonary valve ring; right and left fibrous trigones; membranous portion of interventricular septum. 10. The normal pacemaker of the heart is the sinoatrial node. 11. Conduction Pathway: sinoatrial node; muscle of atrium; atrioventricular node; atrioventricular bundle (of His); left bundle branch; Purkinje fibers on surface of left ventricle to apex. 12. Trace the course of sensory fibers from the heart to the central nervous system. Locate the cell bodies of pain fibers supplying the heart. 12. Afferent fibers from the heart primarily mediate sensations of pain. These fibers course to the CNS with the branches of the sympathetic trunk to the heart, involving cardiac (visceral) branches from upper thoracic sympathetic ganglia and white rami of the upper four thoracic nerves. The cell bodies of the pain fibers are in the first four thoracic dorsal root ganglia. 13. Why does a "heart attack" (myocardial infarction) sometimes produce pain along the medial aspect of the arm? 13. This phenomenon involves a poorly understood entity called "referred pain". One explanation of this occurrence calls attention to the fact that afferent fibers from the heart enter the spinal cord at the same level as those from the medial aspect of the arm. Since the visceral afferent fibers from the heart are presumably only rarely active, impulses set up in these fibers are interpreted by the brain as coming from the more commonly active somatic afferent fibers of the arm. See M1159 and H482. 14. What are the histological layers of the cardiac wall? 14. Endocardium, myocardium, epicardium. Dissection 20, Pericardium and Heart Page 8 15. In what layer of the cardiac wall are the coronary arteries and their major branches found? 15. In the epicardium. 16. Do anastomoses normally exist between coronary arteries or their major branches? 16. See H480, M1 Fig. 1.60,p.147 17. Are the cardiac valves heard best by listening directly over their projection on the surface? 17. See H486, M1 171-173. LJ:bh revised 06/18/09